A new study,[1] from the European Journal of Medicinal Chemistry, reports that synthesized chemicals that mimic those found occurring naturally in broccoli, cauliflower and other cruciferous vegetables, have the ability to inhibit melanoma. The synthesized chemicals, in fact, were able to inhibit the growth of melanoma cells by about 70% in an experiment on mice.
My last blog showed that tomato powder also had the ability to cut the risk of melanoma by 50% in another mouse experiment, and other studies have also shown that fruits and vegetables have important anti-cancer effects. So when we talk about the reasons that melanoma has increased so rapidly, despite the best efforts by the sunscreen industry and the anti-sun movement, we know many reasons that are backed by science: Lack of regular sun exposure, alcohol consumption, milk consumption and lack of fresh fruits and vegetables in the typical modern nutrition program.

Other investigations have studied the relationship between melanoma survival and fruit consumption.[2] Melanoma patients who had their cancers removed—and who had a predicted death rate of 40% within 10 years—were assessed for consumption of fruit and red meat. Daily fruit consumption correlated to a reduced risk of death of 46%. Those who ate red meat at least once weekly showed an increased risk of death of 84%.
Eat your vegetable and fruits, eschew the meat and most other animal products, obtain regular, non-burning sun exposure, forget the alcohol and milk products and enjoy many outdoor activitiesin natural surroundings. Many of these factors will be discussed in my forthcoming book, Embrace the Sun.
Enjoy the outdoors!
[1] Deepkamal N. Kareliaa, Ugir Hussain, Parvesh Singh, A.S. Prakasha Gowdad, Manoj K. Pandey. Srinivasa R, Ramisettia. Shantu Amin, Arun K. Sharma. Design, synthesis, and identification of a novel napthalamide-isoselenocyanate compound NISC-6 as a dual Topoisomerase-IIα and Akt pathway inhibitor, and evaluation of its anti-melanoma activity. European Journal of Medicinal Chemistry 135;28:282-295.
[2] Gould Rothberg BE, Bulloch KJ, Fine JA, Barnhill RL, Berwick M5. Red meat and fruit intake is prognostic among patients with localized cutaneous melanomas more than 1 mm thick. Cancer Epidemiol. 2014 Oct;38(5):599-607.
Teen tanning by Marc Sorenson, EdD….
“There are lies, damn lies and statistics,” or so the saying goes. Karen Selick, of the Canadian Constitution Foundation, some time ago penned a press release entitled: Don’t outlaw teen tanning.[1] I was fortunate that a friend thought I’d be interested. He sent me the release, even though the release was published in 2013.
Selick’s discussion gives an excellent explanation of how the twisting of statistics may lead to a total misinterpretation of the truth. She discusses the fact that anti-tanning advocates consistently state that using indoor tanning equipment before the age of 35 results in a 75% increase in the risk of developing melanoma. That does sound frightening, but when the figures are looked at more closely, she explains that the actual risk of young people contracting melanoma is almost negligible.
Her reasoning is brilliant. She consulted the Statistics Canada Causes of Death database, and demonstrates that in the decade from 2000 to 2009, the last decade from which statistics for teens were available, 5 Canadians 19 years of age or younger died from melanoma. In other words about a half-person per year.
She also points out that among teens during that same decade, there were 195 deaths from falls, 627 deaths from drowning and 6,972 from “transport accidents.”
To draw an analogy, Ms. Selick states the following: “……….. suppose that only one person in Canada were to be murdered in 2014. If two people were murdered in 2015, that would constitute a shocking 100 percent increase in the murder rate — but it would still be only two people, an extraordinarily low murder rate for a country of 34 million people.”
Another observation from the press release was a comparison of the risk of heart disease in Scotland, where sunlight is scarce, with Australia, where sunlight is abundant. The Australians have a one-third reduced risk of death rates from heart attacks. Ms. Selick’s release states that “Those who would ban teen tanning focus so intently on skin cancer that they seem completely oblivious to the health benefits that sun exposure (real or simulated) can confer.”
I have mentioned in this blog that there are 324 lives lost from diseases that are associated with sun deficiency for every life lost to diseases associated with sun exposure, and since sunbeds produce the same type of light as sun exposure, it is not surprising that sunbeds have healthful effects.
We also now have research that demonstrates that over 20 years, women who use sunbeds have a 23% reduced risk of all-cause death.[2]
Dr. Richard Weller, a dermatologist and the author of many pro-sun research studies, often discusses the beneficial effect of nitric oxide, a photoproduct of sun and sunbed exposure. He makes a compelling case that nitric oxide dramatically reduces the risk of hypertension and heart disease. Here is one of his statements:
“The prevalence of cardiovascular and cerebrovascular deaths is around 100 times higher than those from skin cancer. Interventions leading to small changes in the incidence of cardiovascular disease are thus of greater benefit to the health of the public even than large changes in skin-cancer incidence.”[3]
I am not here to suggest that you use a sunbed. That is up to you. I have my own sunbed and enjoy it without the least worry. Just be sure that when you use a sunbed or engage in sunbathing, do it safely without burning.
[1] http://www.huffingtonpost.ca/karen-selick/skin-cancer-tanning-beds_b_2744788.html
[2] Lindqvist PG, Epstein E, Landin-Olsson M, Ingvar C, Nielsen K, Stenbeck M, Olsson H. Avoidance of sun exposure is a risk factor for all-cause mortality: results from the Melanoma in Southern Sweden cohort. J Intern Med. 2014 Jul;276(1):77-86.
[3] Weller R. The health benefits of UV radiation exposure through vitamin D production or non-vitamin D
Pathways. Blood pressure and cardiovascular disease. Photochem. Photobiol. Sci. 2016, DOI: 10.1039/C6PP00336B.
Tanning bed use, By Marc Sorenson, EdD. Sunlight Institute.
Sun exposure and tanning-bed exposure have been much maligned by those who would increase sunscreen sales and other “protection” against melanoma. So a new paper has been written regarding the truth about tanning beds. According to this paper, Risk of melanoma with tanning beds is slightly associated with home use, but there is no significant increase in risk with beds used in tanning salons. This is according to a soon-to-be-published analysis of studies that differentiated between home-use tanning beds and salon use of tanning beds.[1]
The analysis showed that when all tanning devices were considered together, tanning bed use was associated with a 15%-20% increased risk of melanoma. However, when home-use tanning was separated from salon use, salon use showed only a 5% increased risk, which was not significant. In other words, there may have been no risk whatever. In fact, in three of the studies that were part of the analysis, overall use of tanning beds associated to a lessened risk of melanoma.
Therefore, if there is any increased risk of melanoma with tanning-bed use, it is all due to the use of home units. This is what we might expect, since salons take care to assess skin type and monitor the time spent in the unit.
Before we decide to eschew the use of home units, however, we should also take into consideration the very healthful benefits of tanning-bed use in general. Here are a few well-documented facts about the benefits:
- Tanning bed use is associated with a reduced risk of clots.[2]
- Tanning-bed use is associated with increased vitamin D levels.[3]
- Tanning-bed use is associated with stronger bones.[4]
- Tanning-bed use can cure psoriasis and eczema and tanning beds are often recommended by dermatologists.[5]
- Tanning-bed use more than three times yearly is associated with a 40-50% reduced risk of endometrial cancer.[6]
- Tanning-bed use is associated to lower breast-cancer risk.[7]
- A 20- year study demonstrated that both sun exposure and tanning-bed exposure reduced the risk of death; women who used tanning beds were 23% less likely to die of any cause than women who did not use them.[8]
The key to safe tanning-bed use is the same key as for safe sun exposure: Don’t be taken in by the anti-sun, anti-tanning movement.
[1] Hoel, D. Commercial Tanning Salons and Melanoma Risk. Letter to the editor, Dermato-endocrinology. Not yet published.
[2] Lindqvist PG, Epstein E, Olsson H. Does an active sun exposure habit lower the risk of venous thrombotic events? A D-lightful hypothesis. J Thromb Haemost. 2009 Apr; 7(4):605-10.
[3] Holick, M. Boston University. “Effects Of Vitamin D And Skin’s Physiology Examined.” Science Daily 21 February 2008 <http://www.sciencedaily.com¬ /releases/2008/02/080220161707.htm>.
[4] Tangpricha V, Turner A, Spina C, Decastro S, Chen TC, Holick MF. Tanning is associated with optimal vitamin D status (serum 25-hydroxyvitamin D concentration) and higher bone mineral density. Am J Clin Nutr 2004;80:1645-49.
[5] Radack KP, Farhangian ME, Anderson KL, Feldman SR. A review of the use of tanning beds as a dermatological treatment. Dermatol Ther (Heidelb). 2015 Mar;5(1):37-51.
[6] Epstein E, Lindqvist PG, Geppert B, Olsson H. A population-based cohort study on sun habits and endometrial cancer. Br J Cancer. 2009 Aug 4;101(3):537-40.
[7] Yang L, Veierød MB, Löf M, Sandin S, Adami HO, Weiderpass E. Prospective study of UV exposure and cancer incidence among Swedish women. J Intern Med. 2014 Jul;276(1):77-86
[8] Lindqvist PG, Epstein E, Landin-Olsson M, Ingvar C, Nielsen K, Stenbeck M, Olsson H. Avoidance of sun exposure is a risk factor for all-cause mortality: results from the Melanoma in Southern Sweden cohort. J Intern Med. 2014 Jul;276(1):77-86.
By Marc Sorenson, EdD. Sunlight Institute…
Most people believe that melanoma incidence is increasing rapidly, and that complete avoidance of sun exposure is the answer to preventing the disease. And of course, we must always wear sunscreen, even in the winter. Occasionally, however, there are research studies that belie those beliefs and quite simply show that sunscreens are at best worthless and at worst toxic.
A very-well-done piece of research in Northern Europe compared melanoma incidence rates with sunscreen use during a period of time from 1997-1999 to 2008 and 2012.[1] One of the most interesting findings was that higher income people had significantly higher melanoma incidence, and that increased sunscreen use by those people had not prevented them from being at higher risk of melanoma. In other words, we see this equation: Higher sunscreen use=higher melanoma risk! We know that people who work outdoors regularly have far less risk of melanoma than those who work indoors.[2] This research backs that fact, because it is obvious that higher-income people spend much more time indoors that poorer people who work outside. Those higher-income people also have more money to spend on sunscreens.
Possibly one of the most profound assessments of sunscreen use and melanoma risk was done by Case Adams, a naturopath. In an article entitled Melanoma Rates Double as More Use Sunscreen, Fewer Sunbathe,[3] he analyzes sunscreen sales statistics from Prezi market analysis. He then demonstrates that sunscreen sales between 1982 and 2012 increased by 38 times or 3800%. During the same years, melanoma risk doubled! He also notes that the number of people who sunbathe has profoundly decreased. Anyone who thinks that increasing sunscreen use has led to a reduction in melanoma is wandering around in the darkness of denial! Dr. Adams also makes this interesting statement: “Thus we cannot logically equate the growth of skin cancer with an increase in sun exposure.”
The best protection against melanoma is regular sun exposure. Safely enjoy it!
[1] Williams SN, Dienes KA. Sunscreen Sales, Socio-Economic Factors, and Melanoma Incidence in Northern Europe: A Population-Based Ecological Study. SAGE Open December 14;1-6.
[2] Garland FC, White MR, Garland CF, Shaw E, Gorham ED. Occupational sun exposure and melanoma in the USA Navy. Arch Environ Health 1990; 45:261-67.
[3] http://www.realnatural.org/melanoma-rates-double-as-more-use-sunscreen-fewer-sunbath/
By Marc Sorenson, EdD. Sunlight Institute…
This Blog is meant neither to promote the use of tanning beds nor to discourage such use; rather, it is designed to balance the message. Seldom is anything positive said about tanning beds, although there is research that shows many positive benefits; such research is usually ignored because it does not conform to a preconceived notion. We therefore want to present some of that research to demonstrate that there are other opinions that provide some balance to the messages. You, the reader, can then make up your mind based on the research. Knowing the entire truth about any subject is important prior to making up one’s mind regarding that subject.
Sun exposure and tanning have been vilified by many (but not all) dermatologists. Tanning beds have been demonized to an even greater degree and are called “cancer machines” by many in the medical profession and in the popular press. There are movements afoot to make it illegal for those under the age of 18 to even use them, which is woefully misguided and ill-advised. Every beneficial effect of vitamin D that is produced by sun exposure is also produced by the use of high-quality tanning beds, and endorphins and nitric oxide are also produced, just as with the sun. The following is a list and discussion of tanning-bed benefits.
- Many so-called experts have said that tanning beds do not create higher vitamin D levels, but the research belies that falsehood. In a study that compared 50 subjects who used a tanning bed at least once weekly to 106 control subjects who did not use tanning beds, it was shown that tanning-bed users had 90% higher vitamin D levels than non-users, and they also had significantly higher bone-mineral density, indicative of stronger bones.[1] Parathyroid hormone (PTH) levels were also taken and were 18% lower among the tanners. High PTH levels are often associated with weak bones and low vitamin D levels. The researchers compared dark-skinned people with Caucasians and found that tanning-bed sessions increased vitamin D levels almost identically in both ethnic groups.[2]
I am part of an email list of scientists and researchers who are intensely interested in sun research, and who share articles on sun and vitamin D. I received a most interesting email from Rufus Greenbaum, who lives in the UK and who organizes vitamin D symposiums. He recounted how he had met a man who had used tanning beds twice weekly since 1970, and who had just completed a bone densitometer test, known as a DEXA scan. His doctor stated, “You have the strongest bones that I have ever seen.” That news certainly came as no shock. Conventional tanning beds produce large quantities of vitamin D in short periods of time,[3] and vitamin D is absolutely essential for optimal absorption of calcium in the gut.[4] [5] Without calcium absorption, consuming vast quantities of calcium makes little difference to bone strength; much of the calcium will be flushed down the toilet.
- Tanning beds can cure psoriasis and eczema and are often recommended by dermatologists as a way to overcome these diseases. Some common-sense scientists understand that UV light is nearly 100% effective for many dermatologic conditions, and that tanning beds are very convenient sources of UV for patients who cannot otherwise afford the rigorous travel and time commitments necessary to visit the dermatologist.[6] Their investigation involved an arduous search of PubMed and Google Scholar for papers that reported on tanning beds and their salutary effects on different skin diseases.
The searches showed convincingly that tanning beds were a valid use for psoriasis, but also indicated tanning beds could be useful “as a treatment option for atopic dermatitis [eczema], mycosis fungoides, acne, scleroderma, vitiligo, and pruritus, as well as other UV sensitive dermatoses.”
The conclusion they reached was amazing, considering negative reports that are regularly touted by the press. They stated: “Unsupervised sun exposure is a standard recommendation for some patients to obtain phototherapy. Selected use of commercial tanning beds in the treatment of dermatologic conditions may be another useful and effective treatment for those patients with an inability to access office-based or home-based phototherapy.”[Italics mine]
One of the dermatologists who recommends unsupervised sun exposure as stated above is Dr. Julie Moore of Gottlieb Memorial Hospital. She says that sun is one of the best ways to treat psoriasis, so she recommends that her patients “sit out on the deck and give their affected areas a good sun bath.[7]” Hallelujah! Common sense is beginning to penetrate the dermatology profession, as more dermatologists are climbing on the sun bandwagon each year.
- Whereas a daily 400 IU vitamin D supplement does not maintain healthful levels, tanning bed use increases vitamin D levels by 150% in only seven weeks.
- Tanning-bed use reduces chronic pain.[9] [10] In a study by dermatologists, using persons with fibromyalgia symptoms including pain, those who used UV-producing tanning beds experienced a decrease of .44 points on a scale of pain score when compared to those who did not receive UV light. Feelings of well-being and relaxation were also reported among the tanners.[11]
- Sun lamps are now being recommended for use by pregnant women who will give birth in a winter month. The recommendation is being made to protect the unborn child from osteoporosis during adulthood.[12]
- Research from Sweden demonstrated that women who use tanning beds more than three times yearly, had a reduced risk of endometrial cancer of 40- 50%.[13] The authors surmised that the effects observed were likely due to stimulating higher vitamin D levels in winter.
- Tanning-bed use reduces the risk of clots.[14] In an eleven-year study of the sun-exposure habits venous thrombotic (clotting) events of 40,000 women, it was found that women who sunbathed during the summer, on winter vacations, or when abroad, or used a tanning bed, were at 30% reduced risk of venous thrombotic events compared to those who did not. The authors again speculated that increased vitamin D, which has anticoagulant properties, resulted in these positive results.
- Tanning-bed use is associated to lower breast-cancer risk.[15]
- High quality tanning beds, because they provide UVB to both sides of the body simultaneously, stimulate the production of up to 10,000 IU of vitamin D in less than ten minutes. Ten minutes of tanning bed exposure can be done on a lunch break. That means they are more efficient than summer sun. Of course, those with darker skin will require a longer time to produce the same amount of vitamin D.
- It is likely that all benefits of sun can be provided by tanning beds, including increased resistance to cancer, osteoporosis, heart disease, diabetes, periodontitis, arthritis, infection and other maladies.
- Tanning beds may be used regardless of outside weather.
- Tanning beds may be used during “vitamin D winter.” This is especially important at higher latitudes that lack sufficient UVB from winter sun to stimulate adequate vitamin D production by the skin.
The truth about tanning beds and melanoma
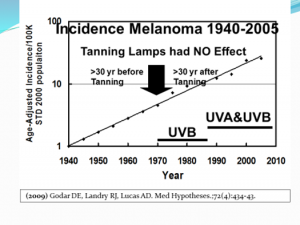
As we have shown, it is impossible to establish sun as the cause of melanoma; yet through chicanery and dishonesty, as established by Dr. Ackerman, we continue to see that the desire for profit produces chicanery, dishonesty and hypocrisy, which leads to the continuing mantra of the anti-sun movement—that melanoma is caused by our friend, the sun. That mantra is ludicrous, and the purveyors of the message are beginning to sound silly. We expect that due to the worry that the sun/melanoma message is ready to crash and burn, these same people are now attacking the tanning industry. One of the claims is that since the advent of tanning beds—in about 1970—melanoma has increased dramatically. While that is true, it has nothing to do with tanning beds. Melanoma was increasing steadily and exponentially long before tanning beds hit the scene and that rate of increase was not influenced by tanning beds. Dr. Diane Godar has produced a graph showing that tanning beds made no difference at all in the increase in melanoma. You will note that the rate of increase in melanoma is exactly the same now as it was since 1940. Dr. Godar’s graph is presented below.
Those who oppose the use of tanning beds can conveniently ignore the rate of increase prior to the first tanning beds to make it appear that the tanning bed is the culprit. This is intellectual dishonesty, and it reminds me of the old saying, “There are lies and damn lies, and then there are statistics.” Twisting or ignoring the facts should be criminal.
Several studies have investigated the relationship of tanning-bed use to melanoma and a review of 22 investigations done from 1979 through 2002 showed that only four indicated tanning beds increased melanoma risk; eighteen showed no association.[16] One that showed an increased melanoma risk was conducted by Dr. Philippe Autier and colleagues in Belgium in 1991.[17] However, in 2002 Dr. Autier conducted another study in which no association between tanning bed use and melanoma was found.[18] This report stated, “No result suggested a dose-response curve, and no association was even present for subjects who reported more than 35 hours of cumulated tanning-bed use at least 19 yrs. before the interview. Our study doesn’t support the possibility that tanning bed use could increase melanoma risk.”
I looked for other studies that might have come to contrary conclusions and found one from 2007.[19] It was a meta-analysis of 19 studies that concluded tanning beds do increase the melanoma risk. However, when Dr. Grant assessed the meta-analysis, he noted that the studies failed to take skin type into consideration.[20] He re-analyzed the data and determined: “These results indicate that when studies largely influenced by inclusion of people with skin phenotype 1 [light-skinned non-tanners] without adjustment for skin phenotype are removed from the meta-analysis, no significant relation is found between tanning bed use and risk of CMM [cutaneous malignant melanoma].”
Several studies between 2003 and 2008 showed mixed results. One showed no significant increase in melanoma with tanning bed use.[21] Another study of five European countries showed that in France, where 20% of the population used tanning beds, their use was associated with a 19% increase in risk of melanoma.[22] In Sweden, where 83% of the population used tanning beds, there was a 38% decrease in melanoma. Overall, the risk of melanoma was reduced by 10% in tanning-bed users, although individuals with fair skin and a high number of moles were at increased risk. Clearly, studies that indict tanning beds, without taking into consideration skin type are flawed, and if they do not also differentiate between tanning and burning, they are doubly flawed.
Remember that excessive ultraviolet light exposure, whether it comes from sun or tanning lamps, causes burning. We have clearly established that burning may correlate to an increased risk of melanoma. Unfortunately, most of the studies that associated tanning beds with increased melanoma did not control for burning. Use of either sun exposure or tanning beds must be done prudently, so it is best to use professional tanning salons with trained personnel who assess skin type and make recommendations for the maximum time clients should tan.
Dr. Grant also reminds us that UVB is the most beneficial wavelength. UVA does have health benefits, including stimulating the production of nitric oxide, but excessive UVA is harmful in that it penetrates more deeply and generates free radicals that can lead to skin aging and DNA damage, as several studies have shown.[23] [24] [25] However, the tan produced by UVA serves as a protection against damage by further UVA. It is important to use tanning beds with outputs that mimic the midday, mid-latitude spring-and-summer UVB portion of total UV—roughly 3.5-5%. European countries limit UVB emitted from tanning beds to 1.5% of total UV radiation[26] [27]—a huge mistake. Tanning beds in the USA emit a much higher percentage of UVB, about 5% on average.[28] Prior to 1983, tanning beds used in Norway and Sweden were rich in UVB and there was no association between tanning-bed use and melanoma. Both the lamps and the acrylic sheet between the lamps and the person affect the UVB/UVA ratio; the acrylic, as it ages, decreases the UVB transmission more than UVA.
Personally, I have no qualms about using tanning beds, but I am not telling you to do the same. Read all the facts and then make up your own mind. Considering the numerous health benefits from high serum vitamin D levels and the production of endorphins, nitric oxide and other photoproducts, the slightly increased chance of rarely-fatal common skin cancer does not concern me.
A very light skin that does not tan, or a skin condition that is sensitive to UV may preclude tanning-bed use by some individuals. Those with freckles and red hair do not generally tan well, and should avoid tanning beds or limit themselves to very short exposures. In addition, it is a good idea to cover the face and genitals as those areas may be excessively sensitive to ultraviolet light. Others who may have adverse effects to tanning bed exposure are organ transplant recipients, those with many nevi (moles) or those taking photosensitive prescription drugs.[29] If you do not know if your drug is photosensitive, ask a pharmacist. Avoid even the least amount of burning.
Finally, it is a good idea to be checked regularly by a dermatologist to assess any changes that may occur to your skin. That advice, however, is even more important for those who do not use tanning beds or get regular sun, since more melanomas occur among those who receive little or no UVB, or in those irregularly exposed. In some cases, tanning beds may help the physical and mental health of people residing in the far north.
In one instance, tanning beds for Canadian military personnel may be essential to survival. The Canadian armed forces most remote outpost is also the northernmost community on Earth, and its purpose is to gather radio signals and other electronic intercepts from Russia and pass them to military analysts in the South.[30] The sun disappears on October 14 and does no reappear until February 28. During that time, temperatures drop to 5+ degrees below zero, and if the wind blow, the chill factor is incredibly low. The facility is build with most of the comforts of home, including gym facilities, and tanning machines that increase vitamin D levels are considered essential to life. We expect that if anyone were to try to take away those machines, it would cause an insurrection. In the previous blog, it was also mentioned that scientists have suggested the use of tanning beds for psoriasis when they were too far away from the dermatologists’ offices for a convenient visit.[31]
Tanning beds and other sources of ultraviolet light can be of great value to human health if they are used safely; the same can be said about the sun.
Are phototherapy sessions in a dermatologist’s office safe?
As we have indicated, dermatologists and their organizations, with certain refreshing exceptions, promote the idea that both tanning beds and natural sun exposure are detrimental to health. Yet, thousands of dermatologists use UVR light to reduce the risk of many skin diseases. They claim that their UVR exposure is totally safe. That is an blatant example of duplicity at its worst. Recently, Dr. Anne Haas, President of the California Dermatology Society, made an egregiously false statement at a regulatory hearing regarding UVR devices, saying that whereas tanning beds were cancer causers, the UVR devices used in dermatologists’ offices had never been shown to cause any cancer problems. Watch this short video to hear her statement:
Her statement, that there is no evidence UV devices in the dermatologist’s office cause cancer, is deceitful. Here is the truth:
- The light used by dermatologists is the same type of light used in tanning beds.[32] [33]
- The use of phototherapy in the dermatologist offices definitely do lead to an increase in skin cancer.[34] And some of that skin cancer was sufficiently noteworthy that the researchers concluded their study with this warning: “A noteworthy number of NMSC were diagnosed in this Mediterranean population of patients exposed to high-dose UV treatment. A thorough risk-benefit evaluation should always be done before UV treatment and patients should be carefully monitored for skin cancer during and after treatment discontinuation.”[35]
- The National Psoriasis Foundation recommends brief, frequent exposures of sunlight as a therapy and report that 80% of those who do it improve or totally clear psoriasis.[36]
- Many honest dermatologists recommend tanning-bed use to their patients to clear psoriasis. Obviously it is effective for that disease, and if phototherapy in the dermatologist’s office causes skin cancer, what seems to be the problem? Both therapies work. Why deny someone with psoriasis the benefits of a lower cost and possibly easier accessibility to treatment?[37]
So why the deception? The answer lies in money. When scientists such as those in the last quoted paper advocate tanning beds for therapy, it could cost the dermatology industry a fortune.
Your will note in the graph below that melanoma incidence has increased nearly in lockstep with the increase in the number of dermatologists. What a business! Is there any doubt why they don’t want the tanning industry absorbing the money made from their lucrative and expensive office treatments? Think about it.
Now you know a few more facts about sunlight, tanning beds, health and the deception of the anti-sun groups. Let it sink in and then make your own decision abut sun or tanning bed exposure. And while you decide, please consider the calculation I’ve made in my new book to be released soon: For every death caused by diseases that associate with sun exposure, there are about 350 deaths associated with sun deprivation. Which way would you like to bet?
[1] Tangpricha V, Turner A, Spina C, Decastro S, Chen TC, Holick MF. Tanning is associated with optimal vitamin D status (serum 25-hydroxyvitamin D concentration) and higher bone mineral density. Am J Clin Nutr 2004;80:1645-49.
[2] Hakim OA, Hart K, McCabe P, Berry J, Francesca R, Rhodes LE, Spyrou N, Alfuraih A, Lanham-New S. VITAMIN D PRODUCTION IN UK CAUCASIAN AND SOUTH ASIAN WOMEN FOLLOWING UVR EXPOSURE. J Steroid Biochem Mol Biol. 2016 Mar 22. pii: S0960-0760(16)30072-3. doi: 10.1016/j.jsbmb.2016.03.025. [Epub ahead of print] Review.
[3] Grant, W. Personal communication with the author, June, 2006
[4] Heaney RP, Dowell MS, Hale CA, Bendich A. Calcium Absorption Varies within the Reference Range for Serum 25-Hydroxyvitamin D. Journal of the American College of Nutrition 2003; 22: 142–146.
[5] Heaney, R. Vitamin D and calcium interactions: functional outcomes. Am J Clin Nutr 2008;88(suppl):541S–4S
[6] Radack KP, Farhangian ME, Anderson KL, Feldman SR. A review of the use of tanning beds as a dermatological treatment. Dermatol Ther (Heidelb). 2015 Mar;5(1):37-51.
[7] Science News, August 6, 2013. Summer sun good for psoriasis sufferers says Gottlieb dermatologist.
[8] Holick, M. Boston University. “Effects Of Vitamin D And Skin’s Physiology Examined.” Science Daily 21 February 2008 <http://www.sciencedaily.com¬ /releases/2008/02/080220161707.htm>.
[9] Kaur M, Feldman SR, Liguori A, Fleischer AB Jr. Indoor tanning relieves pain. Photodermatol Photoimmunol Photomed. 2005 Oct;21(5):278.
[10] Taylor SL, Kaur M, LoSicco K, Willard J, Camacho F, O’Rourke KS, Feldman SR. Pilot study of the effect of ultraviolet light on pain and mood in fibromyalgia syndrome. J Altern Complement Med. 2009 Jan;15(1):15-23.
[11] No authors listed. Tanning Beds Provide Potential Pain Relief for Fibromyalgia Patients. Wake Forest Baptist Medical Center Press release, 2009.
[12] Bukhari, M. Quoted in London Times April 27, 2008.
[13] Epstein E, Lindqvist PG, Geppert B, Olsson H. A population-based cohort study on sun habits and endometrial cancer. Br J Cancer. 2009 Aug 4;101(3):537-40.
[14] Lindqvist PG, Epstein E, Olsson H. Does an active sun exposure habit lower the risk of venous thrombotic events? A D-lightful hypothesis. J Thromb Haemost. 2009 Apr;7(4):605-10.
[15] Yang L, Veierød MB, Löf M, Sandin S, Adami HO, Weiderpass E. Prospective study of UV exposure and cancer incidence among Swedish women. J Intern Med. 2014 Jul;276(1):77-86
[16] International Smart Tan Network 2006. Research shows no connection between tanning and melanoma: Why this is misunderstood.
[17] Autier P1, Joarlette M, Lejeune F, Liénard D, André J, Achten G. Cutaneous malignant melanoma and exposure to sunlamps and sunbeds: a descriptive study in Belgium. Melanoma Res. 1991 Apr-May;1(1):69-74.
[18] Autier P, Tanning bed use and risk of melanoma: results from a large multicentric European study. Poster at the XVIII International Pigment Cell conference held 9-13 September 2002 at Egmond The Netherlands.
[19] International Agency for Research on Cancer Working Group on artificial ultraviolet light (UV) and skin cancer. The association of use of tanning beds with cutaneous malignant melanoma and other skin cancer: a systematic review. Int J Cancer 2007;120:1116-22.
[20] Grant, W. Insufficient evidence exists to link tanning bed use to risk of melanoma for other than those with skin phenotype 1. Sun, Nutrition and Health Research Center ( SUNARC). March 9, 2007. www. SUNARC org.
[21] Clough-Gorr KM1, Titus-Ernstoff L, Perry AE, Spencer SK, Ernstoff MS. Exposure to sunlamps, tanning beds and melanoma risk. Cancer Causes Control. 2008 Sep;19(7):659-69.
[22] Bataille V, Boniol M, De Vries E, Severi G, Brandberg Y, Sasieni P A multicentreepidemiological study on sunbed use and cutaneous melanoma in Europe. Eur J Cancer 2005;41:2141-49.
[23]Garland CF, Garland FC, Gorham ED. Epidemiologic evidence for different roles of ultraviolet A and B radiation in melanoma mortality rates. Ann Epidemiol. 2003;13:395-404.
[24] Moan J, Dahlback A, Setlow RB. Epidemiological support for an hypothesis for melanoma induction indicating a role for UVA radiation. Photochem Photobiol. 1999;70):243-7.
[25] Moan J, Porojnicu AC, Dahlback A, Setlow RB. Addressing the health benefits and risks, involving vitamin D or skin cancer, of increased sun exposure. Proc Natl Acad Sci U S A. 2008;15;105(2):668-73.
[26] Grant, W. Insufficient evidence exists to link tanning bed use to risk of melanoma for other than those with skin phenotype 1. Sun, Nutrition and Health Research Center (SUNARC). March 9, 2007. www. SUNARC org.
[27] Autier P. Perspectives in melanoma prevention: the case of tanning beds. Eur J Cancer 2004;40:2367-76.
[28] Grant W. Insufficient evidence exists to link tanning bed use to risk of melanoma for other than those with skin phenotype 1. Sun, Nutrition and Health Research Center (SUNARC). March 9, 2007. www. SUNARC org.
[29] Grant, WB. Personal communication with author.
[30] Matthew Fisher at CFS Alert: Canada’s “frozen Chosen” at top of the world have been in the dark since Oct 14. National Post February 2, 2013.
[31] Radack KP, Farhangian ME, Anderson KL, Feldman SR. A review of the use of tanning beds as a dermatological treatment. Dermatol Ther (Heidelb). 2015 Mar;5(1):37-51.
[32] Archier E1, Devaux S, Castela E, Gallini A, Aubin F, Le Maître M, Aractingi S, Bachelez H, Cribier B, Joly P, Jullien D, Misery L, Paul C, Ortonne JP, Richard MA. Carcinogenic risks of psoralen UV-A therapy and narrowband UV-B therapy in chronic plaque psoriasis: a systematic literature review. J Eur Acad Dermatol Venereol. 2012 May;26 Suppl 3:22-31.
[33] Radack KP, Farhangian ME, Anderson KL, Feldman SR. A review of the use of tanning beds as a dermatological treatment. Dermatol Ther (Heidelb). 2015 Mar;5(1):37-51.
[34] Egeberg A, Thyssen JP, Gislason GH, Skov L. Skin cancer in patients with psoriasis. J Eur Acad Dermatol Venereol. 2016 Mar 2. doi: 10.1111/jdv.13619. [Epub ahead of print].
[35] Maiorino A, De Simone C, Perino F, Caldarola G, Peris K. Melanoma and non-melanoma skin cancer in psoriatic patients treated with high-dose phototherapy. J Dermatolog Treat. 2016 Jan 28:1-5. [Epub ahead of print].
[36] National Psoriasis Foundation web site Oct. 2005.
[37] Radack KP, Farhangian ME, Anderson KL, Feldman SR. A review of the use of tanning beds as a dermatological treatment. Dermatol Ther (Heidelb). 2015 Mar;5(1):37-51.
By Marc Sorenson, EdD. Sunlight Institute…
Most of the following Material is excerpted from my upcoming book, Embrace the Sun, which will be available sometime this summer.
The assault on the sun, which has increased in intensity for several decades, is one of the most heinous crimes yet perpetrated on humanity. At the root of this evil is the love of money, as is the case in most instances where large numbers of people are defrauded by business entities in collusion with government and “education.” When these forces combine to use half-truths, outright falsehoods and chicanery that destroy health and shorten lives, are they not engaging in high crimes and misdemeanors? What do we call the crime of taking away another’s life? I am opposed to evil in all its forms, including the theft of sun—a theft that diminishes the mental, spiritual and physical advantages sun brings to mankind. The lies perpetuated by supposedly professional organizations make me ill.
I do not oppose making money in an honest manner. The desire for money, and therefore for a better life, is one of the engines that drives entrepreneurship and leads to the marvelous technologies that we enjoy. But money that derives from lying to the people indicates that evil is at play. When a business finds that one of its products (or messages) is causing harm that could literally lead to disease and death, its first act should be to inform its customers and distributors, and then it should remove the product or message from the market. Regrettably, cover-ups and arguments against such findings are often the norm. The first thought is not “We must warn the people that our product or message is harmful,” but rather, “We must do damage control so that our cash flow is not interrupted.” Indeed, if the product is being unjustly maligned, a vigorous campaign against such malignity should be undertaken; but if the complaint against the product is just, then honesty in correcting the problem or eliminating the product should be the first step.
As regards the sun, it has been assailed from many sides as being the plague of mankind—a devastating scourge that is resulting in a plethora of skin diseases—especially melanoma, that threaten to destroy life on Earth. And despite voluminous research to the contrary, the mantra of those who market sunscreens and (most) of those who treat melanoma remains, “Cover up, avoid sun exposure and never forget to use your sunscreens.” Accordingly, the blood is on their hands; they have a billion-dollar business to support, and the facts be damned.
The anti-sun organizations such as the American Academy of Dermatology (AAD) and the Skin Cancer Foundation (SCF) have been spreading a false message for decades. Their pundits have claimed that the sun is public health enemy number 1 and should be avoided at all costs. They have raised the alarm that melanoma would become the scourge of mankind unless steps were taken to remove the presence of sun exposure from human existence.
Perhaps you will believe that the above statement is outlandish hyperbole. But consider two statements by Wilma Bergfeld, a former president of the AAD, in 1996:
- Melanoma will be the leading cause of cancer death among Americans by 2012.
- Mankind will need to move underground to survive the hazards of sun exposure, namely melanoma.
If you would like to hear the words that emanated from her mouth, view the short video below.
How could anyone believe the propaganda promulgated by Dr. Bergfeld, which is still being pushed by the AAD? Nevertheless, the drumbeat to avoid the sun is having its impact, as death, disease and destruction follows in the wake of its “education” programs.
Let’s consider some truths regarding sun exposure and melanoma.
The Melanoma International Foundation (MIF) states that ultraviolet radiation (UVR) from sun causes melanoma and should be avoided as a detriment to human health.[1] That message is primarily disseminated by (some) dermatologists and their governing bodies (previously discussed), which conveniently ignore the hundreds of scientific investigations associating sun exposure to profoundly better health. The sun performs its miracles by reducing risk for such maladies as breast and prostate cancer, heart disease, osteoporosis and scores of others. The MIF message does not differentiate between strong, intermittent exposure, which can lead to sunburn, and regular, non-burning exposure, such as that received by those who routinely work and recreate outdoors. As you will shortly read, the latter are protected against melanoma.
Concomitantly, a message that opposes the MIF statement is rapidly emerging: sun avoidance, by reducing the body’s production of vitamin D and other beneficial photoproducts, is responsible for a dramatic increase in both degenerative and communicable diseases.[2] In addition, a third view is drawing adherents: that the increase in melanoma incidence is an illusion and an artifact produced by incorrect assessment: the misdiagnosis of benign skin lesions as melanoma.[3]
Nevertheless, melanoma is nothing to trifle with, and any unusual skin lesion should be immediately assessed by a dermatologist. However, since many lesions are benign, yet may nonetheless be misdiagnosed as melanoma, it is a good idea to seek multiple opinions before an excision is performed. Proceeding through a deep and invasive surgery for a harmless lesion is something no one should experience, and the most harmful part of the surgery may be the needless fear that one could have died from a deadly cancer—a cancer that really never existed.
Melanoma accounts for about 9,940 cancer deaths per year in the U.S., making up only a small portion of the total number of cancer deaths per year in the US, estimated to be 589,430.[4] Interestingly, melanoma is most common among men over 50,[5] which makes one wonder why tanning beds are being targeted for extinction by the dermatological societies. Men over 50 hardly fit the demographic that use tanning beds! That demographic is young women. Already we begin to see that there is deception within the organizations that promote sun avoidance; the mantra continues to be that we are killing our young women with tanning-bed use and sun exposure. Does no one care for the 50-year-old men who are dying from melanoma and do not use tanning beds? Does anyone even mention that there are more than twice as many men as women who die from melanoma?[6]
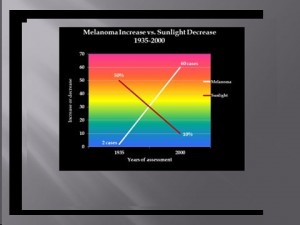
It has been ingrained into the consciousness of educated people throughout the world that the ultraviolet portion of sun radiation (UVR) is the cause of melanoma. The world population, however, as it “progresses,” spends increasingly less time exposed to direct sun. This is due to (1) an increase in indoor activities and decrease in outdoor activities, and (2) the increased use of sunscreens to prevent UVR exposure when outdoors. Nevertheless, the rate of melanoma is believed to be increasing at an alarming pace, as evinced by the aforementioned statement by the MIF, who also stated in 2007 that “melanoma is epidemic: rising faster than any other cancer and projected to affect one person in 50 by 2010, currently it affects 1 in 75. In 1935, only one in 1,500 was struck by the disease.”[7] That is correct; the American Cancer Society in 2014 reported that one in 50 now contracts the disease.[8] The MIF, then, if one assesses the statistics reported by medical organizations, was accurate regarding the increase in melanoma. However, they were wrong, perhaps “dead wrong” in stating that the sun is at fault.
Let’s take another look at the mathematics. According to the MIF, people had about 30 times the risk of contracting melanoma in 2010-2014 as in 1935, or stated in another way, a 3,000% risk increase. One might surmise that sun exposure must have increased spectacularly, during the time frame discussed, to have caused the exponential increase in melanoma, assuming that the statement by the MIF—that melanoma is caused by sun exposure—is correct. But is that statement correct?
Let’s ask six pertinent questions.
Question 1. Has sun exposure increased as melanoma has increased?
If melanoma has indeed increased exponentially since 1935, and if that increase is due to sun exposure, then sun exposure must also have shown a parallel or at least significant increase during that time. To determine the veracity of that idea, I analyzed data from the Office of Occupational Statistics and Employment Projections, Bureau of Labor Statistics (BLS), to determine if there was an increase or a decrease in human sun exposure during the years from 1910 to 2,000.[9] I closely considered changes since 1935, the year the MIF used as a baseline for measuring increases in melanoma incidence.
The data from the BLS showed that indoor occupations such as “professional, managerial, clerical, sales, and service workers (except private household service workers) grew from one-quarter to three-quarters of total employment between 1910 and 2000.” The BLS also stated that during the same period, the outdoor occupation of farming declined from 33% to 1.2% of total employment, a 96% reduction. The data also show that approximately 66% of the decline in the occupation of farmers and 50% of the decline in the occupation of farm laborers occurred after 1935. Further information, this time from the Environmental Protection Agency (EPA) determined that as of 1986, about 5 percent of adult men worked mostly outside, and that about 10 percent worked outside part of the time. The proportion of women who worked outside was thought to be even lower.[10] These data demonstrate a dramatic shift from outdoor, sun-exposed activity to indoor, non-sun-exposed activity during the mid-to-late 20th Century. This change, nonetheless, has been accompanied by a 30-times increase in melanoma risk since 1935, the MIF-baseline year. Accordingly, if sun exposure is really responsible for the pandemic of melanoma, it has achieved that dubious distinction during a time of profound decrease in sun exposure! To me, this is wholly counterintuitive. The data just presented really suggest that sun exposure is not responsible for the increase in melanoma, and we submit instead, that the profound decrease in sun exposure may be a factor in the purported exponential melanoma increase. That concept is illustrated graphically below.
Although it has been theorized that decreasing thickness of the ozone layer may be responsible for the increasing incidence of melanoma, research by Moan and Dahlback in Norway reported that yearly melanoma incidence increased 350% in men and 440% in women between 1957 and 1984—a period when there was absolutely no thinning of the ozone layer.[11]
The answer to question 1 is no; sun exposure has not increased as melanoma has increased. Exactly the opposite has occurred.
Question 2. Do outdoor workers have a higher incidence of melanoma than indoor workers?
If melanoma is increasing due to increased sun exposure, it is clear that outdoor workers, being exposed to far higher quantities of sun, would also have a far higher incidence of melanoma. Nevertheless, Dianne Godar and colleagues[12] presented evidence that outdoor workers, while receiving 3-9 times the sun exposure as indoor workers have had no increase in melanoma since before 1940, whereas melanoma incidence in indoor workers has increased steadily and exponentially.[13] [14]
Godar and colleagues also published irrefutable evidence of the protective influence of sun against melanoma in a landmark study in 2015,[15] entitled Dramatic Increases in Melanoma Correlate to Low Annual Sun exposure in Europe.
Published in the scientific journal Dermato-Endocrinology, the paper makes some very interesting comments, all based on excellent research:
- Melanoma has steadily increased in fair-skinned indoor working people around the world. Increasing melanoma incidence significantly correlates with decreasing personal annual UV doses [emphasis ours]. (UV or ultraviolet radiation is the spectrum of sun that stimulates the skin to produce vitamin D3.)
- People are more susceptible to melanoma when they have larger numbers of moles, light skin and hair, and poor tanning ability.
- There is a paradox between indoor and outdoor workers’ melanoma incidences and their annual UV (ultraviolet light) exposure. Outdoor workers receive 3-9 times the annual UV doses that indoor worker receive, but have only 50% of the risk for contracting melanoma.
- Although most scientists believe that intermittent UV exposures—resulting in sunburns—initiate melanoma, the creation and use of sunscreens DID NOT [emphasis ours] reduce the incidence of the disease. One of the reasons may be that sunscreens dramatically reduce vitamin D synthesis in the skin.
- Sunburns are probably not [emphasis mine] involved in the initiation or growth of melanoma, since a study on opossums showed that intense sun doses of UVB produced significantly fewer melanomas than sub-erythemal (non reddening) doses. Also, outdoor workers do get numerous sunburns but still have dramatically lower risk of contracting melanoma. [I do not advocate sunburning; although it may not cause melanoma, it will certainly do some damage to skin.]
- Many melanomas occur on areas of the body where the sun never shines.
The authors go on to theorize that a lower level of vitamin D, among those who receive inadequate sun, could be a major reason for the exponential increase of melanoma in European countries where the UV (sun) exposure is minimal. Another reason they suggest is infection with human papilloma virus (HPV).
Whatever the theories propose, regarding the cause of high melanoma incidence accompanying low sun or UV exposure, the equation remains the same: FOR THE VAST MAJORITY OF THE POPULATION, THE GREATER THE REGULAR EXPOSURE TO SUN, THE LESS THE RISK OF MELANOMA. Nevertheless, such information sells neither sunscreens nor melanoma surgeries, so don’t stand on one leg until the public believes the truth. However, you can learn the facts and become a soldier in the “sun army” by promoting the evidence.
Other research corroborates the idea that outdoor workers experience less melanoma than indoor workers.[16] Vagero, et al.[17] showed that melanoma was more common among indoor office workers and other indoor workers than among outdoor workers, and Kennedy, et al.[18] showed that a lifetime of sun exposure correlated to a reduced risk of melanoma. Garland, et al.[19] showed that those who worked indoors had a 50% greater risk of melanoma than those who worked both indoors and outdoors, and Kaskel, et al.[20] demonstrated that children who engage in outdoor activities are less likely to develop melanoma than those who do not. Many other papers in the scientific literature show that both incidence and death rate from melanoma are reduced with increasing exposure to sun.[21] [22] [23] [24] [25] [26] [27] [28] [29] [30] [31] [32]
None of these findings is surprising when one considers that whereas common, non-melanoma skin cancers are easily produced in experiments using ultraviolet radiation (UVR) from sunlamps, the same is not true for melanoma, which is difficult to produce with UVR.[33]
Finally, from 2016, research reported in the journal Anticancer Research demonstrated that UVR exposure was inversely associated with melanoma.[34] The researchers had set out to study whether the annual UVR level, estimated on a county level, was associated with incidence rates of oral, pharyngeal, and cervical cancers and melanoma. They found that all of these cancers were inversely associated with sun exposure. Interestingly, the authors, in their introduction to the research, said that UVR exposure is a well-demonstrated risk factor for melanoma. Then, at the end of their paper, they made this statement: “Our findings are in agreement with several other published studies reporting no positive correlation between UVR exposure and the incidence rates of oral, pharyngeal, and cervical cancer and melanoma.” Those two statements are contradictory, but their conclusion was correct: Those cancers are inversely correlated to UVR. Do you believe that the anti-sun organizations will admit their errors and embrace the sun? Don’t bet your bank account on it!
This data indicate again that sun exposure is not responsible for the increase in melanoma, and that the decrease in sun exposure may be a factor in the reported dramatic melanoma increase.
The answer to question 2 is no; outdoor workers do not have a higher incidence of melanoma than indoor workers.
Question 3. Do many melanomas occur on areas of the body that receive little sun exposure?
If sun exposure is the reason for the increase in melanoma, then it would be reasonable to expect that areas of the body that receive the most exposure, would also be the areas of greatest occurrence of the disease. This is not the case. The research by Garland and colleagues al.,[35] when assessing the incidence of melanoma occurring at various sites, found higher rates on the trunk (seldom exposed to sun) than on the head and arms (commonly exposed to sun). Others have shown that melanoma in women occur primarily on the upper legs, and in men more frequently on the back—areas of little sun exposure.[36] In blacks, melanoma is more common on the soles of the feet and on the lower legs.[37] Based on this data, it would be difficult to make the case that sun exposure is responsible for the increase in melanoma.
It should be mentioned that it is believed that intermittent bursts of intense sun (that causes sunburn) increases the risk of melanoma, whereas regular exposure reduces the risk[38] and that even on chronically sun-damaged skin, the mutations that lead to melanoma are rare.[39] Even the idea that sunburn causes melanoma is inconsistent with the fact that most melanomas do not occur at burn sites.[40] [41] The paper by Godar[42]put forth the hypothesis that lack of sun reduces the quantity of vitamin D in the skin, and then cited research showing that the potent hormone form of vitamin D, calcitriol, reduced the incidence, size and number of skin tumors and also reduced invasiveness and metastasis of melanoma in mice. Since regular sun exposure correlates to higher vitamin D production and higher levels in the blood, this evidence is plausible and would explain the reasons for reduced melanoma rates among those who are regularly exposed to sun.
Since many melanomas occur on areas of the body that receive little sun exposure, the indication is that sun exposure is not the cause of melanoma.
The answer to question 3 is yes, many melanomas occur on areas of the body that receive little sun exposure.
Question 4. Is there a co-morbidity of melanoma with common skin cancers, some of which are known to be associated to high sun exposure?
There is general agreement that sun exposure is one of the causal factors for squamous cell and basal cell carcinoma, also known as non-melanoma skin cancer (NMSC). However, these cancers do not demonstrate co-morbidity with melanoma.[43] [44] [45] Dr. Grant, after analyzing data from the Atlas of Cancer Mortality in the United States, noted that between 1950-1969 and 1970-1994, death rates from NMSC decreased by 31% for white males and by 47% for white females. However, during those same periods, melanoma death rates increased by 89% in white males and 42% for white females.[46]If one accepts the rate of NMSC as a measure of the cumulative exposure to sun, it is reasonable to conclude that sun exposure correlates to a reduced risk of melanoma, and that the lack of exposure increases the risk of melanoma.
This is another indication that sun exposure is not responsible for the increase in melanoma.
The answer to question 4 is no; there a no co-morbidity of melanoma with common skin cancers, some of which are known to be associated to high sun exposure.
Question 5. Has an increase in sunscreen use resulted in a decrease in melanoma?
Sunscreens block sun, and they are intended to decrease sun damage to the skin—damage that is said to increase the risk of melanoma. Sunscreen use has increased considerably in the past few decades. Therefore, if sun exposure is the cause of melanoma—as stated by the IMF—there should be a simultaneous decrease in melanoma as sunscreen use has increased. According to Kline & Company, a research group, sales of sunscreens in 1972 were $33 million; in 2008, sales were $650 million.[47] In addition, according to the Fredonia Market Research Group Company, the sales of sunscreens used in cosmetics in 2007 was $130 million.[48] Therefore, the total sales of sunscreens as of 2007 were $780 million. Considering that a dollar’s value is only about 20% of what it was in 1972, the adjusted 2008 sunscreen expenditures are approximately $156 million, or about 4.7 times the 1972 figure. In other words, sunscreen use has increased by about 4.7 times. Population also grew from 210 million in 1972 to 305 million in 2008–a 50% increase. Adjusting for population growth, it can be concluded that per capita sunscreen use has at least tripled in the time frame being considered.
As previously discussed, melanoma, according to the MIF, has increased steadily and exponentially since 1935. Therefore, the data on increasing sunscreen use does not indicate that sun exposure increases the risk of melanoma. Rather, it indicates that sunscreen use may, by reducing vitamin D production, contribute to the reported increase in melanoma. It has been shown that an SPF 15 sunscreen will decrease sun-stimulated vitamin D production by 99.5%, [49]and it has been suggested that by blocking only UVB light (which stimulates the production of vitamin D in skin) while leaving UVA unblocked, sunscreens ironically may lead to UVA damage of DNA, leading to melanoma.[50] [51] Increasing melanoma rates, coupled with increasing use of sunscreen, lends credence to that hypothesis. Regular sun exposure, therefore, does not increase risk of melanoma.
The answer to question 5 is no; increase in sunscreen use has not resulted in a decrease in melanoma.
Now let’s ask one more very important question:
Question 6. Is it possible that the reported pandemic of melanoma is not a pandemic at all, but that the “increase” in melanoma” is due to excessive diagnosis of benign lesions?
Writing in the British Medical Journal in 2008, Dr. Sam Shuster, a dermatologist, argued that the purported increase in melanoma is not really an increase, but an artifact due to non-melanoma lesions being misdiagnosed as melanoma.[52] In 2009, another study by dermatologists— Shuster and his colleagues—this time published by the British Journal of Dermatology, came to a similar conclusion and called the “increase” in melanoma a “midsummer night’s dream.”[53] They concluded, after tracking the reported increase in melanoma in the Eastern region of the UK between 1991 and 2004, that benign lesions were being classified in increasing numbers as stage-one melanoma. No other stages of the disease increased, and the increase in mortality due to melanoma was either miniscule or non-existent. This was true even though all grades of tumors were diagnosed at first presentation. They also noted that “the distribution of the lesions reported did not correspond to the sites of lesions caused by solar exposure,” a finding similar to that discussed in heading #3 above. These dermatologists concluded that “the large increase in reported incidence is likely to be due to diagnostic drift which classifies benign lesions as stage 1 melanoma.” They further stated that “These findings inevitably challenge the validity of epidemiology studies linking increasing melanoma incidence with UV radiation and suggest the need for a search for other ways in which the disease may be caused.”
Another celebrated dermatologist, Dr. A Bernard Ackerman, has written a monograph entitled Sun and the “Epidemic” of Melanoma: Myth on Myth.[54] In it he reviews extensive research and concludes that melanoma has nothing to do with sun exposure; and like the authors of the aforementioned BMJ article, he indicates that excessive diagnosis of benign lesions is responsible for the purported epidemic of melanoma.
Stunningly, the American Academy of Dermatology (AAD) published a report showing that most melanoma diagnoses may be incorrect.[55]Approximately 44 different authors contributed to that report. They made an accuracy-in-detection analysis based on the number of melanomas that needed to be excised during a period of ten years, compared to the actual number that were excised. Many clinics in different countries were involved in assessing the numbers.
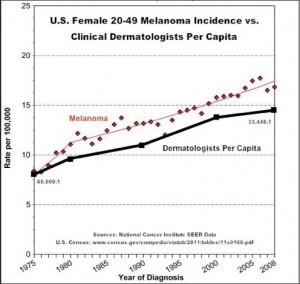
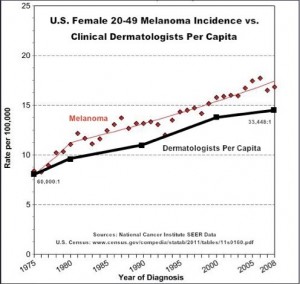
A total of 300,215 cases were found where excision took place. Of those cases, there were 17,172 melanomas that really required excision, and 283,043 that were excised and turned out to be benign lesions. Therefore, there were about 16.5 non-melanoma lesions removed for each lesion that was cancerous, and only about 6% were legitimate cancers. From this information, it is obvious that many melanoma surgeries are bogus and may inflate the incidence of melanoma. The aforementioned Drs. Shuster and Ackerman were correct. Dermatology is a huge business, and considering the spectacular per capita increase in the number of dermatologists, it is no wonder that they want to keep this little gravy train rolling down the track. See the graph below, which illustrates that the increase in the numbers of dermatologists paralleld the increase in the number of melanomas in young women.
It is obvious that the business of removing benign lesions is lucrative for the doctors. As the authors stated in their introduction to their research, “Early excision is the only strategy to reduce melanoma mortality, but unnecessary excision of benign lesions increases morbidity and healthcare costs.” It is hard to believe that the AAD published the report, but I am thankful it was done.
The answer to question 6 is yes. It is possible that the reported pandemic of melanoma is not a pandemic at all, but that the “increase” in melanoma” is due to excessive diagnosis of benign lesions.
The bottom line: From the research thus far presented, it could be concluded that either melanoma is increasing dramatically and is directly correlated to decreasing sun exposure, or that melanoma is not increasing at all, and the “epidemic” of melanoma does not exist. In either case, the statement by the MIF—that sun causes melanoma—has no validity. Stop blaming the sun!
You should have learned the following points from this part of the presentation:
- Sun exposure has decreased profoundly as melanoma has increased remarkably.
- Outdoor workers have a significantly lower incidence of melanoma than indoor workers.
- Many melanomas occur on areas of the body that receive little or no sun exposure.
- There a no co-morbidity of melanoma with common skin cancers, some of which are known to be associated to high sun exposure.
- An increase in sunscreen has been associated with an increase in melanoma incidence.
- It is possible that the “epidemic” of melanoma is not an epidemic at all, but that the “increase” in melanoma is due to excessive diagnosis of benign non-melanoma lesions.
- The idea that regular sun exposure leads to melanoma is counterintuitive.
- These facts should be presented to everyone who defames the sun as a carcinogen (cancer causer) for melanoma.
Stay tuned for more posts on this subject.
[1]Melanoma International Foundation, 2007 Facts about melanoma. Sources: National Cancer Institute 2007 SEER Database, American Cancer Society’s 2007 Facts and Figures, the Skin Cancer Foundation, the American Academy of Dermatology.
[2]Grant, W. In defense of the sun: An estimate of changes in mortality rates in the United States if mean serum 25-hydroxyvitamin D levels were raised to 45 ng/mL by solar ultraviolet-B irradiance. Dermato-endocrinology 2009;4:207-214.
[3]N.J. Levell, C.C. Beattie, S. Shuster and D.C. Greenberg. Melanoma epidemic: a midsummer night’s dream? British J Dermatol 2009;161:630–34
[4]Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015.CA Cancer J Clin. 2015 Jan-Feb;65(1):5-29.
[5] Melanoma Research Foundation. Melanoma Fact Sheet. Accessed 9-15-2014 at http://melanomainternational.org/melanoma-facts/#.VCHCG1_ANE0
[6] American Cancer Society. Cancer Facts & Figures 2015
[7] Melanoma Research Foundation. Melanoma Fact Sheet. Accessed 9-15-2014 at http://melanomainternational.org/melanoma-facts/#.VCHCG1_ANE0
[8] American Cancer Society. Melanoma Skin Cancer Overview 9/16/2014. http://www.cancer.org/cancer/skincancer-melanoma/overviewguide/melanoma-skin-cancer-overview-key-statistics
[9] Ian D. Wyatt and Daniel E. Hecker. Occupational changes in the 20th century. Monthly Labor Review, March 2006 pp 35-57: Office of Occupational Statistics and Employment Projections, Bureau of Labor Statistics
[10] U.S. Congress, Office of Technology Assessment, Catching Our Breath: Next Steps for Reducing Urban Ozone, OTA-O-412 (Washington, DC: U.S. Government Printing Office, July 1989).
[11] J. Moan and A. Dahlback. The relationship between skin cancers, solar radiation and ozone depletion. Br J Cancer 1992; 65: 916–21
[12] Godar D, Landry, R, Lucas, A. Increased UVA exposures and decreased cutaneous Vitamin D3 levels may be responsible for the increasing incidence of melanoma. Med Hypotheses 2009;72(4):434-43.
[13] Godar D. UV doses worldwide. Photochem Photobiol 2005;81:736–49.
[14] Thieden E, Philipsen PA, Sandby-Møller J, Wulf HC. UV radiation exposure related to age, sex, occupation, and sun behavior based on time-stamped personal dosimeter readings. Arch Dermatol 2004;140:197–203.
[15] Stephen J Merrill, Samira Ashrafi, Madhan Subramanian & Dianne E Godar. Exponentially increasing incidences of cutaneous malignant melanoma in Europe correlate with low personal annual UV doses and suggests 2 major risk Factors. Dermato-endocrinology 2015;7:1
[16] Lee J. Melanoma and exposure to sun. Epidemiol Rev 1982;4:110–36.
[17] Vågero D, Ringbäck G, Kiviranta H. Melanoma and other tumors of the skin among office, other indoor and outdoor workers in Sweden 1961–1979 Brit J Cancer 1986;53:507–12.
[18] Kennedy C, Bajdik CD, Willemze R, De Gruijl FR, Bouwes Bavinck JN; Leiden Skin Cancer Study. The influence of painful sunburns and lifetime sun exposure on the risk of actinic keratoses, seborrheic warts, melanocytic nevi, atypical nevi, and skin cancer. Invest Dermatol 2003;120:1087–93.
[19] Garland FC, White MR, Garland CF, Shaw E, Gorham ED. Occupational sun exposure and melanoma in the USA Navy. Arch Environ Health 1990; 45:261-67.
[20] Kaskel P, Sander S, Kron M, Kind P, Peter RU, Krähn G. Outdoor activities in childhood: a protective factor for cutaneous melanoma? Results of a case-control study in 271 matched pairs. Br J Dermatol 2001;145:602-09.
[21]Garsaud P, Boisseau-Garsaud AM, Ossondo M, Azaloux H, Escanmant P, Le Mab G. Epidemiology of cutaneous melanoma in the French West Indies (Martinique). Am J Epidemiol 1998;147:66-8.
[22]Le Marchand l, Saltzman S, Hankin JH, Wilkens LR, Franke SJM, Kolonel N. Sun exposure, diet and melanoma in Hawaii Caucasians. Am J Epidemiol 2006;164:232-45.
[23]Armstong K, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Biol 2001;63:8-18
[24]Crombie IK. Distribution of malignant melanoma on the body surface. Br J Cancer 1981;43:842-9.
[25]Crombie IK. Variation of melanoma incidence with latitude in North America and Europe. Br J Cancer 1979;40:774-81.
[26]Weinstock MA, Colditz,BA, Willett WC, Stampfer MJ. Bronstein, BR, Speizer FE. Nonfamilial cutaneous melanoma incidence in women associated with sun exposure before 20 years of age. Pediatrics 1989;84:199-204.
[27]Tucker MA, Goldstein AM. Melanoma etiology: where are we? Oncogene 2003;22:3042-52.
[28]Berwick M, Armstrong BK, Ben-Porat L, Fine J, Kricker A, Eberle C. Sun exposure and mortality from melanoma. J Nat Cancer Inst 2005;97:95-199.
[29]Veierød MB, Weiderpass E, Thörn M, Hansson J, Lund E, Armstrong B. A prospective study of pigmentation, sun exposure, and risk of cutaneous malignant melanoma in women. J Natl Cancer Inst 2003;95:1530-8.
[30]Oliveria S, Saraiya M, Geller A, Heneghan M, Jorgensen C. Sun exposure and risk of melanoma. Arch Dis Child 2006;91:131-8.
[31]Elwood JM, Gallagher RP, Hill GB, Pearson JCG. Cutaneous melanoma in relation to intermittent and constant sun exposure—the western Canada melanoma study. Int J Cancer 2006;35:427-33
[32] Grant WB. Role of solar UV irradiance and smoking in cancer as inferred from cancer incidence rates by occupation in Nordic countries. Dermatoendocrinol. 2012;4(2):203-11.
[33]Setlow RB, Woodhead AD, Grist E. Animal model for ultraviolet radiation induced melanoma: platyfish-swordtail hybrid. Proc Natl Acad Sci 1989;86:8922-9026
[34]Adams S, Lin J, Brown D, Shriver CD, Zhu K.Ultraviolet Radiation Exposure and the Incidence of Oral, Pharyngeal and Cervical Cancer and Melanoma: An Analysis of the SEER Data. Anticancer Res. 2016 Jan;36(1):233-7.
[35]Garland FC, White MR, Garland CF, Shaw E, Gorham ED. Occupational sun exposure and melanoma in the USA Navy. Arch Environ Health 1990; 45:261-67.
[36] Rivers, J. Is there more than one road to melanoma? Lancet 2004;363:728-30.
[37] Crombie, I. Racial differences in melanoma incidence. Br J Cancer 1979;40:185-93.
[38] Elwood JM, Gallagher RP, Hill GB, Pearson JCG. Cutaneous melanoma in relation to intermittent and constant sun exposure – The Western Canada melanoma study. Br J Cancer 1985;35:427–33.
[39]Maldonado JL, Fridlyand J, Patel H, Jain AN, Busam K, Kageshita T, Ono T, Albertson DG, Pinkel D, Bastian BC. Determinants of BRAF mutations in primary melanomas. J Natl Cancer Inst 2003 Dec 17;95(24):1878-90.
[40]Shuster, S. Is sun exposure a major cause of melanoma? No. BMJ2008;337:a764
[41]Garsaud P, Boisseau-Garsaud AM, Ossondo M, Azaloux H, Escanmant P, Le Mab G. Epidemiology of cutaneous melanoma in the French West Indies (Martinique). Am J Epidemiol 1998;147:66-8
[42]Godar DE, Landry RJ, Lucas AD. Increased UVA exposures and decreased cutaneous Vitamin D3 levels may be responsible for the increasing incidence of melanoma. Med hypothesis (2009), doi:10.1016/j.mehy.2008.09.056
[43]Grant, W. An ecologic study of cancer mortality rates in Spain with respect to indices of solar UVB irradiance and smoking. Int J Cancer 2007;120:1123-28.
[44] Tuohimaa P, Pukkala E, Scélo G, Olsen JH, Brewster DH, Hemminki K, Tracey E, Weiderpass E, Kliewer EV, Pompe-Kirn V, McBride ML, Martos C, Chia KS, Tonita JM, Jonasson JG, Boffetta P, Brennan P. Does solar exposure as indicated by the non-melanoma skin cancers protect from solid cancers? Vitamin D as a possible explanation. Eur J Cancer 2007;43:1701-12.
[45]Grant, W. Solar ultraviolet irradiance and cancer incidence and mortality. Chapter 2. Edited by JorgReichrath, Landes Bioscience 2007.
[46]Grant, W. Solar ultraviolet irradiance and cancer incidence and mortality. Chapter 2. Edited by JorgReichrath, Landes Bioscience 2007.
[47] Kline & Company’s Cosmetics & Toiletries USA Annual Service (1972 and 2008 editions).
[48] Fredonia market research group report, 2009.
[49] Matsuoka LY, Ide L, Wortsman J, MacLaughlin JA, Holick MF. Sunscreens suppress cutaneous vitamin D3 synthesis. Journal of Clinical Endocrinology & Metabolism 1987; 64:1165-68.
[50] Garland CF, Garland FC, Gorham ED. Could sunscreens increase melanoma risk? Am J Public Health 1992;82(4):614-5.
[51] Garland CF, Garland FC, Gorham ED. Rising trends in melanoma. An hypothesis concerning sunscreen effectiveness. Ann Epidemiol 1993 Jan;3(1):103-10.
[52] Shuster, S. Is sun exposure a major cause of melanoma? No. BMJ2008;337:a764
[53] N.J. Levell, C.C. Beattie, S. Shuster and D.C. Greenberg. Melanoma epidemic: a midsummer night’s dream? British J Dermatol 2009;161:630–34
[54] Ackerman, B. The Sun and the “Epidemic” of Melanoma: Myth on Myth. 2008.
[55]ArgenzianoG1, Cerroni L, Zalaudek I, Staibano S, Hofmann-Wellenhof R, et al. Accuracy in melanoma detection: a 10-year multicenter survey.J Am Acad Dermatol. 2012 Jul;67(1):54-9.
By Marc Sorenson, EdD Sunlight Institute
Those of us that understand the importance on regular sun exposure on human health were not surprised by the most recent research by Dr. Pelle Lindqvist and colleagues. It showed that women who had active sun-exposure habits lived longer than those who did not.[1] Over a 20-year period, the study demonstrated that compared to the highest sun-exposure group, life expectancy of sun avoiders was reduced significantly. Much of the reduction in death among the sun-exposed group was due to a lessened risk of cardiovascular disease and non-cancer, non-cardiovascular death. The risk of skin cancer was slightly increased among the sun exposed group, primarily because they lived longer and had more time to contract cancer.
Perhaps the most impressive statement to come out of the research was this: “Nonsmokers who avoided sun exposure had a life expectancy similar to smokers in the highest sun exposure group, indicating that avoidance of sun exposure is a risk factor for death of a similar magnitude as smoking.”
This newest research is just one of several important contributions by Lindqvist and his group. Other assessments of the 20-year study revealed that the subjects who avoided sun exposure were twice as likely to die of any cause compared to those who had the highest sun exposure, and the researchers made this statement: “In both models the summary sun exposure variables showed a ‘dose-dependent’ inverse relation between sun exposure and all-cause death.”[2]
The research also showed that women with “normal” sun exposure habits were not at significantly increased risk of either melanoma or melanoma-related death. The publication seemed to give vitamin D most of the credit for increased life spans among those who had high sun exposures, but also mentioned the possibility that nitric-oxide production by sun-exposed skin may have been a factor.
If avoiding the sun is as dangerous as smoking cigarettes, why do many dermatologists still try to frighten us to death about soaking up some rays? Will they never learn?
[1] Lindqvist PG, Epstein E, Nielsen K, Landin-Olsson M, Ingvar C, Olsson H. Avoidance of sun exposure as a risk factor for major causes of death: a competing risk analysis of the Melanoma in Southern Sweden cohort. J Intern Med. 2016 Mar 16. doi: 10.1111/joim.12496. [Epub ahead of print].
[2] Pelle G. Lindqvist, Elisabeth Epstein, Mona Landin-Olsson, Christian Ingvar, Kari Nielsen, Magnus Stenbeck & Håkan Olsson. Avoidance of sun exposure is a risk factor for all-cause mortality: results from the Melanoma in Southern Sweden cohort. J Intern Med. 2014 Jul;276(1):77-86.
By Marc Sorenson, EdD, Sunlight Institute…
Sepsis is a deadly disease, defined as infection of the tissues by bacteria. It can spread throughout the body and blood, where it is known as septicemia. Sepsis accounts for 500,000 emergency-room hospital visits per year in the USA, and the typical stay is nearly five hours.[1] It is one of the most deadly of medical conditions and often results in multiple organ failure.[2] It is, in fact, one of the top-ten causes of death. It is more common than heart attack, and claims more lives than any cancer.[3] Yet, much of the population has never heard of it.
Antibiotics have not been effective against severe sepsis and in some cases may exacerbate the disease.1 Sepsis is also the most common cause of death in critical-care patients in non-coronary intensive care units.[4]
Does regular time in the sun act to protect against this deadly disease? The research indicates that it does. In both the USA and UK, the disease is more common in winter than summer and higher in the Northeast than in the Southwest.
It is likely that vitamin D, produced by sun exposure, is the mechanism by which sepsis risk is decreased in summer.[5] According to Dr. William Grant, reports have shown that vitamin D upregulates human cathelicidin, LL-37, which has antimicrobial as well as anti-endotoxin activity.[6] However, we must never lose sight of the other benefits of sun exposure beyond vitamin D, which is only one of the sun’s beneficial photoproducts. Staying out of the sun—and using deadly chemical sunscreens to block life-giving sun exposure—are two of the biggest blunders ever made in the history of health disasters.
It is also interesting to note that in Australia, melanoma rates skyrocketed between 1980 and 2000.[7] 1980 was the year when a massive anti-sun campaign, called “Slip, Slop, Slap” began. Sepsis rates jumped simultaneously with melanoma and coincided with the widespread use of sunscreens. During this campaign, there was also an increase in viral respiratory infections, most cancers, and congestive heart failure.[8]
Remember that hospitals are not sterile environments. Try to stay away from them except in cases of dire need. Get some moderate, non-burning midday sun exposure instead—without using sunscreens.
[1] Wang, H. et al. National estimates of severe sepsis in United States emergency departments. Crit Care Med 2007;35:2461-2.
[2] Mookherjee, N. et al. Cathelicidins and functional analogues as antisepsis molecules. Expert Opinions on Therapeutic Targets 2007;11:993-1004.
[3] World Sepsis Day web page. September 13, 2015. http://world-sepsis-day.org/?MET=SHOWCONTAINER&vCONTAINERID=11. Accessed February 25, 2016.
[4] Florian B Mayr, Sachin Yende, and Derek C Angus. Epidemiology of severe sepsis. Virulence 2014, 5:1, 4-11.
[5] Karin Amrein, Paul Zajic, Christian Schnedl, Andreas Waltensdorfer, Sonja Fruhwald, Alexander Holl,
Tadeja Urbanic Purkart, Gerit Wünsch, Thomas Valentin, Andrea Grisold, Tatjana Stojakovic, Steven Amrein, Thomas R Pieber and Harald Dobnig. Vitamin D status and its association with season, hospital and sepsis mortality in critical illness. Critical Care 2014, 18:R47
[6] Grant WB Solar ultraviolet-B irradiance and vitamin D may reduce risk of septicemia. Dermatoendocrinol. 2009 Jan;1(1):37-42.
[7] Montague M, et al. Slip! Slop! Slap! and SunSmart, 1980-2000: Skin cancer control and 20 years of population-based campaigning. Health Educ Behav. 2001;28:290–305
[8] Grant WB Solar ultraviolet-B irradiance and vitamin D may reduce risk of septicemia. Dermatoendocrinol. 2009 Jan;1(1):37-42.
By Marc Sorenson, EdD, Sunlight Institute
Sunlight exposure is said to cause melanoma, which is false, as we have said many times in this blog. However, other cancers are seldom mentioned by those who would frighten us away from the sun, because the facts don’t fit their agenda. Most major cancers are profoundly reduced by sunlight. Let’s first take the example of prostate cancer (PC) risk, which has been known for at least 15 years to be associated with low sunlight exposure.
Researchers reporting their findings in the British medical journal, Lancet, compared sunlight-exposure history to the risk of contracting the disease, and they found that children who sunburned had about an 82% reduced risk of contracting PC as adults.[1] Of course, no one is recommending sunburn as a preventive measure against prostate cancer. In this case, sunburn served as a surrogate measure for a lot of sunlight exposure. Other measures of sunlight exposure similarly showed protective effects. Regular holidays in warm areas were associated with a 51% reduced risk; a high sunbathing score was associated to a 17% reduced risk, and very low sunlight exposure was associated to a tripling of risk. The researchers stated the following: “These findings are compatible with UVR having a protective role against prostate cancer.”
So why do the anti-sun groups such as the American Academy of Dermatology and the Skin Cancer Foundation mention only skin cancer and neglect to give life-saving information regarding other cancers such as PC? That is an easy answer. Both organizations make big dollars by keeping us in the dark. Follow the money to the sunscreen manufacturers, who have a cozy financial relationship with these supposedly “clean” cancer organizations.
So men, safely sunbathe and get outdoors as much as possible. Your prostate will love you for it.
[1] Luscombe CJ, Fryer AA, French ME, Liu S, Saxby MF, Jones PW, Strange RC. Exposure to ultraviolet radiation: association with susceptibility and age at presentation with prostate cancer. Lancet. 2001 Aug 25;358(9282):641-2.
By Marc Sorenson, EdD, Sunlight Institute…..
Before proceeding with the discussion on sunlight addiction, it is important to review the truth about sunlight and melanoma, to understand why sunlight addiction may be a good thing.
A recent report on ultraviolet light and addiction[1] is obviously meant to be a hit piece regarding sunlight exposure and tanning, as seen in the opening statement: “Despite widespread awareness that UV exposure is a major risk factor for all common cutaneous malignancies, skin cancer incidence relentlessly increases by ~3% per year.”
The “all common cutaneous malignancies” portion of this statement, of course, is patently false. Whereas the relatively benign common skin cancers are increased by exposure to sunlight, melanoma is increased by avoiding the sun. If the dramatic increase in melanoma over the past century were due to sunlight exposure, then sunlight exposure must also have increased dramatically during that time. To determine whether that has happened, we analyzed data from the Office of Occupational Statistics and Employment Projections, Bureau of Labor Statistics, (BLS) to determine if there was an increase or decrease in human sunlight exposure during the years from 1910 to 2,000.[2] The statistics showed that indoor occupations such as “professional, managerial, clerical, sales, and service workers grew from one-quarter to three-quarters of total employment between 1910 and 2000.” BLS also stated that during the same period, the outdoor occupation of farming declined from 33% to 1.2% of total employment, a 96% reduction. The data also showed an approximately 66% decline in the occupation of farmers and 50% of the decline in the occupation of farm laborers.
The Environmental Protection Agency also determined that as of 1986, about 5 percent of adult men worked mostly outside, and that about 10 percent worked outside part of the time. The proportion of women who worked outside was thought to be even lower.[3] These data demonstrate a dramatic shift from outdoor, sun-exposed activity to indoor, non-sun-exposed activity during the mid-to-late 20th Century.
Despite these facts, the Melanoma International Foundation (MIF) has stated that melanoma has increased by 30 times (3,000%) just since 1935! Here is the statement by the MIF: “Melanoma is epidemic: rising faster than any other cancer and projected to affect one person in 50 by 2010, currently it affects 1 in 75. In 1935, only one in 1,500 was struck by the disease.”[4] Indeed, the American Cancer Society in 2014 reported that one in 50 now contracts the disease.[5] That exponential increase in melanoma has been accompanied by a profound decrease in sunlight exposure, yet sunlight or other UV exposure is blamed for the melanoma increase—a totally counterintuitive argument! I submit that not only is sunlight not responsible for the exponential increase in melanoma, but that the decrease in sun exposure may be a major cause of that increase.
Here are other facts that belie the idea that melanoma is caused by sunlight exposure:
- Outdoor workers, while receiving 3-9 times the UVR exposure as indoor workers,[6] [7] have had no increase in melanoma since before 1940, whereas melanoma incidence in indoor workers has increased steadily and exponentially.
- Most melanomas occur on areas of the body that are seldom or never exposed to the sunlight.[8] [9] [10]
- The use of sunscreen, which has increased steadily, has not resulted in a decrease in melanoma.[11] In fact, melanoma has increased as sunscreen use has become more widespread. Since sunscreens block sunlight, it is evident that at best they are a waste of money and at worst may be contributing to the increase in melanoma.
Now, let’s discuss the research on the aforementioned addiction to sunlight. The researchers conducted various experiments on mice that showed behavior choices, such as desiring lighter rather than darker environments, were increased by regular exposure. These behavior choices were mediated by β-endorphins, peptide hormones which are similar to opiates. So is this all bad? This marvelous product, β-endorphin, is one of the feel-good hormones that decreases pain and increases a sense of well-being. The case the researchers make regarding addiction to sunlight is compelling, and why not? Sunlight exposure causes vitamin D production in the skin, which is essential to human health; it also stimulates the production of nitric oxide, which relaxes our vessels and lowers our blood pressure; it stimulates the production of serotonin in the brain, which is another feel-good hormone necessary for a happy mood and wellbeing. And considering the myriad additional effects of sunlight on health, including the prevention of cancer, the prevention and reversal of bone diseases and the reduction of heart disease, could it not be part of God’s (or Nature’s) master plan to develop a positive addiction to sunlight so than our health could be enhanced? I am a sunlight addict, and expose myself to it regularly for two reasons: (1) It marvelously improves my mood and (2) it protects me from disease and weakness. I am a light-skinned, blue-eyed Caucasian who has spent much of my seven decades on this earth seeking the sun. Yet, there have been no melanomas or even common skin cancer.
Nevertheless, the researchers summarize their paper on sun addiction with the following: “While primordial UV addiction, mediated by the hedonic [pertaining to pleasure] action of β-endorphin and anhedonic effects of withdrawal, may theoretically have enhanced evolutionary vitamin D biosynthesis, it now may contribute to the relentless rise in skin cancer incidence in man.”
That summary statement is claptrap, as can be seen by the research on melanoma and sunlight presented above. If sunlight is addictive and helps me to avoid melanoma, heart disease, bone loss and other maladies, I can only say, “hooray for the addiction!”
[1] Gillian L. Fell, Kathleen C. Robinson, Jianren Mao, Clifford J. Woolf, and David E.
Fisher. Skin β-endorphin mediates addiction to ultraviolet light. Cell. 2014 June 19; 157(7): 1527–1534.
[2] Ian D. Wyatt and Daniel E. Hecker. Occupational changes in the 20th century. Monthly Labor Review, March 2006 pp 35-57: Office of Occupational Statistics and Employment Projections, Bureau of Labor Statistics
[3] U.S. Congress, Office of Technology Assessment, Catching Our Breath: Next Steps for Reducing Urban Ozone, OTA-O-412 (Washington, DC: U.S. Government Printing Office, July 1989).
[4] Melanoma International Foundation, 2007 Facts about melanoma. Sources: National Cancer Institute 2007 SEER Database, American Cancer Society’s 2007 Facts and Figures, The Skin Cancer Foundation, The American Academy of Dermatology.
[5] American Cancer Society. Melanoma Skin Cancer Overview 9/16/2014. Accessed on 9/23/2014 at http://www.cancer.org/cancer/skincancer-melanoma/overviewguide/melanoma-skin-cancer-overview-key-statistics
[6] Godar D. UV doses worldwide. Photochem Photobiol 2005;81:736–49.
[7] Thieden E, Philipsen PA, Sandby-Møller J, Wulf HC. UV radiation exposure related to age, sex, occupation, and sun behavior based on time-stamped personal dosimeter readings. Arch Dermatol 2004;140:197–203.
[8] Garland FC, White MR, Garland CF, Shaw E, Gorham ED. Occupational sunlight exposure and melanoma in the USA Navy. Arch Environ Health 1990; 45:261-67.
[9] Rivers, J. Is there more than one road to melanoma? Lancet 2004;363:728-30.
[10] Crombie, I. Racial differences in melanoma incidence. Br J Cancer 1979;40:185-93.
[11] Phillippe Autier. Do high factor Sunscreens offer protection from melanoma? West J Med. 2000 Jul; 173(1): 58.