By Marc Sorenson, EdD. Sunlight Institute…
Most of the following Material is excerpted from my upcoming book, Embrace the Sun, which will be available sometime this summer.
The assault on the sun, which has increased in intensity for several decades, is one of the most heinous crimes yet perpetrated on humanity. At the root of this evil is the love of money, as is the case in most instances where large numbers of people are defrauded by business entities in collusion with government and “education.” When these forces combine to use half-truths, outright falsehoods and chicanery that destroy health and shorten lives, are they not engaging in high crimes and misdemeanors? What do we call the crime of taking away another’s life? I am opposed to evil in all its forms, including the theft of sun—a theft that diminishes the mental, spiritual and physical advantages sun brings to mankind. The lies perpetuated by supposedly professional organizations make me ill.
I do not oppose making money in an honest manner. The desire for money, and therefore for a better life, is one of the engines that drives entrepreneurship and leads to the marvelous technologies that we enjoy. But money that derives from lying to the people indicates that evil is at play. When a business finds that one of its products (or messages) is causing harm that could literally lead to disease and death, its first act should be to inform its customers and distributors, and then it should remove the product or message from the market. Regrettably, cover-ups and arguments against such findings are often the norm. The first thought is not “We must warn the people that our product or message is harmful,” but rather, “We must do damage control so that our cash flow is not interrupted.” Indeed, if the product is being unjustly maligned, a vigorous campaign against such malignity should be undertaken; but if the complaint against the product is just, then honesty in correcting the problem or eliminating the product should be the first step.
As regards the sun, it has been assailed from many sides as being the plague of mankind—a devastating scourge that is resulting in a plethora of skin diseases—especially melanoma, that threaten to destroy life on Earth. And despite voluminous research to the contrary, the mantra of those who market sunscreens and (most) of those who treat melanoma remains, “Cover up, avoid sun exposure and never forget to use your sunscreens.” Accordingly, the blood is on their hands; they have a billion-dollar business to support, and the facts be damned.
The anti-sun organizations such as the American Academy of Dermatology (AAD) and the Skin Cancer Foundation (SCF) have been spreading a false message for decades. Their pundits have claimed that the sun is public health enemy number 1 and should be avoided at all costs. They have raised the alarm that melanoma would become the scourge of mankind unless steps were taken to remove the presence of sun exposure from human existence.
Perhaps you will believe that the above statement is outlandish hyperbole. But consider two statements by Wilma Bergfeld, a former president of the AAD, in 1996:
- Melanoma will be the leading cause of cancer death among Americans by 2012.
- Mankind will need to move underground to survive the hazards of sun exposure, namely melanoma.
If you would like to hear the words that emanated from her mouth, view the short video below.
How could anyone believe the propaganda promulgated by Dr. Bergfeld, which is still being pushed by the AAD? Nevertheless, the drumbeat to avoid the sun is having its impact, as death, disease and destruction follows in the wake of its “education” programs.
Let’s consider some truths regarding sun exposure and melanoma.
The Melanoma International Foundation (MIF) states that ultraviolet radiation (UVR) from sun causes melanoma and should be avoided as a detriment to human health.[1] That message is primarily disseminated by (some) dermatologists and their governing bodies (previously discussed), which conveniently ignore the hundreds of scientific investigations associating sun exposure to profoundly better health. The sun performs its miracles by reducing risk for such maladies as breast and prostate cancer, heart disease, osteoporosis and scores of others. The MIF message does not differentiate between strong, intermittent exposure, which can lead to sunburn, and regular, non-burning exposure, such as that received by those who routinely work and recreate outdoors. As you will shortly read, the latter are protected against melanoma.
Concomitantly, a message that opposes the MIF statement is rapidly emerging: sun avoidance, by reducing the body’s production of vitamin D and other beneficial photoproducts, is responsible for a dramatic increase in both degenerative and communicable diseases.[2] In addition, a third view is drawing adherents: that the increase in melanoma incidence is an illusion and an artifact produced by incorrect assessment: the misdiagnosis of benign skin lesions as melanoma.[3]
Nevertheless, melanoma is nothing to trifle with, and any unusual skin lesion should be immediately assessed by a dermatologist. However, since many lesions are benign, yet may nonetheless be misdiagnosed as melanoma, it is a good idea to seek multiple opinions before an excision is performed. Proceeding through a deep and invasive surgery for a harmless lesion is something no one should experience, and the most harmful part of the surgery may be the needless fear that one could have died from a deadly cancer—a cancer that really never existed.
Melanoma accounts for about 9,940 cancer deaths per year in the U.S., making up only a small portion of the total number of cancer deaths per year in the US, estimated to be 589,430.[4] Interestingly, melanoma is most common among men over 50,[5] which makes one wonder why tanning beds are being targeted for extinction by the dermatological societies. Men over 50 hardly fit the demographic that use tanning beds! That demographic is young women. Already we begin to see that there is deception within the organizations that promote sun avoidance; the mantra continues to be that we are killing our young women with tanning-bed use and sun exposure. Does no one care for the 50-year-old men who are dying from melanoma and do not use tanning beds? Does anyone even mention that there are more than twice as many men as women who die from melanoma?[6]
It has been ingrained into the consciousness of educated people throughout the world that the ultraviolet portion of sun radiation (UVR) is the cause of melanoma. The world population, however, as it “progresses,” spends increasingly less time exposed to direct sun. This is due to (1) an increase in indoor activities and decrease in outdoor activities, and (2) the increased use of sunscreens to prevent UVR exposure when outdoors. Nevertheless, the rate of melanoma is believed to be increasing at an alarming pace, as evinced by the aforementioned statement by the MIF, who also stated in 2007 that “melanoma is epidemic: rising faster than any other cancer and projected to affect one person in 50 by 2010, currently it affects 1 in 75. In 1935, only one in 1,500 was struck by the disease.”[7] That is correct; the American Cancer Society in 2014 reported that one in 50 now contracts the disease.[8] The MIF, then, if one assesses the statistics reported by medical organizations, was accurate regarding the increase in melanoma. However, they were wrong, perhaps “dead wrong” in stating that the sun is at fault.
Let’s take another look at the mathematics. According to the MIF, people had about 30 times the risk of contracting melanoma in 2010-2014 as in 1935, or stated in another way, a 3,000% risk increase. One might surmise that sun exposure must have increased spectacularly, during the time frame discussed, to have caused the exponential increase in melanoma, assuming that the statement by the MIF—that melanoma is caused by sun exposure—is correct. But is that statement correct?
Let’s ask six pertinent questions.
Question 1. Has sun exposure increased as melanoma has increased?
If melanoma has indeed increased exponentially since 1935, and if that increase is due to sun exposure, then sun exposure must also have shown a parallel or at least significant increase during that time. To determine the veracity of that idea, I analyzed data from the Office of Occupational Statistics and Employment Projections, Bureau of Labor Statistics (BLS), to determine if there was an increase or a decrease in human sun exposure during the years from 1910 to 2,000.[9] I closely considered changes since 1935, the year the MIF used as a baseline for measuring increases in melanoma incidence.
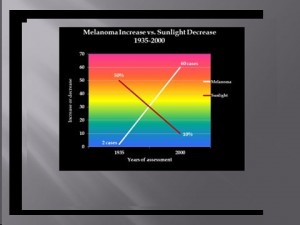
The data from the BLS showed that indoor occupations such as “professional, managerial, clerical, sales, and service workers (except private household service workers) grew from one-quarter to three-quarters of total employment between 1910 and 2000.” The BLS also stated that during the same period, the outdoor occupation of farming declined from 33% to 1.2% of total employment, a 96% reduction. The data also show that approximately 66% of the decline in the occupation of farmers and 50% of the decline in the occupation of farm laborers occurred after 1935. Further information, this time from the Environmental Protection Agency (EPA) determined that as of 1986, about 5 percent of adult men worked mostly outside, and that about 10 percent worked outside part of the time. The proportion of women who worked outside was thought to be even lower.[10] These data demonstrate a dramatic shift from outdoor, sun-exposed activity to indoor, non-sun-exposed activity during the mid-to-late 20th Century. This change, nonetheless, has been accompanied by a 30-times increase in melanoma risk since 1935, the MIF-baseline year. Accordingly, if sun exposure is really responsible for the pandemic of melanoma, it has achieved that dubious distinction during a time of profound decrease in sun exposure! To me, this is wholly counterintuitive. The data just presented really suggest that sun exposure is not responsible for the increase in melanoma, and we submit instead, that the profound decrease in sun exposure may be a factor in the purported exponential melanoma increase. That concept is illustrated graphically below.
Although it has been theorized that decreasing thickness of the ozone layer may be responsible for the increasing incidence of melanoma, research by Moan and Dahlback in Norway reported that yearly melanoma incidence increased 350% in men and 440% in women between 1957 and 1984—a period when there was absolutely no thinning of the ozone layer.[11]
The answer to question 1 is no; sun exposure has not increased as melanoma has increased. Exactly the opposite has occurred.
Question 2. Do outdoor workers have a higher incidence of melanoma than indoor workers?
If melanoma is increasing due to increased sun exposure, it is clear that outdoor workers, being exposed to far higher quantities of sun, would also have a far higher incidence of melanoma. Nevertheless, Dianne Godar and colleagues[12] presented evidence that outdoor workers, while receiving 3-9 times the sun exposure as indoor workers have had no increase in melanoma since before 1940, whereas melanoma incidence in indoor workers has increased steadily and exponentially.[13] [14]
Godar and colleagues also published irrefutable evidence of the protective influence of sun against melanoma in a landmark study in 2015,[15] entitled Dramatic Increases in Melanoma Correlate to Low Annual Sun exposure in Europe.
Published in the scientific journal Dermato-Endocrinology, the paper makes some very interesting comments, all based on excellent research:
- Melanoma has steadily increased in fair-skinned indoor working people around the world. Increasing melanoma incidence significantly correlates with decreasing personal annual UV doses [emphasis ours]. (UV or ultraviolet radiation is the spectrum of sun that stimulates the skin to produce vitamin D3.)
- People are more susceptible to melanoma when they have larger numbers of moles, light skin and hair, and poor tanning ability.
- There is a paradox between indoor and outdoor workers’ melanoma incidences and their annual UV (ultraviolet light) exposure. Outdoor workers receive 3-9 times the annual UV doses that indoor worker receive, but have only 50% of the risk for contracting melanoma.
- Although most scientists believe that intermittent UV exposures—resulting in sunburns—initiate melanoma, the creation and use of sunscreens DID NOT [emphasis ours] reduce the incidence of the disease. One of the reasons may be that sunscreens dramatically reduce vitamin D synthesis in the skin.
- Sunburns are probably not [emphasis mine] involved in the initiation or growth of melanoma, since a study on opossums showed that intense sun doses of UVB produced significantly fewer melanomas than sub-erythemal (non reddening) doses. Also, outdoor workers do get numerous sunburns but still have dramatically lower risk of contracting melanoma. [I do not advocate sunburning; although it may not cause melanoma, it will certainly do some damage to skin.]
- Many melanomas occur on areas of the body where the sun never shines.
The authors go on to theorize that a lower level of vitamin D, among those who receive inadequate sun, could be a major reason for the exponential increase of melanoma in European countries where the UV (sun) exposure is minimal. Another reason they suggest is infection with human papilloma virus (HPV).
Whatever the theories propose, regarding the cause of high melanoma incidence accompanying low sun or UV exposure, the equation remains the same: FOR THE VAST MAJORITY OF THE POPULATION, THE GREATER THE REGULAR EXPOSURE TO SUN, THE LESS THE RISK OF MELANOMA. Nevertheless, such information sells neither sunscreens nor melanoma surgeries, so don’t stand on one leg until the public believes the truth. However, you can learn the facts and become a soldier in the “sun army” by promoting the evidence.
Other research corroborates the idea that outdoor workers experience less melanoma than indoor workers.[16] Vagero, et al.[17] showed that melanoma was more common among indoor office workers and other indoor workers than among outdoor workers, and Kennedy, et al.[18] showed that a lifetime of sun exposure correlated to a reduced risk of melanoma. Garland, et al.[19] showed that those who worked indoors had a 50% greater risk of melanoma than those who worked both indoors and outdoors, and Kaskel, et al.[20] demonstrated that children who engage in outdoor activities are less likely to develop melanoma than those who do not. Many other papers in the scientific literature show that both incidence and death rate from melanoma are reduced with increasing exposure to sun.[21] [22] [23] [24] [25] [26] [27] [28] [29] [30] [31] [32]
None of these findings is surprising when one considers that whereas common, non-melanoma skin cancers are easily produced in experiments using ultraviolet radiation (UVR) from sunlamps, the same is not true for melanoma, which is difficult to produce with UVR.[33]
Finally, from 2016, research reported in the journal Anticancer Research demonstrated that UVR exposure was inversely associated with melanoma.[34] The researchers had set out to study whether the annual UVR level, estimated on a county level, was associated with incidence rates of oral, pharyngeal, and cervical cancers and melanoma. They found that all of these cancers were inversely associated with sun exposure. Interestingly, the authors, in their introduction to the research, said that UVR exposure is a well-demonstrated risk factor for melanoma. Then, at the end of their paper, they made this statement: “Our findings are in agreement with several other published studies reporting no positive correlation between UVR exposure and the incidence rates of oral, pharyngeal, and cervical cancer and melanoma.” Those two statements are contradictory, but their conclusion was correct: Those cancers are inversely correlated to UVR. Do you believe that the anti-sun organizations will admit their errors and embrace the sun? Don’t bet your bank account on it!
This data indicate again that sun exposure is not responsible for the increase in melanoma, and that the decrease in sun exposure may be a factor in the reported dramatic melanoma increase.
The answer to question 2 is no; outdoor workers do not have a higher incidence of melanoma than indoor workers.
Question 3. Do many melanomas occur on areas of the body that receive little sun exposure?
If sun exposure is the reason for the increase in melanoma, then it would be reasonable to expect that areas of the body that receive the most exposure, would also be the areas of greatest occurrence of the disease. This is not the case. The research by Garland and colleagues al.,[35] when assessing the incidence of melanoma occurring at various sites, found higher rates on the trunk (seldom exposed to sun) than on the head and arms (commonly exposed to sun). Others have shown that melanoma in women occur primarily on the upper legs, and in men more frequently on the back—areas of little sun exposure.[36] In blacks, melanoma is more common on the soles of the feet and on the lower legs.[37] Based on this data, it would be difficult to make the case that sun exposure is responsible for the increase in melanoma.
It should be mentioned that it is believed that intermittent bursts of intense sun (that causes sunburn) increases the risk of melanoma, whereas regular exposure reduces the risk[38] and that even on chronically sun-damaged skin, the mutations that lead to melanoma are rare.[39] Even the idea that sunburn causes melanoma is inconsistent with the fact that most melanomas do not occur at burn sites.[40] [41] The paper by Godar[42]put forth the hypothesis that lack of sun reduces the quantity of vitamin D in the skin, and then cited research showing that the potent hormone form of vitamin D, calcitriol, reduced the incidence, size and number of skin tumors and also reduced invasiveness and metastasis of melanoma in mice. Since regular sun exposure correlates to higher vitamin D production and higher levels in the blood, this evidence is plausible and would explain the reasons for reduced melanoma rates among those who are regularly exposed to sun.
Since many melanomas occur on areas of the body that receive little sun exposure, the indication is that sun exposure is not the cause of melanoma.
The answer to question 3 is yes, many melanomas occur on areas of the body that receive little sun exposure.
Question 4. Is there a co-morbidity of melanoma with common skin cancers, some of which are known to be associated to high sun exposure?
There is general agreement that sun exposure is one of the causal factors for squamous cell and basal cell carcinoma, also known as non-melanoma skin cancer (NMSC). However, these cancers do not demonstrate co-morbidity with melanoma.[43] [44] [45] Dr. Grant, after analyzing data from the Atlas of Cancer Mortality in the United States, noted that between 1950-1969 and 1970-1994, death rates from NMSC decreased by 31% for white males and by 47% for white females. However, during those same periods, melanoma death rates increased by 89% in white males and 42% for white females.[46]If one accepts the rate of NMSC as a measure of the cumulative exposure to sun, it is reasonable to conclude that sun exposure correlates to a reduced risk of melanoma, and that the lack of exposure increases the risk of melanoma.
This is another indication that sun exposure is not responsible for the increase in melanoma.
The answer to question 4 is no; there a no co-morbidity of melanoma with common skin cancers, some of which are known to be associated to high sun exposure.
Question 5. Has an increase in sunscreen use resulted in a decrease in melanoma?
Sunscreens block sun, and they are intended to decrease sun damage to the skin—damage that is said to increase the risk of melanoma. Sunscreen use has increased considerably in the past few decades. Therefore, if sun exposure is the cause of melanoma—as stated by the IMF—there should be a simultaneous decrease in melanoma as sunscreen use has increased. According to Kline & Company, a research group, sales of sunscreens in 1972 were $33 million; in 2008, sales were $650 million.[47] In addition, according to the Fredonia Market Research Group Company, the sales of sunscreens used in cosmetics in 2007 was $130 million.[48] Therefore, the total sales of sunscreens as of 2007 were $780 million. Considering that a dollar’s value is only about 20% of what it was in 1972, the adjusted 2008 sunscreen expenditures are approximately $156 million, or about 4.7 times the 1972 figure. In other words, sunscreen use has increased by about 4.7 times. Population also grew from 210 million in 1972 to 305 million in 2008–a 50% increase. Adjusting for population growth, it can be concluded that per capita sunscreen use has at least tripled in the time frame being considered.
As previously discussed, melanoma, according to the MIF, has increased steadily and exponentially since 1935. Therefore, the data on increasing sunscreen use does not indicate that sun exposure increases the risk of melanoma. Rather, it indicates that sunscreen use may, by reducing vitamin D production, contribute to the reported increase in melanoma. It has been shown that an SPF 15 sunscreen will decrease sun-stimulated vitamin D production by 99.5%, [49]and it has been suggested that by blocking only UVB light (which stimulates the production of vitamin D in skin) while leaving UVA unblocked, sunscreens ironically may lead to UVA damage of DNA, leading to melanoma.[50] [51] Increasing melanoma rates, coupled with increasing use of sunscreen, lends credence to that hypothesis. Regular sun exposure, therefore, does not increase risk of melanoma.
The answer to question 5 is no; increase in sunscreen use has not resulted in a decrease in melanoma.
Now let’s ask one more very important question:
Question 6. Is it possible that the reported pandemic of melanoma is not a pandemic at all, but that the “increase” in melanoma” is due to excessive diagnosis of benign lesions?
Writing in the British Medical Journal in 2008, Dr. Sam Shuster, a dermatologist, argued that the purported increase in melanoma is not really an increase, but an artifact due to non-melanoma lesions being misdiagnosed as melanoma.[52] In 2009, another study by dermatologists— Shuster and his colleagues—this time published by the British Journal of Dermatology, came to a similar conclusion and called the “increase” in melanoma a “midsummer night’s dream.”[53] They concluded, after tracking the reported increase in melanoma in the Eastern region of the UK between 1991 and 2004, that benign lesions were being classified in increasing numbers as stage-one melanoma. No other stages of the disease increased, and the increase in mortality due to melanoma was either miniscule or non-existent. This was true even though all grades of tumors were diagnosed at first presentation. They also noted that “the distribution of the lesions reported did not correspond to the sites of lesions caused by solar exposure,” a finding similar to that discussed in heading #3 above. These dermatologists concluded that “the large increase in reported incidence is likely to be due to diagnostic drift which classifies benign lesions as stage 1 melanoma.” They further stated that “These findings inevitably challenge the validity of epidemiology studies linking increasing melanoma incidence with UV radiation and suggest the need for a search for other ways in which the disease may be caused.”
Another celebrated dermatologist, Dr. A Bernard Ackerman, has written a monograph entitled Sun and the “Epidemic” of Melanoma: Myth on Myth.[54] In it he reviews extensive research and concludes that melanoma has nothing to do with sun exposure; and like the authors of the aforementioned BMJ article, he indicates that excessive diagnosis of benign lesions is responsible for the purported epidemic of melanoma.
Stunningly, the American Academy of Dermatology (AAD) published a report showing that most melanoma diagnoses may be incorrect.[55]Approximately 44 different authors contributed to that report. They made an accuracy-in-detection analysis based on the number of melanomas that needed to be excised during a period of ten years, compared to the actual number that were excised. Many clinics in different countries were involved in assessing the numbers.
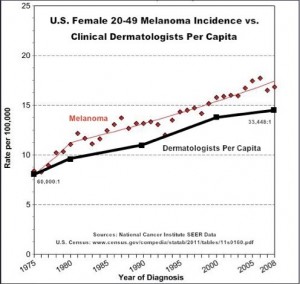
A total of 300,215 cases were found where excision took place. Of those cases, there were 17,172 melanomas that really required excision, and 283,043 that were excised and turned out to be benign lesions. Therefore, there were about 16.5 non-melanoma lesions removed for each lesion that was cancerous, and only about 6% were legitimate cancers. From this information, it is obvious that many melanoma surgeries are bogus and may inflate the incidence of melanoma. The aforementioned Drs. Shuster and Ackerman were correct. Dermatology is a huge business, and considering the spectacular per capita increase in the number of dermatologists, it is no wonder that they want to keep this little gravy train rolling down the track. See the graph below, which illustrates that the increase in the numbers of dermatologists paralleld the increase in the number of melanomas in young women.
It is obvious that the business of removing benign lesions is lucrative for the doctors. As the authors stated in their introduction to their research, “Early excision is the only strategy to reduce melanoma mortality, but unnecessary excision of benign lesions increases morbidity and healthcare costs.” It is hard to believe that the AAD published the report, but I am thankful it was done.
The answer to question 6 is yes. It is possible that the reported pandemic of melanoma is not a pandemic at all, but that the “increase” in melanoma” is due to excessive diagnosis of benign lesions.
The bottom line: From the research thus far presented, it could be concluded that either melanoma is increasing dramatically and is directly correlated to decreasing sun exposure, or that melanoma is not increasing at all, and the “epidemic” of melanoma does not exist. In either case, the statement by the MIF—that sun causes melanoma—has no validity. Stop blaming the sun!
You should have learned the following points from this part of the presentation:
- Sun exposure has decreased profoundly as melanoma has increased remarkably.
- Outdoor workers have a significantly lower incidence of melanoma than indoor workers.
- Many melanomas occur on areas of the body that receive little or no sun exposure.
- There a no co-morbidity of melanoma with common skin cancers, some of which are known to be associated to high sun exposure.
- An increase in sunscreen has been associated with an increase in melanoma incidence.
- It is possible that the “epidemic” of melanoma is not an epidemic at all, but that the “increase” in melanoma is due to excessive diagnosis of benign non-melanoma lesions.
- The idea that regular sun exposure leads to melanoma is counterintuitive.
- These facts should be presented to everyone who defames the sun as a carcinogen (cancer causer) for melanoma.
Stay tuned for more posts on this subject.
[1]Melanoma International Foundation, 2007 Facts about melanoma. Sources: National Cancer Institute 2007 SEER Database, American Cancer Society’s 2007 Facts and Figures, the Skin Cancer Foundation, the American Academy of Dermatology.
[2]Grant, W. In defense of the sun: An estimate of changes in mortality rates in the United States if mean serum 25-hydroxyvitamin D levels were raised to 45 ng/mL by solar ultraviolet-B irradiance. Dermato-endocrinology 2009;4:207-214.
[3]N.J. Levell, C.C. Beattie, S. Shuster and D.C. Greenberg. Melanoma epidemic: a midsummer night’s dream? British J Dermatol 2009;161:630–34
[4]Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015.CA Cancer J Clin. 2015 Jan-Feb;65(1):5-29.
[5] Melanoma Research Foundation. Melanoma Fact Sheet. Accessed 9-15-2014 at http://melanomainternational.org/melanoma-facts/#.VCHCG1_ANE0
[6] American Cancer Society. Cancer Facts & Figures 2015
[7] Melanoma Research Foundation. Melanoma Fact Sheet. Accessed 9-15-2014 at http://melanomainternational.org/melanoma-facts/#.VCHCG1_ANE0
[8] American Cancer Society. Melanoma Skin Cancer Overview 9/16/2014. http://www.cancer.org/cancer/skincancer-melanoma/overviewguide/melanoma-skin-cancer-overview-key-statistics
[9] Ian D. Wyatt and Daniel E. Hecker. Occupational changes in the 20th century. Monthly Labor Review, March 2006 pp 35-57: Office of Occupational Statistics and Employment Projections, Bureau of Labor Statistics
[10] U.S. Congress, Office of Technology Assessment, Catching Our Breath: Next Steps for Reducing Urban Ozone, OTA-O-412 (Washington, DC: U.S. Government Printing Office, July 1989).
[11] J. Moan and A. Dahlback. The relationship between skin cancers, solar radiation and ozone depletion. Br J Cancer 1992; 65: 916–21
[12] Godar D, Landry, R, Lucas, A. Increased UVA exposures and decreased cutaneous Vitamin D3 levels may be responsible for the increasing incidence of melanoma. Med Hypotheses 2009;72(4):434-43.
[13] Godar D. UV doses worldwide. Photochem Photobiol 2005;81:736–49.
[14] Thieden E, Philipsen PA, Sandby-Møller J, Wulf HC. UV radiation exposure related to age, sex, occupation, and sun behavior based on time-stamped personal dosimeter readings. Arch Dermatol 2004;140:197–203.
[15] Stephen J Merrill, Samira Ashrafi, Madhan Subramanian & Dianne E Godar. Exponentially increasing incidences of cutaneous malignant melanoma in Europe correlate with low personal annual UV doses and suggests 2 major risk Factors. Dermato-endocrinology 2015;7:1
[16] Lee J. Melanoma and exposure to sun. Epidemiol Rev 1982;4:110–36.
[17] Vågero D, Ringbäck G, Kiviranta H. Melanoma and other tumors of the skin among office, other indoor and outdoor workers in Sweden 1961–1979 Brit J Cancer 1986;53:507–12.
[18] Kennedy C, Bajdik CD, Willemze R, De Gruijl FR, Bouwes Bavinck JN; Leiden Skin Cancer Study. The influence of painful sunburns and lifetime sun exposure on the risk of actinic keratoses, seborrheic warts, melanocytic nevi, atypical nevi, and skin cancer. Invest Dermatol 2003;120:1087–93.
[19] Garland FC, White MR, Garland CF, Shaw E, Gorham ED. Occupational sun exposure and melanoma in the USA Navy. Arch Environ Health 1990; 45:261-67.
[20] Kaskel P, Sander S, Kron M, Kind P, Peter RU, Krähn G. Outdoor activities in childhood: a protective factor for cutaneous melanoma? Results of a case-control study in 271 matched pairs. Br J Dermatol 2001;145:602-09.
[21]Garsaud P, Boisseau-Garsaud AM, Ossondo M, Azaloux H, Escanmant P, Le Mab G. Epidemiology of cutaneous melanoma in the French West Indies (Martinique). Am J Epidemiol 1998;147:66-8.
[22]Le Marchand l, Saltzman S, Hankin JH, Wilkens LR, Franke SJM, Kolonel N. Sun exposure, diet and melanoma in Hawaii Caucasians. Am J Epidemiol 2006;164:232-45.
[23]Armstong K, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Biol 2001;63:8-18
[24]Crombie IK. Distribution of malignant melanoma on the body surface. Br J Cancer 1981;43:842-9.
[25]Crombie IK. Variation of melanoma incidence with latitude in North America and Europe. Br J Cancer 1979;40:774-81.
[26]Weinstock MA, Colditz,BA, Willett WC, Stampfer MJ. Bronstein, BR, Speizer FE. Nonfamilial cutaneous melanoma incidence in women associated with sun exposure before 20 years of age. Pediatrics 1989;84:199-204.
[27]Tucker MA, Goldstein AM. Melanoma etiology: where are we? Oncogene 2003;22:3042-52.
[28]Berwick M, Armstrong BK, Ben-Porat L, Fine J, Kricker A, Eberle C. Sun exposure and mortality from melanoma. J Nat Cancer Inst 2005;97:95-199.
[29]Veierød MB, Weiderpass E, Thörn M, Hansson J, Lund E, Armstrong B. A prospective study of pigmentation, sun exposure, and risk of cutaneous malignant melanoma in women. J Natl Cancer Inst 2003;95:1530-8.
[30]Oliveria S, Saraiya M, Geller A, Heneghan M, Jorgensen C. Sun exposure and risk of melanoma. Arch Dis Child 2006;91:131-8.
[31]Elwood JM, Gallagher RP, Hill GB, Pearson JCG. Cutaneous melanoma in relation to intermittent and constant sun exposure—the western Canada melanoma study. Int J Cancer 2006;35:427-33
[32] Grant WB. Role of solar UV irradiance and smoking in cancer as inferred from cancer incidence rates by occupation in Nordic countries. Dermatoendocrinol. 2012;4(2):203-11.
[33]Setlow RB, Woodhead AD, Grist E. Animal model for ultraviolet radiation induced melanoma: platyfish-swordtail hybrid. Proc Natl Acad Sci 1989;86:8922-9026
[34]Adams S, Lin J, Brown D, Shriver CD, Zhu K.Ultraviolet Radiation Exposure and the Incidence of Oral, Pharyngeal and Cervical Cancer and Melanoma: An Analysis of the SEER Data. Anticancer Res. 2016 Jan;36(1):233-7.
[35]Garland FC, White MR, Garland CF, Shaw E, Gorham ED. Occupational sun exposure and melanoma in the USA Navy. Arch Environ Health 1990; 45:261-67.
[36] Rivers, J. Is there more than one road to melanoma? Lancet 2004;363:728-30.
[37] Crombie, I. Racial differences in melanoma incidence. Br J Cancer 1979;40:185-93.
[38] Elwood JM, Gallagher RP, Hill GB, Pearson JCG. Cutaneous melanoma in relation to intermittent and constant sun exposure – The Western Canada melanoma study. Br J Cancer 1985;35:427–33.
[39]Maldonado JL, Fridlyand J, Patel H, Jain AN, Busam K, Kageshita T, Ono T, Albertson DG, Pinkel D, Bastian BC. Determinants of BRAF mutations in primary melanomas. J Natl Cancer Inst 2003 Dec 17;95(24):1878-90.
[40]Shuster, S. Is sun exposure a major cause of melanoma? No. BMJ2008;337:a764
[41]Garsaud P, Boisseau-Garsaud AM, Ossondo M, Azaloux H, Escanmant P, Le Mab G. Epidemiology of cutaneous melanoma in the French West Indies (Martinique). Am J Epidemiol 1998;147:66-8
[42]Godar DE, Landry RJ, Lucas AD. Increased UVA exposures and decreased cutaneous Vitamin D3 levels may be responsible for the increasing incidence of melanoma. Med hypothesis (2009), doi:10.1016/j.mehy.2008.09.056
[43]Grant, W. An ecologic study of cancer mortality rates in Spain with respect to indices of solar UVB irradiance and smoking. Int J Cancer 2007;120:1123-28.
[44] Tuohimaa P, Pukkala E, Scélo G, Olsen JH, Brewster DH, Hemminki K, Tracey E, Weiderpass E, Kliewer EV, Pompe-Kirn V, McBride ML, Martos C, Chia KS, Tonita JM, Jonasson JG, Boffetta P, Brennan P. Does solar exposure as indicated by the non-melanoma skin cancers protect from solid cancers? Vitamin D as a possible explanation. Eur J Cancer 2007;43:1701-12.
[45]Grant, W. Solar ultraviolet irradiance and cancer incidence and mortality. Chapter 2. Edited by JorgReichrath, Landes Bioscience 2007.
[46]Grant, W. Solar ultraviolet irradiance and cancer incidence and mortality. Chapter 2. Edited by JorgReichrath, Landes Bioscience 2007.
[47] Kline & Company’s Cosmetics & Toiletries USA Annual Service (1972 and 2008 editions).
[48] Fredonia market research group report, 2009.
[49] Matsuoka LY, Ide L, Wortsman J, MacLaughlin JA, Holick MF. Sunscreens suppress cutaneous vitamin D3 synthesis. Journal of Clinical Endocrinology & Metabolism 1987; 64:1165-68.
[50] Garland CF, Garland FC, Gorham ED. Could sunscreens increase melanoma risk? Am J Public Health 1992;82(4):614-5.
[51] Garland CF, Garland FC, Gorham ED. Rising trends in melanoma. An hypothesis concerning sunscreen effectiveness. Ann Epidemiol 1993 Jan;3(1):103-10.
[52] Shuster, S. Is sun exposure a major cause of melanoma? No. BMJ2008;337:a764
[53] N.J. Levell, C.C. Beattie, S. Shuster and D.C. Greenberg. Melanoma epidemic: a midsummer night’s dream? British J Dermatol 2009;161:630–34
[54] Ackerman, B. The Sun and the “Epidemic” of Melanoma: Myth on Myth. 2008.
[55]ArgenzianoG1, Cerroni L, Zalaudek I, Staibano S, Hofmann-Wellenhof R, et al. Accuracy in melanoma detection: a 10-year multicenter survey.J Am Acad Dermatol. 2012 Jul;67(1):54-9.

Hello, what is your opinion about the number of moles and melanoma relationship? Thank you
Hi John,
A large number of moles is the # 1 predictor of melanoma, regardless of sun exposure. Habitual sun exposure, of course is a protector against melanoma.
Marc