Sunlight and Health: by Marc Sorenson, EdD
Sunlight and health is an article written to fulfill a request from Grassroots Health (GRH). GRH is a marvelous organization; its purpose is to promote the healthful benefits of vitamin D (and sunlight).
Sunlight and health, from the earliest human civilizations to our current battle with COVID-19, have an inseparable link. Dr. John Fielder’s exceptionally well-written paper, History of Heliotherapy, provides insight into the past. Many ancients deified sunlight. The populations of those times had no doubt of its healing powers. Hippocrates, the Greek physician known as the “father of medicine,” recommended sunbathing and had his own large solarium, an enclosed area for sunning. In addition, the ancient Romans, used thermae (hot tubs and baths) that were equipped with solaria. The Roman philosopher Pliny wrote, “Sun is the best remedy.”
Sunlight and health maintained a link well into the 20th century.
In the early 19th Century, scientists began to experiment with heliotherapy (sunlight therapy) as a healer. They were duly impressed with their results. Therefore, they attempted to build a new system of therapeutics based on heliotherapy. In 1857, Madame Duhamel exposed children with TB to sunshine because it hastened their recovery. Many other doctors also used heliotherapy with great success. Dr. Fielder said that sunbathing was so successful, all doubt as to its place in the hygienic system was ensured.”
Though nothing has really changed, regarding sunlight and health, doubts about the relationship have crept in.
In the early 20th Century, people noticed that farmers developed common skin cancers on their faces and hands. This news began the war on sunlight. Nevertheless, the sun held its own for some time, because research also showed sunlight had anti-cancer properties. This idea triggered a 1932 editorial in The Lancet medical Journal. It suggested sunlight was so effective in promoting health, that the government should reserve public areas for nude sunbathing! (Dawson, Lord. Naked and Unashamed. Lancet 6, 1932:688.)
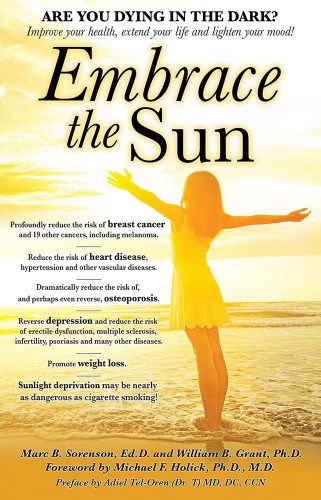
Then, the tide began to turn. Scientists completely misrepresented the association of common skin cancers and melanoma:
Due to this egregious misrepresentation, scientists decided, regrettably, that that sunlight must cause melanoma, the deadly skin cancer. A new fear had been born, along with a new industry-sunscreen and new medical profits. Even though moderate, regular sun exposure protects against melanoma, this fear-vs-fact based decision launched an all-out assault on the sun. Moreover, it continues today. Unfortunately, it has also become ‘rewarding’ to the industry that provides tanning lotions and treatments for the cancers. View this video by Dr. Edward Gorham to learn more about this subject: Vitamin D: Skin Cancer/Sunscreen – the Dilemma.
To dispel the myths, here are the facts about melanoma:
Seventy-five percent of melanomas occur on body areas seldom exposed to sunlight.
In the U.S., as sun exposure has decreased by about 90% since 1935, melanoma incidence has increased by 3,000%. Documentation in Embrace the Sun. See the graph below.
As in the US, while sun exposure in Europe has profoundly decreased, there has been an exponential increase in melanoma.
Men who work outdoors have about half the risk of melanoma as men who work indoors.
Outdoor workers, while receiving 3-9 times the sun exposure as indoor workers, have had no increase in melanoma since 1940. Melanoma incidence in indoor workers has increased steadily and exponentially.
Sunscreen invention, and its steadily increasing use, has not reduced the risk of melanoma. In fact, melanoma increased as sunscreen use increased. Documentation in Embrace the Sun.
Because of all this, increasing melanoma incidence significantly correlates with decreasing personal annual sunlight exposure.
Outdoor workers do get numerous sunburns and still have a dramatically lower risk of contracting melanoma.
Thus, melanoma increases as sun exposure decreases. Therefore, there is much need to provide the education and data to everyone so they can avoid blaming the sun.
Here are more facts about melanoma and its prevention:
Another cause is alcohol; those persons in the highest fifth of alcohol consumption have a 65% increase in melanoma risk.
In addition, meat consumption may increase melanoma risk by 84%.
Furthermore, daily fruit consumption may reduce the risk of melanoma by nearly 50%.
Persons with the highest levels of PCBs (banned industrial chemicals) have 7-times the melanoma risk as those with lowest levels.
There is a positive association between melanoma and obesity. It is also interesting to note that the increases in both diseases have progressed in unison.
Furthermore, the highest number of new melanoma cases are in Utah, followed closely by Vermont, Minnesota and New Hampshire. Another “surprising” fact is that by far the lowest number of new cases are in Texas.
So, since melanoma continues to increase in lock step with reduced sun exposure, should we continue to blame the sun?
We have destroyed the misconception that sunlight is a major cause of melanoma. Let us proceed to the magnificent health-protective effects of regular, non-burning sun exposure against other diseases:
Research from Indonesia shows COVID-19 deaths are 20 times higher among those with vitamin D levels less than 20 ng/ml. That is, when compared to those with levels greater than 30 ng/ml. Consequently, had the researchers had subjects vitamin D levels greater than 50 ng/ml, I would predict no deaths at all. In addition, remember that sun exposure to the body produces 90% of serum vitamin D levels (in the overall population). Therefore, we see the profound effect sun exposure could have on COVID-19.
Indonesians have taken this research seriously. Below is a photo of Indonesian men “social distancing” in the sunlight.
Another fact about sunlight and health with Covid-19
Recent research from the Department of Homeland Security (DHS) showed another interesting aspect of sun exposure’s influence on Covid-10. They demonstrated that direct sunlight “quickly” killed all Covid-19 viruses both in aerosols and on objects. Thus, sunlight not only stops the disease inside the body, but also stops transmission of the disease outside the body. This makes sunlight a powerful, two-edged sword against the disease.
Sunlight and Health: More facts regarding the influence of sun exposure on disease.
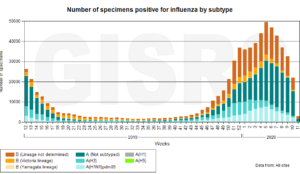
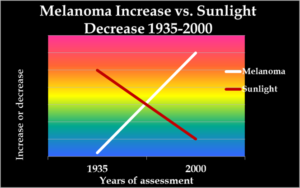
Influenza diminishes almost to nothing during late spring, summer, and early fall – times of greatest sun exposure. See the chart below, produced by the WHO and provided by Goran Olsson of Moscow, Russia.
Yet, we do not yet have annual data for COVID-19, a “flu-like” disease. However, it did emerge in the northern hemisphere in winter when sun exposure and vitamin D levels are low.
Women who sunbathe regularly have half the risk of death, over a 20-years period, compared to those who stay indoors.
In addition, a Spanish study shows that women who seek the sun have one-eleventh the hip-fracture risk as sun avoiders.
Another fact is that those who avoid sun have 10-times the breast cancer risk as those who embrace the sun.
Multiple sclerosis (MS) is highest in areas of little sunlight and virtually disappears in areas of year-round direct sunlight.
Additionally, sun exposure decreases heart disease risk through nitric oxide production.
Sun exposure improves mood through production of serotonin and endorphin.
Morning sun exposure resets the circadian rhythm, which synchronizes physical, emotional and mental processes and associates with lower cancer rates.
Those persons who spend many hours daily outdoors have only 1/50 the risk of Parkinson’s disease.
For each death caused by diseases associated with sun exposure, there are 328 deaths due to diseases associated with sun deprivation.
Sun exposure increases the production of BDNF (Brain-Derived Neurotrophic Factor), essential to nerve function and protection.
Furthermore, sunlight produces up to 20,000 IU of vitamin D in 20 minutes of exposure at midday in sunny seasons.
In England, vitamin D deficiency in children increased by 83 times during a 14-year period. That is likely due to indoor living and sunscreen use.
Finally, as part of my analysis of sunlight’s positive powers, I, and my coauthor, Dr. Bill Grant, performed a death analysis.
First of all, we assessed the number of deaths caused by diseases associated with high sun exposure. In addition, we performed another analysis of the number of deaths associated with diseases of sun deprivation. Here are the deaths for diseases associated with low sun exposure:
Diseases associated with low sun exposure in the USA
| Disease | Year | Deaths |
| Osteoporosis | 2005 | 71,280 |
| Osteoarthritis | 2004 | 500 |
| Rheumatoid arthritis | 1998 | 2,060 |
| Bladder cancer | 2016 | 16,390 |
| Brain cancer | 2016 | 16,050 |
| Breast Cancer | 2016 | 40,980 |
| Cervical cancer | 2016 | 4,074 |
| Colon cancer | 2016 | 49,190 |
| Endometrial cancer | 2016 | 10,470 |
| Gallbladder cancer | 2016 | 3,710 |
| Kidney cancer | 2016 | 14,240 |
| Lung cancer | 2016 | 158,080 |
| Leukemia | 2016 | 24,400 |
| Lymphoma | 2016 | 21,270 |
| Multiple myeloma | 2016 | 12,650 |
| Oral and pharyngeal cancer | 2016 | 9,570 |
| Ovarian cancer | 2016 | 14,240 |
| Pancreatic cancer | 2016 | 34,920 |
| Prostate cancer | 2016 | 26,120 |
| Thyroid cancer | 2016 | 1,980 |
| Cardiovascular disease | 2015 | 801,000 |
| Diabetes | 2010 | 69,071 |
| Crohn’s disease | 2004 | 825 |
| Asthma | 2010 | 4,000 |
| Influenza | 2010 | 36,000 |
| Pneumonia | 2016 | 53,282 |
| Septicemia | 2012 | 35,000 |
| HIV – AIDS | 2013 | 6,995 |
| Necrotizing fasciitis | 2010 | 200 |
| Tuberculosis | 2014 | 555 |
| COPD | 2009 | 145,575 |
| Total annual deaths, approximated | 1,684,677 |
There were few deaths from diseases associated with high sun exposure-approximately 5,125.
Consequently, there are, according to our calculations, approximately 1,684,677 yearly deaths caused by diseases associated with low sun exposure. This compares to 5125 deaths from diseases associated with high sun exposure, and produces a ratio of approximately 328:1. Therefore, based on this analysis we concluded that it defies common sense to continue the anti-sun campaigns prevalent today. This ratio demonstrates that regular, non-burning sun exposure (without sunscreens), is desirable. It should be encouraged as a prudent precaution. It would to yield a highly beneficial effect on health and well-being. This ratio should make anti-sun advocates think twice about suggesting that we avoid sun exposure. This is particularly important for African Americans, who have the highest risk of death from Covid-19.
With COVID-19 attacking us like a bad horror movie, we must act now to stop the carnage, and bring the citizens back into the sunlight. Sunlight is a requirement for optimal human health.
For more information on sunlight and health, visit sunlightinstitute.org and read the book, Embrace the Sun. Happy sunning!
Happy sunning!
Coronavirus, sunlight and vitamin D. More compelling information. Take action now. By Marc Sorenson, EdD.

 Coronavirus, (Covid-19), like most flu-like diseases, will probably disappear in much of the Northern hemisphere in the coming summer. Nevertheless, it will return on steroids in the fall and winter. Yet, it does not have to return to you or your family and friends. We can do something! However, why wait? Let us start now! Does anyone reading this really want to wait for the “second wave” and then go into panic mode? Of course not. In addition, do you want to let the vaccine Nazis also spend $billions more of our tax dollars looking for a vaccine? Of course not. The answer to stopping coronavirus is all around us. We need only to seek it and use it.
Coronavirus, (Covid-19), like most flu-like diseases, will probably disappear in much of the Northern hemisphere in the coming summer. Nevertheless, it will return on steroids in the fall and winter. Yet, it does not have to return to you or your family and friends. We can do something! However, why wait? Let us start now! Does anyone reading this really want to wait for the “second wave” and then go into panic mode? Of course not. In addition, do you want to let the vaccine Nazis also spend $billions more of our tax dollars looking for a vaccine? Of course not. The answer to stopping coronavirus is all around us. We need only to seek it and use it.
Two papers show remarkable associations of coronavirus with vitamin D.
If you are not convinced of the power of sunlight after reading this, I despair of being able to help you prevent this fall’s “second wave.”
The first paper was by a team of Indonesian researchers. One might think that Indonesians would have ample vitamin D levels due to an abundance of sunlight. Thus, this should protect them from vitamin D deficiency. However, most Indonesians avoid the sun and keep their skins as white as possible. It is a national quest in the Philippines to be as light-skinned as possible, so that they can consider themselves as “upper crust.” Hence, the population has a great deal of vitamin D deficiency.
The researchers focused on identifying patterns of mortality (death) between coronavirus deaths and vitamin D levels. They conducted the study with a sample of 780 subjects, all who had laboratory confirmed coronavirus infection.
Here are the findings on vitamin D levels and coronavirus mortality:
- Mortality rates were 13 times higher in patients who were vitamin D insufficient (21-29 ng/ml) compared to those who had normal levels (>30 ng/ml).
- Mortality rates were 19-times higher in patients who were vitamin D deficient (<20 ng/ml).
- Even when controlling the data for age, gender and preexisting conditions, the vitamin D deficient cases were more than 10 times more likely to die than those who had normal levels.
No wonder the Indonesians are now seeking the sun and appreciating it after years of avoiding it. See the picture below of Indonesian men social distancing while soaking up the rays.
An important point regarding vitamin D and coronavirus:
Vitamin D levels above 30 ng/ml are not necessarily “normal,” and it is likely that 50-60 ng/ml would be a better number. People who are constantly in the sunshine, i.e. lifeguards, often have levels above 70 ng/ml. Dr. Bruce Hollis and his colleagues suggested that lifeguards have the “true normal” levels. They believe that a population of “normal” volunteers with average levels of 27 ng/ml may exhibit vitamin D deficiency. Another similar study showed that “normal” adults had 25(OH)D levels of about 27.2 ng/ml, whereas lifeguards had levels of approximately 70 ng/ml].
Could the real pandemic be a pandemic of sunlight deficiency resulting in a pandemic of vitamin D deficiency?
If >30 ng/ml provides this much protection against coronavirus, levels > 60 ng/ml would probably provide complete protection. Everyone should have a vitamin D assessment, and then get out in the sun, during this time of the coronavirus epidemic. For your own health, and the health of those you love, schedule a test, and make your goal 60 ng/ml.
Paper # 2
Another paper by Mark Alipio, done in the Philippines, was similar to the Indonesian study. Thus, it showed that coronavirus patients with normal vitamin D levels had a mild disease outcome. The outcome for those patients was 19.6 times better than for those with low levels.
A fact everyone should remember:
Ninety percent of serum vitamin D levels are due to sun exposure, which causes the skin to produce vitamin D3. Therefore, vitamin D levels are surrogate measurements for sun exposure. You must not assume that vitamin D capsules will supply all the beneficial effects of sun exposure or sunbed exposure. Both sunlight and sunbed light produce photoproducts that have health effects far beyond vitamin D. Safely sunbathe (without burning) to achieve optimal vitamin D levels. Moreover, while so doing, you will produce other remarkably important health benefits.
For more information on the extraordinary health benefits of sun exposure, visit sunlightinstitute.org and read my book, Embrace the Sun.
Covid-19 and sunlight, in our hearts and minds, by Marc Sorenson, EdD
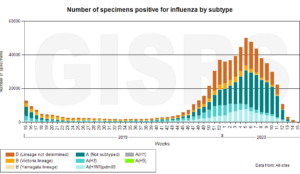
Covid-19 (coronavirus) is a topic that is inescapable in our times. The media discusses it relentlessly and it is in the hearts and minds of nearly every citizen. And why not? We all know of friends or acquaintances who have had the disease, and it has become a political football. So what can we do about it? There are certain geographical and population differences in Covid 19 incidence and death that may provide some insight. Thus, New York and Florida provide interesting contrasts for the difference in incidence.
Shawn Hannity’s interview with Florida’s Governor DeSantis provides thought-provoking insight and fascinating facts regarding Covid-19.
First of all, Florida and New York are heavily populated states. Yet, as you can see from this graph, death risk is minuscule in Florida compared to New York. The graph shows the comparison of death rates.
Because of New York’s high population density, with people living nearly on top of each other, epidemic diseases spread easily. Thomas Jefferson, third president of United States, once made this clairvoyant statement. “When we get piled upon one another in large cities, as in Europe, we shall become as corrupt as Europe.” Perhaps he should have used the word “ill” rather than corrupt.
Here are more reasons for the stark contrast in Covid-19 deaths between New York and Florida.
Here are New York’s responses to the Covid-19 epidemic.
- New York shut down nearly all social gathering places. Yet, their leaders in the beginning told people to congregate and have a good time.
- New York made homes a breeding ground for Covid-19 infection with “shelter in place” orders.
- New York forced many elderly patients and others, whom they had no room for in regular hospitals, to live in nursing homes. Thus, they produced a hotbed for infection. Twenty-five percent of all deaths from Covid-19 in New York occurred in nursing homes.
- New York has resisted the demand to return people to work and to use outdoor areas with social distancing.
- Furthermore, New York City was appallingly unprepared to provide masks, ventilators and other medical equipment.
The reaction to Covid-19 in Florida.
- Florida allowed access to its beaches and provided guidelines for social distancing.
- Florida also continued to allow golfing, with guidelines.
- In addition, Florida acted quickly against Covid-19. A research study shows that Florida is entering a safe area of declining contagion.
- Florida immediately concentrated on the elderly and other at-high-risk populations, in spite of an exceptionally large elderly population. Thus, they had a remarkably low death rate among the elderly.
- Florida showed far better preparation than New York. Thus, it moved quickly to impede the epidemic. Consequently, one of the charts on the interview with Hannity showed that fatalities per 100,000 were 1.8 in Florida. Yet, there were to 101.2 fatalities per 100,000 in New York.
- Florida has much more sunshine simply because it is in the South. I showed a plethora of healthful effects offered by regular, non-burning sun exposure in my last blog. I will list them once more here to refresh your memory:
The power of sunlight for health beyond Covid-19
- Influenza diminishes almost to nothing during late spring, summer, and early fall, times of greatest sun exposure and vitamin D production.
- Seventy-five percent of melanomas occurs on areas of the body seldom or never exposed to sun.
- Women who sunbathe regularly have half the risk of deathduring a 20-year period compared to those who stay indoors.
- A Spanish study shows that women who seek the sun have one-eleventh the hip-fracture riskas sun avoiders.
- Men who work outdoors have half the risk of melanomaas those who work indoors.
- Women who avoid the sun have 10-times the risk of breast canceras those who embrace the sun.
More benefits of sunlight exposure
- Multiple sclerosis (MS) is highest in areas of little sunlight, andvirtually disappears in areas of year-round direct sunlight.
- Sun exposure decreases heart disease risk through nitric oxide production.
- Sun exposure dramatically improves mood through production of serotonin.
- Those persons who spend many hours daily outdoors have only 1/50 the risk of Parkinson’s disease!
- For each death caused by diseases associated with sun exposure, there are 328 deaths caused by diseases associated with sun deprivation.
- Sun exposure increases the production of BDNF, essential to nerve function.
- Sun exposure can produce as much as 20,000 IU of vitamin D in 20 minutes of full-body sun exposure.
- In the U.S., vitamin D deficiency in children has increased by 83 times during a 14-year period. That is likely due to indoor living and sunscreen use.
Conclusions regarding New York, Florida and Covid-19
Florida made better choices and earlier choices regarding the Covid-19 epidemic. They also opened their beaches in a reasonable manner. This allowed more sun exposure.
When the disease diminishes this summer, it will be due to sun exposure that produces vitamin D and many other healthful photoproducts. In addition, remember, that sun exposure effects positive changes well beyond stopping the coronavirus.
Non-burning sun exposure is essential, and best around midday. Do not overexpose. My previous blog presented guidelines for sun exposure. Also, be sure to read my book, Embrace the Sun. In addition, visit my previous blog for more information.
Happy Sunning!
UV index. Vita min D and health. By Marc Sorenson, EdD
min D and health. By Marc Sorenson, EdD
The UV index is a measure of the intensity of ultraviolet radiation B (UVB) from the sun. It is expressed as a number on a scale of 0-11. A higher number indicates a higher sunlight intensity. Exposure to the ultraviolet B (UVB) portion of sunlight is necessary to cause the skin to produce vitamin D. Nevertheless, unless the body is deeply tanned or naturally very dark, a very high UV index can cause sunburn, so caution is necessary.
A low UV index is also problematic.
However, if the UV index is very low, it cannot stimulate the production of vitamin D in the skin. Vitamin D production is essential for human health. Thus, lack of vitamin D may be a major reason that flu-like diseases occur primarily during winter, when there is little or no vitamin D production. This, of course varies according to latitude.
A List of vitamin D benefits from Business Insider.
A recent article from Business Insider (a Philippines online paper) discussed various health effects of vitamin D and sun exposure. Here are some of their salient points, not all of which are correct.
- The primary cause of vitamin D deficiency is sun deprivation (correct).
- Vitamin D helps keep the immune system, so deficiency could be the reason for frequent flu (correct).
- You can get more vitamin D by spending at least 5 to 10 minutes outside 3 times a week without sunscreen (correct).
How much vitamin D does a person need?
- The most incorrect statement of the article is this. The average adult needs around 600 international units (IU) of vitamin D a day (not correct). For reference, a serving of salmon contains roughly 400 IU (not correct). 20 minutes of full-body, unobstructed sunlight can cause the skin to produce up to 20,000 IU of vitamin D. If 600 IU were the only source of vitamin D, one would produce a level of six ng/ml, which would be woefully inadequate. 600 IU is only slightly better than nothing.
- Fifteen minutes of non-burning midday sun (without sunscreen) would optimize vitamin D levels in a few days. Dark-skinned individuals would need much more exposure, up to an hour.
-
Getting more frequent colds or respiratory infections could be a symptom of vitamin D deficiency (correct). However, it is even more likely to be a sign of sunlight deprivation.
- Colds and flu nearly disappear in the summer when the sun is direct. During this time of the coronavirus epidemic, everyone on earth needs daily direct or indirect sun exposure. Those who do not tan can obtain plenty of sunlight from being outdoors under an umbrella or even in the shade near where the sun is shining.
-
Bone diseases, vitamin D and sunlight.
- Vitamin D deficiency can cause Osteomalacia and Osteoporosis, conditions where your bones become less dense (correct). Sun exposure produces about 90% of the body’s serum levels of vitamin D. In addition, not all vitamin D supplement studies have produced stronger bones.
Sunlight is king for increasing bone strength.
- However, sun exposure, or exposure to sunbeds (tanning beds) produces marvelous results. For example, a Spanish study showed that women in Spain—those who regularly enjoyed sun exposure—had about one-eleventh the risk of hip fractures as women who had little exposure. Women who use sunbeds also have profoundly higher bone mass than women who do not use them. Their vitamin D levels are also remarkably higher.
-
Mental problems due to a low UV index and subsequent vitamin D deficiency.
- Vitamin D has some links to depression (correct). Nevertheless, that link in my opinion is 100% due to to sun deprivation. Dr. Gavin Lambert and his colleagues in Australia measured serotonin levels in response to varying degrees of bright light. To do so, they drew blood samples from the internal jugular veins of 101 men and compared the serotonin concentrations of the blood to weather conditions and seasons. The results were remarkable: Men measured on a very bright day produced eight times more serotonin than those measured on a cloudy, dismal day.
More on the UV index and “solar noon.”
When meteorologists report UV index, the emphasis usually warns against the maximum UV level. That level generally occurs around “solar noon.” Solar noon is a four-hour period stretching from 10:00 AM to 2:00 PM. As you have probably noticed, forecasters constantly warn us to avoid the 10:00 to 2:00 hours. Avoiding intense UV radiation is their watchword. Many of them say, “Get sun exposure in the early morning or late afternoon to produce vitamin D.” They should know that the UV index must be over 3 to produce vitamin D.
These reporters do not understand how low UV index hinders vitamin D production.
They do not comprehend that UV index is so weak in the morning that it produces absolutely no vitamin D. The same is true in the evening. Therefore, the closer to solar noon you plan your outdoor time, the more vitamin D you will produce. Vitamin D produced in the skin from solar UVB exposure does not lead to vitamin D toxicity and is safe, as the body limits its own production.
Another method to measure the efficacy of sunlight for vitamin D is to stand in the sun at any time of day and observe your shadow. If your shadow is shorter than your height, you are producing vitamin D. This, the shorter the shadow, better.
Caveats regarding the UV index and vitamin D. Morning sun is still very healthful.
Early morning sun exposure, when the UV index is very low, (under 3) has remarkable health effects. These include resetting the circadian rhythm, increasing production of serotonin, lowering blood pressure through nitric-oxide production and assisting weight loss. Nevertheless, vitamin D stimulation in the skin is not one of the health effects of early morning light.
So safely soak up the sun at any time of day and reap the health benefits. Never burn.
Happy sunning!
For more information: http://sunlightinstitute.org/ and read the book, Embrace the Su n.
n. 
Death by Prescription Drugs. By Marc Sorenson, EdD.
 Are there better ways to heal? Could there be better ways to fight the coronavirus? (be sure to scroll down to the WHO flu graph.)
Are there better ways to heal? Could there be better ways to fight the coronavirus? (be sure to scroll down to the WHO flu graph.)
Death by prescription drugs is commonplace. Therefore, perhaps whole foods, avoidance of junk foods and plenty of sunlight are better alternatives. Thus, our approach here will be (1) to explain the health burden inflicted by prescription drugs. (2) To make nutrition suggestions and (3) finally propose exercise and sunlight as additional solutions.
Death and prescription drugs. The danger is real!
Since you probably realize that prescription drugs are ubiquitous, did you also realize just how dangerous they are? Would it get your attention to tell you that they are the fourth leading cause of death?
U.S. News published an interesting article, which makes us wonder if our pharmaceuticals do more harm that good. Are they healers of killers? Here are some of the most noteworthy facts the article presents:
Salient points from the article on Death and prescriptions.
- First, prescription medications are the fourth leading cause of death and a major cause of additional illnesses among Americans.
- A recent analysis estimates 128,000 Americans die each year due to taking medications as prescribed.
- In addition, adverse drug reactions from properly prescribed and used medicines result in 1.5 to 2.7 million hospitalizations each year.
- Sixty to 70 percent of us take at least one prescribed drug and many take an additional fistful of pills daily.
- A quote from Dr. Donald Light [apropos, no?], who analyzed the data: “By far the greatest number of [prescription drug-related] hospitalizations and deaths occur from drugs that are prescribed properly by physicians and taken as directed.” This comes from his paper entitled “Institutional Corruption of Pharmaceuticals and the Myth of Safe and Effective Drugs.”
- Another quote from Dr. Light’s paper: “About 2,460 people per week are estimated to die from drugs that were properly prescribed. And that’s based on detailed chart reviews of hospitalized patients.” [That of course, does not include the 1.5-2.7 hospitalizations that occur due to prescriptions.]
- The paper continues, “And though following a doctor’s orders and medication labeling instructions can reduce harms associated with taking prescription drugs, simply taking prescribed drugs as directed can expose a person to significant risk.”
Of course, properly prescribed drugs can save lives. Yet, do these drugs give us the best odds? They do not.
All of this begs a question. Does the brouhaha caused by coronavirus not pale in comparison to the millions of lives lost to drugs? Of course, I believe in finding a cure. Nevertheless, when this pandemic subsides, should we not first look at ways to stop death due to prescription? There are better ways to prevent and cure illnesses, and the people must be educated. Knowledge not disseminated is no better than no knowledge at all.
An illustration of a better way than prescription drugs to stop death by diseases—diabetes and other maladies
An example: 2/3 of diabetics who attended our resort were able to stop medications in 11.7 days because of nutrition. In addition, of course, they soaked up the sun. Also, 85% of those who stayed for four weeks were able to leave without the meds. The avoided meds included injected insulin and hypoglycemic drugs (Metformin, Glucotrol, etc.]. That seems like a better option than another drug to “prevent” death. Of course, people must be willing to make changes to heal themselves. Avoiding death is unlikely if a person would rather die than part with junk food. The people at our resort liberated themselves from drugs by making the right choices.
And what about death from other diseases?
Diabetes, of course, was only one of myriad diseases they left behind when they returned home from their sojourns with us. A few others were arthritis, headaches, muscle pain, heart disease, lupus, asthma and obesity. Even erectile dysfunction, mood disorders, endurance and eyesight improved. In addition, nothing we did involved drugs and supplements. Good food, exercise and sunlight were the “medicines” we used. As Hippocrates once stated, “Let Food be your medicine.” He should have added, “Let sunlight and exercise also be your medicine.”
You knew I would get to sunlight and death, did you not?
Another method to enhance human health, while reducing human death: Bring people back into the safe, non-burning sunlight. My latest book, Embrace the Sun, co-authored by Dr. William Grant, has some interesting analyses. There are, in the U.S., according to our calculations, approximately 1,684,677 yearly deaths caused by diseases associated with sun deprivation. That compares to 5125 deaths from diseases associated with high sun exposure, producing a ratio of approximately 328:1. Now you can live with those odds (no pun intended)! Do we really need all those drugs if we give up our killer nutrition and soak up some non-burning sunlight?
Here are some facts everyone should know about death-preventing effects of regular, non-burning sun exposure:
- Seventy-five percent of melanomas occur on areas of the body seldom exposed to sun.
- Women who sunbathe regularly have half the risk of death during a 20-year period compared to those who stay indoors.
- Multiple sclerosis (MS) is highest in areas of little sunlight, and virtually disappears in areas of year-round direct sunlight.
- A Spanish study shows that women who seek the sun have one-eleventh the hip-fracture risk as sun avoiders.
- Women who avoid the sun have 10-times the risk of breast cancer as those who embrace the sun.
- Sun exposure decreases heart disease risk.
- Sun exposure dramatically improves mood.
- Those persons who spend more than 15 minutes outdoors have only 1/50 the risk of Parkinson’s disease!
- For each death caused by diseases associated with sun exposure, there are 328 deaths caused by diseases associated with sun deprivation.
- Sun exposure increases the production of BDNF, essential to nerve function.
- Sun exposure can produce as much as 20,000 IU of vitamin D in 20 minutes of full-body sun exposure.
- In the U.S., vitamin D deficiency in children has increased by 83 times during a 14-year period. That is likely due to indoor living and sunscreen use.
- Sunlight also directly associates with reduced incidence and death from flu. In the next three months, we may determine if it also reduces the incidence of coronavirus. (Chart courtesy of WHO. Sent by Goran Olsson, Moscow, Russia.) Note the incredible increase of flu in seasons of sun deprivation.
Therefore, you see, good nutrition and sunlight can reduce the need for prescriptions and lighten one more death burden. Embrace the Sun.
The phone, sunlight and sound sleep. By Marc Sorenson, EdD. 
The phone is ubiquitous, and it may be taking away a basic human need: sound and restful sleep.
How should the sleep/wake cycle work?
First of all, we awake to bright sunshine. Light enters the eye and stimulates serotonin production. Serotonin is a natural “upper” and mood elevator. Thus, we quickly become awake and invigorated. The bright sunshine also suppresses melatonin, the sleep inducer. Yet at evening light disappears (at least that is how nature intended it), melatonin levels rise, and serotonin levels diminish. We begin to feel sleepy and ideally retire for a good night’s rest. It is a perfect system for our needs—unless we stay up beyond biologically natural hours by using artificial lighting.
Then, the phone throws a wrench into the works!
Particularly, a phone, tablet, computer monitor and other electronic device that emits blue light can interfere with sleep cycles. This may leave you wide-awake and staring at the ceiling when you should be sleeping peacefully. Furthermore, you may feel “out of sync” the next day due to lack of rest. We hear a plethora of advice about using blue-blocker screens, and heaven forbid, giving up the devices at night! Regrettably, however, some humans would rather die than not check their devices just before, and many times during, bedtime. Perhaps they are incorrigibly addicted to the phone, tablet, etc. In addition, such activities inhibit melatonin secretion. Best to eschew the phone by night and embrace the sun by day!
So, is there any way to cater to our phone addictions and still get some shut-eye?
An interesting study showed that exposure to constant bright light, for several hours daily, stopped sleeplessness and let melatonin dominate at night. The researchers compared subjects reading a book (no blue light) and a tablet (lots of blue light). They also assessed sleep patterns and melatonin concentrations. Both groups had identical results for melatonin and sleep patterns. From this research, it appears that we can have our cake and eat it too, provided we receive plenty of sunlight. Most noteworthy was that it was not lack of blue light (when the devices were removed) that enhanced sleep. Rather, it was the bright light exposure in the day. Hence, we can evade sleep-deprivation punishment for  excessive device use if we take our time in the sunlight!
excessive device use if we take our time in the sunlight!
So is there other research indicative of the night-time-sleep-inducing effects of daytime sun exposure?
There are several. For a full discussion, I suggest you read my book, Embrace the Sun, co-authored by Dr. William Grant.
Another investigation established that people whose workplaces have windows are able to sleep about 46 minutes per night longer on average, than those who have no natural light access. Those with windows also are generally happier, have fewer ailments, and experience better vitality than their window-less counterparts.
Why is sleep so important to health, regardless of cell phone, sunlight, etc.?
Another article shows that too little sleep can be deadly. Forbes Magazine online printed an excellent article on sunlight and sleep, which listed the following horrendous statistics: “In 2012, 60 million Americans filled prescriptions for sleeping pills, up from 46 million in 2006.” The article discusses the potential dangers of sleep medications, showing that those who take 18 sleeping pills per year have a tripling of the risk of death compared to those who take fewer than 18.
Do not expect the drug companies to be touting these stats. Take matters in your own hands and get some daily, non-burning sun exposure. In addition, read Embrace the Sun,
Sunbeds can be healthful devices. By Marc Sorenson, EdD.

Sunbeds, also known as tanning beds, have many healthful properties. They produce vitamin D, strengthen bone and reduce the risk of major cancers. Yet, sunbeds are much maligned as being a major cause of melanoma. Thus, teens in many areas have been banned from using them by misguided legislation. In addition, tanning- salon owners must live in fear of government overreach that could put them out of business.
But new research shows that the attack on sunbeds is misguided.
Because of this uproar, a group of scientists (some dermatologists), led by Dr. Jörg Reichrath, did a thorough research review. Furthermore, they published their findings in the scientific journal Anticancer Research, which presented truth about melanoma and sunbeds. This information is most noteworthy since it is contrary to the prevailing papers that emanate from the Powers of Darkness. The Powers of Darkness are those who love to attack both sun exposure and sunbeds.
Especially relevant points regarding sunbeds and melanoma risk, from Anticancer Research:
- First of all, Reichrath and colleagues performed a systematic literature search. This research was undertaken to identify and evaluate research that investigated relationship of solarium use (sunbed use) and melanoma risk. And as a result, they stated the following: “We found no studies that demonstrate a causal relationship between moderate solarium use and melanoma risk.” In addition, they indicated that the quality of the observational studies was low and that bias may have existed.
- Another interesting finding was that although moderate sunbed use had no effect on melanoma, something else did affect melanoma. An unhealthy lifestyle involving extensive sunbathing, alcohol and smoking associated to a 20% increase in the disease. Also, the researchers mention that individuals with unhealthful lifestyles use tanning salons more often.
At this time, I must make a point. Those who are regularly in the sun have stronger bones and less cancer than sun avoiders. So I’m not sure what “extensive” sunbathing entailed. And, another point is this: As time spent in the sun has decreased profoundly in both Europe and the U.S., melanoma has increased exponentially. Read my book, Embrace the Sun, to see the discussion on this topic.
Could sunbeds actually decrease the risk of melanoma?
Another salient finding of the research review: A study from Europe showed that sunbed use was associated with a 30% reduced risk for developing melanoma. Reichrath and colleagues made this comment on that study: “Those findings indicate that solarium [sunbed] use may even have a protective effect.”
Sunbeds: beyond melanoma. Here are a few truths about sunbeds that are seldom discussed:
The transcendent sunbed study showed that during 20-years, women who used them reduced all-cause mortality by 23%. So let’s suppose that that there were some health problems with using sunbeds. That negative possibility pales in comparison to the remarkably reduced risk of death, does it not? And, I am not stating that there were negatives for sunbed use in this research.
What are some of the reasons that sunbed use is associated with a lower risk of all cause death?
Another investigation showed that sunbeds were associated with a reduced the risk of breast cancer.
In addition, research showed that sunbeds were associated with 90% higher vitamin D levels and significantly stronger bones.
Also, they are useful in treating psoriasis and other skin disorders.
Sunbeds are also useful in treating pain and in improving mood.
Finally, these devices have been shown to associate with lower clot risk.
The takeaway from all of these studies is that there is no credible research that melanoma is increased by using sunbeds. And, sunbeds have remarkably healthful effects. When receiving sun exposure or using sunbeds, be sure not to burn.
Happy sunning!
For more information, read the book, Embrace the Sun.
Sunlight or vitamin D or both? By Marc Sorenson, EdD.
Sunlight or vitamin D? That is a question that should not be necessary, yet many believe that vitamin D replaces sun exposure. So, they will state, “just take some vitamin D pills rather than go out in the sunlight, thus, you can derive sunlight benefits without the risk of skin cancer.” This opinion is incorrect, and it leads to sun deprivation.

This poor opinion of sunlight is misguided, erroneous and dangerous.
First of all, sunlight leads to production of many photoproducts when it touches the skin or enters the eyes. (Do not stare into the sun, since sufficient sun enters the eyes by reflection from objects or from the sky). These photoproducts include serotonin, endorphin, vitamin D, dopamine, brain-derived neurotropic factor (BDNF) and nitric oxide.
Furthermore, all of these sunlight photoproducts are known to have healthful effects.
In addition, there are more photoproducts that are produced by sun exposure, but they have not yet been well-studied. Yet, it is likely that all of them will be found to have salubrious effects for the human body. Hence, we need them all. Obviously, a vitamin D pill cannot provide all the health benefits that sunlight provides.
Vitamin D in isolation may not always be healthful. Consider sunlight instead.
So yes, vitamin D is an important photoproduct of sunlight, but it is just one of the photoproducts. Thus, it is along for the ride with its companions. The serum blood tests which measure vitamin D are really surrogate measures for sunlight exposure and its other photoproducts. And, these photoproducts work as a team; one might say a “holistic” team.
Sunlight or vitamin D. What does the vitamin D research tell us?
A surprising piece of recent research assessed the efficacy of vitamin D supplementation on bone strength and density. The researchers worked with 311 healthy volunteers aged 55 to 70 and these volunteers were split into three groups. One group received 400 international units (IU) per day of vitamin D, and a second group received 4,000 IU per day. Finally, a third group received 10,000 IU per day. Bone strength and density were measured at the beginning of the investigation and at intervals of 6, 12, 24 and 36 months. The researchers had thought there would be an increase in bone mass, yet, the results were opposite of their expectations. Stunningly, all three groups lost bone mass, and the higher the vitamin D dose, the more rapid the bone loss!
How can this happen? Does sunlight exposure play a part?
So, we have an interesting dichotomy here. First of all, we see that isolated vitamin D (the supplements) were counterproductive for bone strength and mass. And yet, we know that low serum levels of vitamin D are associated with low bone density. Maybe we can unravel this mystery by mentioning that almost all serum vitamin D (about 90%) is produced by sun exposure on the skin.
Therefore, low vitamin D levels are really indicative of sunlight deprivation.
And as aforementioned, one isolated chemical (vitamin D), cannot possibly be expected to take the place of the holistic sun. Especially relevant is a study that found Spanish women who sunbathed had 1/11 the fracture risk of indoor women. Is there any doubt that the strong-boned women had higher vitamin D levels than their counterparts? You see, we have gotten it backward, because greater sun exposure associates with higher vitamin D levels and predicts long life and health. Sunlight leads to vitamin D production, but vitamin D does not bring sunlight and all its additional photoproducts.
Does vitamin D supplementation protect against cardiovascular disease (CVD), or is it sunlight?
We know the answer to half of that that question due to a study of more than 83,000 people. And this study was a meta-analysis. This means a compilation and analysis of the best supplementation studies. The study compared vitamin D intake with CVD events (heart attacks, stoke, death from CVD and all-cause death). The authors found, as a result, that vitamin D supplementation was not associated with CVD.
Most noteworthy is that for years, sunlight was shown to associate to a much reduced risk of CVD.
And, that included heart attack and stroke.
Many made the mistake of giving the credit for the reduced risk to vitamin D, because of this research.The answer to health is to embrace the holistic sun and not a single photoproduct.
Sunlight related to the beta carotene study
This reminds me of research on beta-carotene, an antioxidant nutrient found in orange and yellow vegetables such as carrots. Since these vegetables have healthful properties, the researchers decided to experiment with isolated beta-carotene. They wanted determine if beta-carotene also had anti-cancer properties. To their dismay, these experiments associated to an increase in cancer. Does isolated vitamin D lead to the same deleterious outcomes? Sunlight should also be used in its whole form, just like the carrot.
So in the winter, in climes where there is little sunlight, how do we get our share of life-saving light?
The best method is to use a good sunbed (tanning bed), and when the sunlight is available, to be outside enjoying it, summer and winter. Sunbed use has many life-enhancing effects, including longer life, stronger bones and better mood. Read more about sunbeds, sunlight, bone strength and health at http://sunlightinstitute.org/ and read the book by Sorenson and Grant: Embrace the Sun.
Happy sunning! And remember never to burn.
Protect the children with sunshine. By Marc Sorenson, EdD.

Protect the children against illness? That is a great idea, and sunshine is one of the most effective “protectors” we can use.
“Children and arthritis” is not something we hear about because arthritis is thought to be an adult’s disease. Yet tragically, an estimated 294,000 children under age 18 have some form of arthritis or rheumatic condition. And this represents approximately 1 in every 250 children in the US.[1] Thus, we must be concerned and promote actions that protect the children.
Do we need to be even more concerned to protect the children in northern climes?
Also, the numbers of children with arthritis increase dramatically In Canada and the Northern U.S. This could be as a result of either vitamin D deficiency or sunlight deficiency or both. Since 90% of vitamin D blood levels are due to sunlight, it is likely that sun deprivation is the cause. So, if our desire is to protect the children, we must insist that they receive plenty of non-burning sun exposure. And in the winter, a vitamin-D producing sunlamp should be the first choice. When we use lamps to produce vitamin D, we also protect the children with other critically important photoproducts. Some of these photoproducts are endorphins, serotonin, nitric oxide brain-derived neurotropic factor (BDNF), dopamine and endorphin. And all of these photoproducts are necessary for health. So, to help the children, we should be sure that they have ample sunshine or light for the aforementioned sun lamps.
Articles from the UK and scientific journals help us to protect the children.
An article from the Express, a UK online newspaper, describes research published in the scientific journal, Annals of the Rheumatic Diseases. They state, “Millions of people could protect themselves from crippling arthritis by getting a regular dose of sunshine.” And although the research involved women, we can easily extrapolate to children, since mothers to a great extent, determine their children’s habits.
To learn more about arthritis and the influence of sun exposure, read this article (and others) posted on Sunlight Institute. First of all, go to the news section and search “arthritis.” You will find numerous articles on the subject. Also, read the book, Embrace the Sun.
Remember to obtain regular sun exposure to protect yourself
and to protect the children. Happy sunning!
[1] Centers for Disease Control and Prevention: arthritis-related statistics.









 d early fall, when I mostly worked on my father’s ranch. The sun blazed from dawn to dusk and I soaked it up. The work on our ranch was intense. We started those sunny days with morning feeding of animals, followed by irrigating, hauling hay and performing other outdoor tasks. Despite the long hours, I loved the sun, and it made the hard work worthwhile. Whenever possible, my shirt came off, and because of my deep tan, my friends called me “brown man.”
d early fall, when I mostly worked on my father’s ranch. The sun blazed from dawn to dusk and I soaked it up. The work on our ranch was intense. We started those sunny days with morning feeding of animals, followed by irrigating, hauling hay and performing other outdoor tasks. Despite the long hours, I loved the sun, and it made the hard work worthwhile. Whenever possible, my shirt came off, and because of my deep tan, my friends called me “brown man.”