Major factors for Covid-19. By Marc Sorenson, EdD
Major factors in Covid-19 and death go far beyond age, lung disease, obesity and heart disease. Two newer studies show that diabetes and Parkinson’s disease are also associated with death among Covid-19 patients. Although scientists commonly accept diabetes as a risk factor for death from Covid, the Parkinson’s information is new and surprising. The Parkinson’s study involved 80,000 patients and the University of Iowa Health Care Center. It showed that Parkinson’s patients with Covid-19 had a 30% greater risk of mortality (death) due to Covid. Of course, that was when compared to patients who did not have Parkinson’s disease. Thus, the researchers found 5.5% (4,290 of 78,355) of Covid-19 patients without Parkinson’s disease died compared to 21.3% patients with Parkinson’s disease.
What is the answer to preventing Parkinson’s disease and therefore reducing the risk of death from Covid-19?
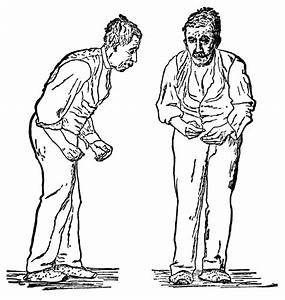
First, the answer is not a drug. Rather, the answer is sun exposure. Parkinson’s is a neurologic disease caused by brain cell deterioration, which decreases dopamine and other major factors. Thus, it results in tremors, (especially of the hands) muscle rigidity, shuffling gait and slow speech. It also closely associates with depression, bipolar disorder and chronic fatigue, and that is not surprising, considering the physical and mental difficulty involved. Sufficient dopamine is essential to proper brain function.
Parkinson’s patients do not have sufficient dopamine. In addition, they have far too little BDNF.
That chemical is brain-derived neurotropic factor (BDNF). It is another major factor, because it helps to promote the survival of dopamine neurons. It is especially relevant that exercise tends to increase BDNF. Another major factor in Parkinson’s is serotonin, the body’s major natural “upper” and a major factor in depression. Finally, depression itself is a major factor in Parkinson’s.
So how does sun deprivation become one of the major factors in the link between Parkinson’s and Covid-19?
Greater amounts of dopamine, serotonin, endorphin and brain-derived neurotropic factor (BDNF) associate with regular sun exposure. Depression also inversely associates with sun exposure. In addition, the onset of bipolar disorder associates with increased hours of daylight at the birth location. If these things were true, we would expect a lower risk of Parkinson’s disease to accompany regular sun exposure. Thus it is. A meta-analysis from Medical Science Monitor showed that people with high sun exposure levels had only 1/50 the risk of contracting Parkinson’s!
An incredible association between sun exposure and Parkinson’s
High sun exposure associates so closely with low risk of Parkinson’s disease that it practically eliminates it. It also associates very closely to the aforementioned major factors for Parkinson’s disease listed above. In addition, we have established that having Parkinson’s increases the death risk from Covid -19 by 30%. It seems like common sense that sunlight would also have a protective effect on Covid-19.
The bottom line regarding major factors for reducing Parkinson’s and Covid-19.
Sun exposure, therefore, is one of the major factors in reducing risk of Parkinson’s, and Parkinson’s is a major factor in death from Covid-19. Do not neglect regular, non-burning sun exposure.
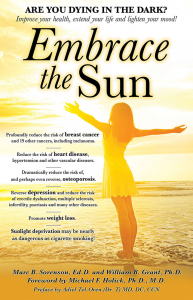
For more information on Covid 19, Parkinson’s disease and related causes, visit https://sunlightinstitute.org/ and read the book, Embrace the Sun.
Mental illness: Vitamin D deficiency, and thereby sunlight deficiency, plays a major role. By Marc Sorenson, EdD.
Mental illness is a pandemic in the United States. Nearly one in five U.S. adults live with a mental illness (46.6 million in 2017). Mental illness has multiple causes and manifestations. It is especially relevant to understand that sunlight deprivation, leading to vitamin D deficiency, plays a major role in this disorder. It is also important to realize that sun exposure, for typical people, produces about 90% of serum (blood) vitamin D. In addition, this production occurs when midday sunlight touches the skin. However, vitamin D is only one of several photoproducts produced by sun exposure to skin or other body parts. In addition, sun exposure produces serotonin, endorphin, dopamine, and brain-derived neurotropic factor (BDNF). Furthermore, all of these vital chemicals has a profound influence on mental Illness.
An important study on vitamin D
The disease is ubiquitous, as is sun deprivation. Thus, thus an investigation on vitamin D and mental illness reminded me of the affects of sunlight. This laboratory-based study found a high prevalence of vitamin D deficiency among 290 patients with mental illness. Consequently, Only 18% of these patients showed adequate levels of vitamin D. To me, this also means that only 18% were obtaining sufficient sun exposure for good mental health and well-being. The researchers concluded that sensible sun exposure could be a boon to mental health.
Let us now discuss a few of the disorders classified as types of mental illness. Then we will also mention the research that indicates an impressive salutary influence of sun exposure.
ADHD, a mental illness of children
ADHD ( attention deficit hyperactivity disorder) is the most prevalent of all mental disorders in children. Hence, it causes significant problems with executive functions, leading to hyperactivity or impulsiveness not appropriate for the person’s age.
Researchers have found that sun exposure correlates to a decreased risk of ADHD. They assessed the relationship between the prevalence of ADHD and the intensity of the sun in various nations and in US states. And after adjusting for birth weights, infant mortality and other relevant factors, the findings were not altered. It was obvious that sun deprivation by itself was associated with a higher risk of ADHD.
Autism, another disease of youth
Is autism a sun-deficiency disorder? Autism rates are increasing exponentially and associate to vitamin D deficiency, which, of course, associates to sun deficiency. The Autism Society of America defines autism as “a complex developmental disability typically appearing during the first three years of life and is the result of a neurological disorder affecting the normal functioning of the brain, impacting development in the areas of social interaction and communication skills. Both children and adults with autism typically show difficulties in verbal and non-verbal communication, social interactions, and leisure or play activities.”
If vitamin D deficiency and/or sun deprivation relates to autism, symptoms should improve in summer. Thus, a case study reported by Dr. Cannell revealed improvements in autism-related sleep and behavioral problems during summer. Autistic traits such as crying, excitability, hyperactivity and pounding objects profoundly diminished during summer.
Bipolar Disorder
Bipolar disorder (BPD), also known as manic-depressive illness, is a brain disorder causing unusual shifts in mood, energy, activity levels, and the ability to perform day-to-day tasks. Symptoms are severe and can result in damaged relationships, poor job or school performance and even suicide.https://www.nimh.nih.gov/health/topics/bipolar-disorder/index.shtm
Sun exposure resets the body’s circadian rhythms, which are variations in physiology and behavior persistent with a cycle length close to 24 hours. This system is contained in the hypothalamus and stimulated by nerve cells in the retina of the eye in response to light. Research indicates that environmental conditions early in life may imprint the circadian system and influence mental function later in life: Increased number of hours of daylight at the location of birth during the first three months of life are associated with a significantly older age of onset of bipolar disorder. For a longer discussion on bipolar disorder, read the book, Embrace the Sun.
Cognitive disabilities (intellectual disorders)
Another research study, based on a 15-year residential history of varying degrees of sun exposure, produced an interesting result. It showed that cognitive impairment in persons who were below the median exposure to sunlight was 88% greater than in those who were above the median. These same investigators had previously shown that lower levels of sun exposure resulted in a 2.6-times higher incidence of cognitive impairment. Therefore, if you want to think clearly and keep your marbles, regularly soak up some non-burning sunlight.
Depression
Few people realize how prevalent depression is in our society, a mental illness representing a huge drain on the economy. Moreover, according to Steven Genuis, in an editorial in Canadian Family Physician, “The World Health Organization estimates depression costs the American economy about $44 billion annually, equal to the total cost of all cardiovascular diseases.” He also stated that in one decade, there was a 300% increase in the sales of antidepressants, making these medications the top-selling pharmaceuticals in the world. (Genuis, S. Keeping your sunny side up (editorial). Canadian Family Physician 2006:52:42-43.)
So what does the sun do to relieve “the blues?”
The answer probably lies in a chemical responsible for transmitting impulses between nerve cells. This “neurotransmitter,” serotonin, is a natural “upper,” and works in synchronization with the natural “downer,” melatonin. When we awake to sunshine, light enters the eye and stimulates serotonin production. We then quickly become awake and invigorated, and melatonin diminishes. Nevertheless, at day’s end, the bright light disappears (or at least it should), melatonin levels rise, and serotonin levels diminish. We begin to feel sleepy and ideally retire for a good night’s rest. It is a perfect system for our needs—unless we stay up beyond biologically natural hours, by using artificial lighting. Many experts believe that lack of serotonin is a cause of depression.
The most important study on serotonin
Though I mentioned this study in my previous blog on sunlight and depression, it bears repeating here. Dr. Gavin Lambert performed one of the most important and unique studies on serotonin. He and his colleagues measured serotonin levels in response to varying degrees of sunlight. First of all, they drew blood samples from the internal jugular veins of 101 men. In addition, they compared the serotonin concentrations of the blood to weather conditions and seasons. As a result, men measured on a bright day produced eight times more serotonin, than those measured on a dismal day. Of course, the mood improved due to sunlight, with no involvement whatsoever of vitamin D. Thus, regular, non-burning sun exposure is the answer to depression. In addition, remember that sun exposure also leads to the production of other mood enhancers such as nitric oxide, endorphin and dopamine.
Certainly, sunlight deprivation is not the only cause of mental illness, but it is one of the most important.
There are more mental illnesses to discuss, and I will expatiate on those in a future article. In the meantime, protect your mental health by being sure to obtain your share of non-burning sunlight. For more information, visit sunlightinstitute.org, and read the book, Embrace the Sun.
Depression, vitamin D and sunlight. Which is more important? By Marc Sorenson, EdD
Depression is a national horror made worse by fear, worry and lack of sunlight. The Covid-19 pandemic and the tendency to lock people away from sunlight and fresh air has taken an enormous toll.
Depression is more likely to respond to sunlight and vitamin D than sedentary living. That is the message I derived from a recent study. First, the purpose of the research was to estimate cumulative vitamin D doses in 96 depressed patients. These vitamin D doses came from two different sources: solar ultraviolet light, and dietary intake. Another part of the research was to compare vitamin D doses of these depressed patients to 96 age- and sex-matched healthy (non-depressed) controls.
Here are the “Enlightening” results and conclusions.
According to the researchers, there was the major (and probably unexpected) finding. Those with depression had significantly lower vitamin D doses compared to age- and sex-matched healthy controls. Thus, the research again proves the efficacy of sunlight (and possibly vitamin D) for reducing depression. Nevertheless, there was a more important conclusion as stated by the investigators. “While dietary intakes of vitamin D were equal in both groups, patients with depression appeared to have statistically significantly less vitamin D from solar ultraviolet B.” This statement is of transcendent importance due to the establishment of an important fact. That fact is that a superior form of vitamin D results from sun exposure.
Other points to remember regarding sunlight and depression.
In addition to this study, numerous other investigations corroborate the efficacy of sun exposure for ameliorating depression. Serotonin is a potent “upper” that improves mood almost immediately. Sunlight produces Serotonin when it enters the eyes.
The most impressive study on serotonin, sunlight and depression.
Dr. Gavin Lambert did one of the most important studies on serotonin. He and his colleagues measured serotonin levels in response to varying degrees of sunlight. To do so, they drew blood samples from the internal jugular veins of 101 men and compared the serotonin concentrations of the blood to weather conditions and seasons. The remarkable results: Men measured on a bright day produced eight times more serotonin, compared to those measured on a dismal day. Of course, the mood improved due to sunlight, with no involvement whatsoever of vitamin D. Thus, regular, non-burning sun exposure is the answer to depression. In addition, remember that sun exposure also leads to the production of other mood enhancers such as nitric oxide, endorphin and dopamine.
For more information regarding sunlight and depression, visit sunlightinstitute.org and read the book, Embrace the Sun.
Happy sunning!
Tuberculosis cases are rising. Embrace the sun! By Marc Sorenson, EdD
Tuberculosis and other diseases are reappearing. Sun exposure is diminishing.
The “Biggest Monster’ Is Spreading. Yet, it is Not the Coronavirus, according to the New York Times.
Tuberculosis kills 1.5 million people each year, and it is the biggest infectious-disease killer worldwide. It is a disease that has caused the death of millions, and evidence of infections date back to about 8,000 BC. Furthermore, the CDC estimates that one-third of the world’s population has tuberculosis. Thus, the Times refers to the disease as the “biggest monster.” That may be true, but antibiotics have never been the answer to Tuberculosis. In addition, the paper indicates that resources used to stop the disease (antibiotics, etc.) have been used to fight Covid-19. Thus, they are scarce. Yet, antibiotics have never been the best answer to tuberculosis. Rather, they serve as a poor substitute for the real answer, which is sunlight.
So, can sunlight quell tuberculosis?
Here is research that should also be of interest to those who love the Sun. In the early 20th century, sun therapy (heliotherapy) treated tuberculosis patients effectively. (Clark, W. Treatment of Bone and joint tuberculosis with Tuberculin and Heliotherapy. Journal of Bone and Joint Surgery 1923;5:721-39.) Dr. Aguste Rollier’s records of 1,129 surgical TB cases showed heliotherapy (sun therapy) cured 87% of “closed cases” and 76% of “open cases.” Hence, among 158 patients with tuberculosis of the hip, 125 were cured and 102 “regained complete recovery of articular function.” Thus, according to one source, “During one period of time, 1,746 of 2,167 tubercular patients under Rollier’s care completely. Consequently, the only failures were among those who had allowed their tuberculosis to enter its most advanced stages.”
The history of Tuberculosis in Bern, Switzerland.
Another study also gave a historical perspective of tuberculosis. It showed how the city of Bern, in Switzerland, obliterated most tuberculosis problems while using lifestyle changes. And those changes included greater access to sun exposure. The authors studied tuberculosis incidence and lifestyle in Bern from 1856-1950. There were three areas of the city assessed due to their historical problems. One was the Black Quarter, where during 1911-1915 there were 550 cases for 100,000 people; the second was the City Center with 327 cases per 100,000 people. The third area was the Outskirts, with 209 cases per 100,000 people. Especially relevant were three living conditions correlating closely to the disease:
- The number of persons per room. Thus, a higher number predicted a greater risk of Tuberculosis.
- A greater number of rooms without sunlight also predicted a greater risk of Tuberculosis.
- In addition, a greater number of windows per apartment predicted a diminished risk of of the disease.
Hence, the country worked to address these problems by improving living conditions, reducing room crowding, building open-air schools and building sanatoria. As a result, TB risk dropped from 330 cases per 100,000 in 1856 to 33 per 100,000 in 1950—a 90% drop! Sanatoria, by the way, were secluded hospitals specializing in healing through good food, fresh air and sunlight.
Can we stop the superbugs?
“Superbug” tuberculosis has now entered the U.S. It is nearly 100% antibiotics resistant, which does not bode well, since it could probably cause an immense killer epidemic. There seems to be no answer to the “superbug” causing it. On the other hand, is there an answer? Could the sun provide a solution to this health threat? The superbugs are upon us like a bad horror movie, and when they start to take over the earth, there will be one remedy: UV light from the sun or sun lamps. We should take care to have our defenses set up in advance by enjoying daily sun exposure.
For more information, visit sunlightinstitute.org In addition, read the book, Embrace the Sun.
Happy sunning!
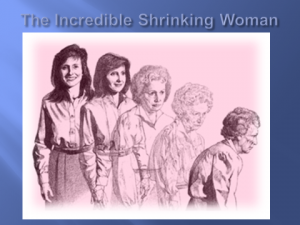
Bone, vitamin D supplements, and sunlight By Marc Sorenson, EdD.
Bone and vitamin D are connected, yet, it may not be in the way you think. It is probably common knowledge that vitamin D is necessary for bone strength, particularly rickets. Yet, beyond rickets, it is not settled science that supplements significantly improve bone strength.
To prove this point, and to cause thoughtful consideration, I call your attention to a meta-analysis of 23 studies. The research assessed change in bone density (BD) from measurement inception to completion of each experiment. The bone densities measured the lumbar spine, femoral neck, total hip, trochanter, total body, or forearm. In addition, all participants took vitamin D supplements. There was little observable change in BD, so the results were disappointing. Thus, the researchers reported, in conclusion, “Continuing widespread use of vitamin D for osteoporosis prevention in community-dwelling adults without specific risk factors for vitamin D deficiency seems to be inappropriate.” Yet, before you give up on vitamin D for bone, let us consider the weakness of the research.
Does bone require much more than 800 IU per day to increase bone strength?
In 10 of the 23 studies cited above, the vitamin D dosage was less than 800 IU per day. This is rather like throwing a packet of food coloring into the sea and expecting the sea to turn red. Direct full-body sunlight during 10-15 minutes can stimulate the skin to produce up to 20,000 IU of vitamin D. Sunlight is the natural way to obtain vitamin D and numerous other healthful photoproducts. A minuscule dose of 800 IU will probably do little for bone strength. Yet, if the researchers had found studies using 3,000 and 5,000 IU, I could have more easily believed their conclusions. However, I could easily have been wrong, as you will see.
So are there other studies that make contradictory conclusions?
No. Most of the research using high-dose vitamin D supplements also had poor results. They usually resulted in much higher fracture risk for those taking the supplements. This was especially true in those who took large, intermittent doses and or intermittent intramuscular injections. Other data showed that doses of more than 4,000 IU daily are associated with more falls and fractures. In addition, research from the Journal of the American Medical Association showed an alarming trend. First of all, treatment with vitamin D for 3 years (4000 IU) day was counterproductive. Thus, it resulted in statistically significant lower bone mineral density (BMD) in certain bones. Furthermore, the same was true for 10,000 IU per day.
Are there better ways to keep bone strong?
Another factor to consider: vitamin D supplements may not be the same as vitamin D made by the human body. The skin always makes natural vitamin D for humans during exposure to sunlight and other sources of UVB light. Irradiating sheep’s lanolin produces the Vitamin D for supplements. Therefore, although 20,000 IU of vitamin D in 20 minutes is possible from sun exposure, the results are very different. Skin-produced vitamin D from sun exposure does not result in increased fracture risk and lower BMD.
The Spanish study on bone and sunlight
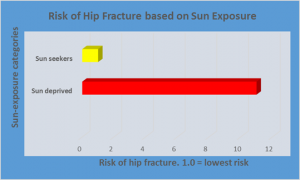
An important study from Spain shows that those who actively sought sun exposure had only 1/11 the risk of hip fracture compared to those who were not sun seekers! In this case, the sun-seeking people must have produced remarkable quantities of vitamin D. They also they increased bone strength remarkably. In addition, we know that the high vitamin D levels certainly caused no problem with bone density and bone strength! How can this be if high doses of vitamin D supplements lead to increased fracture rates? The difference, in my opinion, is the source.
Lessons learned, and conclusions
Therefore, we may take away important lessons from this treatise. First, vitamin D produced by sunlight is not the same as vitamin D from a pill. Moreover, vitamin D is a primary photoproduct of sun exposure. There is an exceptional difference between a pill produced from lanolin and a photoproduct produced in response to sunlight. If sun exposure can produce up to 20,000 IU of vitamin D, and it increases bone strength, something is awry with vitamin supplements, which decrease bone strength. We have produced evidence that show vitamin D supplements may increase bone fragility. It is time to accept the sun or other source of light as the major source of bone strength. That other source could be sunlamps or tanning beds.
A synopsis on bone and sunlight.
Finally, we must realize that sun exposure produces many photoproducts beyond vitamin D. Serotonin, endorphin, nitric oxide; brain-derived-neurotropic factor (BDNF) and dopamine are some of those photoproducts. All of them are vital to human health. Who is to say that these photoproducts do not form a synergistic relationship with sun-produced vitamin D to create the miracle of hip-fracture reduction? Do not neglect your regular, non-burning sun exposure. It may save your bones and your life.
Read more by visiting the Sunlight Institute, and read the book by Sorenson and Grant, Embrace the Sun. Happy Sunning!
 Blondes and Sunlight. By Marc Sorenson, EdD
Blondes and Sunlight. By Marc Sorenson, EdD
Blondes, according to recent research, have longer life spans, and sunlight “could be” the key.
The study involved 29,518 Caucasian women aged 25 to 64, and followed for 25 years, determined their risk of skin cancer and death. Therefore, the researchers formed two groups in the incipient stages of the investigation. Thus, one group was a “fair” group, or blondes, meaning they had red hair or freckles. Another group was the “non-fair” or non-blonde group and served as a control. Furthermore, the researchers matched each person in the fair group with someone in the non-fair group, during the 25-year period. This matching included similar age, smoking habits, education, marital status, and income. The main outcome desired was a comparison of all-cause death (mortality) and mortality from skin cancer in the two groups.
Who lived longer, blondes or non-blondes?The researchers showed that the blondes had significantly lower all-cause death. Still, they had a higher mortality from skin cancer.
Contrasted and compared to the non-blondes, the blondes had significantly reduced all-cause death. What could be the reason for the reduced mortality? One might surmise that sunlight probably played a part. Yet, sunlight was not a focus of this investigation.
Nevertheless, it is especially relevant that these researchers, in a 20-year study on sunlight, showed other surprising results. In a study on sunlight exposure, they demonstrated an amazing fact. They showed that low sun exposure habits were approximately as dangerous as smoking. This was probably due to reduction in cardiovascular disease (heart and vessel disease) among those who soaked up more sun.
Why might light-skinned people have an advantage?
Those who have lighter skins make vitamin D and other important sunlight photoproducts at a rapid rate. Some of those photoproducts are nitric oxide, serotonin, endorphin, dopamine, and BDNF. Furthermore, all of those photoproducts are essential to human health. So could this be the reason that blondes lived longer than non-blondes? For more information on the effects of these photoproducts, visit sunlightinstitute.org and read the book, Embrace the Sun.
A final, salient point regarding sunlight, blondes and skin cancer:
A most noteworthy thought: people who have light skins and/or freckles are already at dramatically increased skin-cancer risk. Thus, it is light skin, freckles and moles that increase skin cancer; it is not sunlight. If the blondes group had accumulated more sunlight exposure, It might have actually protected them from skin cancer. Read more about how sun prevents skin cancer in Embrace the Sun. Regular, non-burning sun exposure is vital.
Happy sunning!
Vitamin D, prostate cancer and sunlight By Marc Sorenson, EdD
Vitamin D is a magnificent, critically important photoproduct of sun exposure, sun lamps and sunbeds (tanning beds). It is not really a vitamin, but rather a hormone that controls hundreds of genes in the body. The production of this hormone occurs in the skin in response to UVB light from the aforementioned sources. About 90% of vitamin D blood levels, across the average population in the U.S., occurs through sun stimulation to skin. Supplements and food sources provide only a small amount of vitamin D on average.
Vitamin D and other cancers, including prostate cancer (PC)
There is a close association of high vitamin D levels and lowered risk of breast cancer and many other cancers. Therefore, it seems logical that supplementation might also reduce PC risk. However, it seems like that may not be the case, and it needs further discussion. In fact, vitamin D studies show only weak correlations between vitamin D levels and a reduction in PC. The highest levels of serum vitamin D shows a J-shaped curve, meaning those levels actually associated to a slightly increased risk. No such increase occurs with the highest levels of sunlight exposure–quite the opposite. The highest levels of sunlight associated to the highest levels of protection against PC.
An interesting study on sunlight, vitamin D and prostate cancer.
It was with interest, therefore, that I read a recent article describing the effect of sunlight on PC, called “Sunlight could decrease prostate cancer risk.” After affirming that sunlight exposure could reduce the risk of PC by 50%, the author unfortunately stated, “This does not mean men should deliberately sunbathe to reduce their risk of prostate cancer. Outdoor exercise and an adequate amount of vitamin D from diet should be sufficient to afford protection from the disease.” Yet, this is not a statement based on science, especially considering the J-shaped curve. Thus, the author obviously assumed vitamin D caused the association of sun exposure to reduced PC risk.
Now, let’s talk about some impressive studies on sunlight per se.
Here are some rather interesting studies regarding sun exposure and PC. In addition, there are numerous others discussed in the book, Embrace the Sun. Probably the most stunning paper was one in which researchers used childhood sunburn as a measure of sun exposure. As a result, they determined that men who experienced sunburns as children were protected against PC. Consequently, they had one-fifth the risk of contracting prostate cancer as those who had not sunburned! However, please do not burn!
Let us be careful about our sunlight!
In addition, a note of caution regarding sunburn: I do not recommend that anyone sunburn to prevent prostate cancer. The researchers used sunburn to predict higher vitamin D levels. Yet, sunburn is not necessary to achieve the remarkable results, since non-burning sun is sufficient. Most noteworthy, this research also demonstrated that men with the lowest sunlight exposure had more than three times the risk of prostate cancer. A follow-up to this study was also interesting. Men in the lowest quartile of sunbathing had a 5.3-fold greater risk of prostate cancer compared with men in the highest quartile.
A final thought
One more paper, cited in conclusion. Researchers have stated, “Higher levels of cumulative sun exposure, adult sunbathing, childhood sunburn and regular sunny holidays in hot climates were each independently and significantly associated with a reduced risk of this [prostate] cancer.”
Men, protect your prostate by obtaining plenty of non-burning, regular sun exposure.
For more information on myriad positive sun articles, visit http://sunlightinstitute.org/ and read the book, Embrace the Sun, by Sorenson and Grant.
Sunlight, sex and sexual dysfunction. By Marc Sorenson, EdD.
Sunlight, sex and sexual dysfunction is a title that generally catches attention. Sexual dysfunction problems are rampant in our society, and those who claim to have answers usually draw immediate attention. Do I have answers and good advice? Probably—I will let you judge. Let us look at some research, and results gained, from sunlight and vitamin D.
Sexual dysfunction among women.
The first, and most recent women’s study, shows Vitamin D3 deficiency associates with Female Sexual Dysfunction (FSD) in Premenopausal Women. Moreover, we know that sun exposure to skin produces 90% of serum vitamin D levels. The scientists conducting this study measured vitamin D levels in 50 premenopausal women with FSD, and 58 healthy controls. The average age of the women was 35 years. Furthermore, all of these women completed a Female Sexual Function Index (FSFI) questionnaire. The investigators then correlated sexual desire, arousal, lubrication, orgasm, satisfaction and pain scores to the vitamin D levels. In addition, they evaluated all women for depression with the Beck depression Inventory (BDI).
Results for the women’s study:
Vitamin D levels were about 40% lower in the women with FSD than in the healthy controls. In addition, the results of each sexual function, spectacularly favored the healthy controls. Consequently, the researchers stated their results in this manner: “Desire (p = 0.0001), arousal (p = 0.0001), lubrication (p = 0.002), orgasm (p = 0.0001), satisfaction (p = 0.018), and pain (p = 0.010) domain scores were also correlated with the levels of serum 25-hydroxyvitamin D3.”
The p score or value means the probability value. Hence, it indicates the probability of obtaining test results at least as extreme as the results actually observed. Thus, the p-value for desire, arousal, lubrication and orgasm are extremely significant. The other sexual functions, satisfaction and pain (lack thereof), were also significant.
Why is sexual dysfunction in women so important?
A study in the journal, Sexual Medicine Review, showed that female sexual dysfunction affects 41% of premenopausal women around the globe. This is not normal, and in my opinion, is due to widespread sunlight deficiency. Sunlight deficiency leads to the deficiency of vitamin D, which results in untold suffering and frustration among women and their husbands. If something as normal and natural as regular, non-burning sun exposure could lead to a more satisfying sex life, would it not be worth the effort?
For more information on the terrific, healthful effects of sunlight and vitamin D, visit sunlightinstitute.org. In addition, read the book, Embrace the Sun.
Sunlight prevents breast cancer. By Marc Sorenson, EdD.
Sunlight prevents breast cancer by many means. Many scientists believe this. Moreover, sunlight also stimulates human skin to produce vitamin D. Therefore, many professionals assume vitamin D is responsible for the reduced risk. Thus, this may lead them to advocate the use of vitamin D supplementation and totally miss the bigger picture. In addition to vitamin D, sunlight or sunlamps produce many supplementary and healthful photoproducts. Among others, sunlight produces nitric oxide, dopamine, serotonin, endorphin and brain-derived neurotropic factor (BDNF). In addition, all these photoproducts are vital to health. Hence, it is likely that these healthful photoproducts lead to an inhibition of breast cancer.
New research shows that sunlight prevents breast cancer independently of vitamin D.
Consequently, it should not surprise us that for breast cancer, sunlight’s effects go beyond vitamin D. Researchers at Children’s Hospital Oakland Research Institute, used a mouse model that easily develops breast cancer. They also treated them with UVR light such as found in sunlight. Much as we might expect, they found that UVR treatments produced significant anti-cancer effects. Furthermore, they found that neither dietary vitamin D nor topical vitamin D influenced cancer risk. Because of their findings, they stated the following: “UVR’s inhibitory effects occur irrespective of whether or not the treatment increases circulating D3 in the mice.” Then they also made another important comment regarding their research. “Therefore, supplemental D3 may not mimic all possible beneficial effects of UVR. Uncovering non-D3-mediated mechanisms of UVR tumor inhibition may lead to novel strategies for cancer prevention.”
An important point about how sunlight prevents breast cancer.
Finally, there is no doubt that vitamin D has anticancer benefits. This research however, is especially relevant because it corroborates what I have said in my book, Embrace the Sun. Consequently, we must not put all of the benefits of sunlight in the vitamin D box. Furthermore, sun exposure performs myriad miracles beyond vitamin D. One of those miracles may be breast cancer prevention and inhibition. In addition, if we erroneously believe we can obtain all of the sun’s benefits from popping a pill, we may miss the holistic effects sunlight, which provide a cornucopia of salubrious results.
So, safely (without burning) embrace the sun, since it helps prevent breast cancer.
For more information, visit sunlightinstitute.org. Another great tip is to read the book, Embrace the Sun.
Happy sunning!
Sunlight outside the body stops transmission of Covid-19. By Marc Sorenson, EdD.

Sunlight outside the body, as regards Covid-19, may be a rather new and intriguing concept. Yet, we have alluded to it briefly in a previous blog. Research from the Department of Homeland Security (DHS) corroborates the idea that direct sunlight rapidly kills the Covid-19 virus. The researchers tested effects of sunlight on Covid-19 viruses in aerosols, suspensions of solid particles or liquid droplets in air. These aerosols represent a potential route of disease transmission, and in this case, transmissions of Covid-19 viruses. Therefore, if sunlight exposure accelerates the decay of these viruses, it prevents an avenue of human-to-human transmission. Thus, breathing in of viruses coughed, sneezed, or even breathed out by others (as in saliva) ceases to be problematic. Sunlight outside the body inactivates the viruses due to decaying them.
The bottom line regarding outside sunlight and Covid-19.
Because of this research, it we know that without sun exposure, the time required to decay the virus was 125 minutes. With direct sunlight, the time ranged from 6 to 19 minutes, according to the intensity of the exposure. That is a profoundly significant change, and is probably why Florida fared so much better than New York, with Covid-19.
Hence, we have shown that sunlight is a two-edged sword; sunlight outside the body helps to halt transmission of the disease. Sunlight’s ability to produce vitamin D in the skin (inside the body) prevents the cytokine storm, which is how Covid-19 kills.
People have long believed that sunlight was the best disinfectant.
First, the German microbiologist Robert Koch, who isolated TB bacteria in 1882, showed that sunlight had disinfectant qualities; it destroyed tuberculosis bacteria. In addition, even earlier, in 1877, other researchers discovered that sugar water left in the shade became cloudy, indicative of bacterial growth. However, if exposed to sunlight, it remained clear. Dr. Zane Kime, in his book, Sunlight Could Save Your Life, wrote that history. In addition, he also reviewed the results of research conducted between 1886 and 1909. Most noteworthy, it showed that the following bacteria succumbed to ultraviolet light: Anthrax, plague, streptococci, tubercle bacillus, cholera, staphylococcus, colon bacillus and dysentery bacillus. Nevertheless, most people forgot sunlight with the advent of antibiotic drugs, but now the interest has returned. (Cited in Kime, Z. Sunlight Could Save Your Life. World Health Publications, Penryn, CA 1980:126-30.) Also, read Embrace the Sun.
So, please realize that the master disinfectant, sunlight, is the best in the world. Thus, it is ready to do battle with the worst the Covid-19 virus can throw at the human body. Get your share of non-burning sunlight and survive this pandemic. For more information, visit sunlightinstitute.org and read the book, Embrace the Sun.
Happy sunning!