Sunscreen chemicals. By Marc Sorenson, EdD.
 Sunscreen chemicals are toxic. I have written about them previously and did an analysis of sunscreen chemicals dangers in my book, Embrace the Sun. And now, Science Digest alerts the public of new research. It indicates that even low concentrations of sunscreen chemicals can stimulate breast tissue growth. Thus, these chemicals could lead to breast cancer. Nevertheless, these chemicals affected only breast cells that had estrogen receptors. The sunscreen chemical tested was oxybenzone, which mimics estrogen in some aspects. Oxybenzone and other similar chemicals are known as xenoestrogens. They are also suspected of many injurious effects beyond possibly causing breast cancer.
Sunscreen chemicals are toxic. I have written about them previously and did an analysis of sunscreen chemicals dangers in my book, Embrace the Sun. And now, Science Digest alerts the public of new research. It indicates that even low concentrations of sunscreen chemicals can stimulate breast tissue growth. Thus, these chemicals could lead to breast cancer. Nevertheless, these chemicals affected only breast cells that had estrogen receptors. The sunscreen chemical tested was oxybenzone, which mimics estrogen in some aspects. Oxybenzone and other similar chemicals are known as xenoestrogens. They are also suspected of many injurious effects beyond possibly causing breast cancer.
Other deleterious effects of sunscreen chemicals 1
First of all, several years ago, the CDC released a study showing that 96.8% of Americans at age six are contaminated with oxybenzone. The study also showed that women were 3.5 times as likely to have high concentrations as men.[1] The authors suggest that women’s greater use of personal-care products, most of which contain sunscreens, is the reason for their higher degree of contamination. Oxybenzone is used in 588 sunscreens and in 567 other personal-care products.[2] Another investigation showed that up to 8.7% of oxybnezone is absorbed[3] and accumulates in the body.[4] It is still found in the urine 5 days after application.
Other deleterious effects of sunscreen chemicals 2
Other research papers confirm that sunscreen chemicals are highly absorbed and then detected in urine and breast milk, where they may cause systemic effects, including disruption of the endocrine system.[5], [6]
In addition, pregnant mothers exposed to oxybenzone gave birth to babies with low birth weights, [7] which “programs” the developing child for greater risks of heart disease, hypertension, type-two diabetes and other diseases in adulthood.[8] Furthermore, sun causes the chemical to become a potent allergen[9], [10] and to form free radicals.[11], [12], [13], [14] Free radicals are unstable atoms which lack an electron in their outer shells. One study concluded, “The surprising result is UV filters applied to the skin surface not only lose their screening capability after a period of incubation, but also may lead to enhanced ROS [free radicals] generation in nucleated epidermis through photogeneration.“[15] In fact, after one hour, more free radicals were created by sunlight contacting sunscreen, than sunlight on skin. To me, this is another indication that sunscreens cause more damage than no sunscreens!
Other deleterious effects of sunscreen chemicals 3
In addition to adverse effects on human health, sunscreen chemicals have potential deleterious effects on the environment. A study from the Archives of Environmental Contamination and Toxicology, regarding the detrimental effects of Oxybenzone, stated that Oxybenzone is a photo-toxicant, meaning its adverse effects are exacerbated in the light.[16] Does this toxic chemical sound like something you’d like to apply to your skin or your children’s skin while out in the sun?
The researchers also stated: “Oxybenzone is an emerging contaminant of concern in the marine environment.” They found that a small dollop of sunscreen in six Olympic-sized pools caused a disruption of coral growth. Such disruption leads to a whitening and killing of the marine activity of coral reefs. This is accomplished by ossification of a free-swimming larva called a planula, which kills the growth of coral reefs. And this information has proven to be prophetic. Many beach areas have now prohibited the use of sunscreen chemicals due to concerns about coral-reef destruction.
The final nail in the coffin for sunscreen chemicals: they may lead to sunburns.
I have often stated that sunscreens may be worthless at best and dangerous at worst. Another scientific study accidentally corroborated my conclusion.[17] The researchers wanted to discover which sun-protection behavior was most effective in preventing sunburn. Hence, they designed a cross-sectional investigation using a nationally representative sample of about 32,000 US adults. They interviewed each participant in person. This is especially relevant when attempting to achieve the most accurate results possible. We can conclude, therefore, that their findings regarding sunscreen use and other “sun-protective” behaviors probably have validity. Seeking shade, wearing a hat or visor, and wearing long sleeves and or pants were other sun-protective behaviors included.
The results:
Fifty-four percent of the subjects were women, and 15,992 of all individuals were considered sun-sensitive (fair skinned). Those who used only sunscreen had the highest sunburn likelihood (62.4%). Also, the group with lowest likelihood of sunburn did not use sunscreen, but engaged in the other protective behaviors (24.3% sunburned). In addition, among 12,566 non–sun-sensitive individuals, those engaged in all 4 protective behaviors had the lowest sunburn (6.6%). The highest likelihood of sunburn was among those who used only sunscreen (26.2%). “The most surprising and counterintuitive finding was that regular sunscreen use, in the absence of other protective behaviors, was associated with the highest likelihood of sunburn.” according to Kasey Morris, who led the study.
Finally, a meta-analysis of the best research, involving 313,000 subjects found that neither melanoma nor non-melanoma skin cancer was associated with sunscreen use. And, another study indicated that in the last three decades, melanoma incidence has increased by 400% and sunscreen use has also increased by 400%. Isn’t it time that we stopped using this toxic, chemical soup?

Think carefully about this information when you next see a sunscreen ad. Enjoy the sun safely (without burning).
Happy sunning
[1] Calafat, A. Concentrations of the Sunscreen Agent, Benzophenone-3, in Residents of the United States: National Health and Nutrition Examination Survey 2003–2004. (Available at http://dx.doi.org/).
[2] Environmental Working Group: Americans Carry Body Burden of Toxic Sunscreen Chemical. 25, 2008. (Available at http://www.ewg.org/node/26212).
[3] Hayden CG, Roberts MS, Benson HA. Systemic absorption of sunscreen after topical application. Lancet 1997:350:863-64.
[4] Gonzalez H, Farbrot A, Larkö A-M. Wennberg A. Percutaneous absorption of the sunscreen benzophenone-3 after repeated whole-body applications, with and without ultraviolet irradiation. British J Dermatol 2016;154:137-140.
[5] Krause M, Klit A, Blomberg Jensen M, Søeborg T, Frederiksen H, Schlumpf M, Lichtensteiger W, Skakkebaek NE, Drzewiecki KT. Sunscreens: Are they beneficial for health? An overview of endocrine disrupting properties of UV-filters. Int. J. Androl. 35, 424436 (2012).
[6] Yang Deng, Asiri Ediriwickrema, Fan Yang, Julia Lewis, Michael Girardi and W. Mark Saltzman. A sunblock based on bioadhesive nanoparticles. Nature materials: published online: 28 September 2015.
[7] Mary S. Wolff, Stephanie M. Engel, Gertrud S. Berkowitz, Xiaoyun Ye, Manori J. Silva, Chenbo Zhu, James Wetmur, and Antonia M. Calafat. Prenatal Phenol and Phthalate Exposures and Birth Outcomes. National Institutes of Health USA Department of Health and Human Services.(available at http://dx.doi.org/)
[8] Lau C, Rogers JM. 2004. Embryonic and fetal programming of physiological disorders in adulthood. Birth Defects Res C Embryo Today 2004;72:300-12.
[9] Bryden AM, Moseley H, Ibbotson SH, Chowdhury MM, Beck MH, Bourke J, English J, Farr P, Foulds IS, et al. Photopatch testing of 1155 patients: results of the U.K. multicentre photopatch group. B J Dermatol 2006;155:737-47.
[10] Rodriguez E, Valbuena MC, Rey M, Porras de Quintana L. 2006. Causal agents of photoallergic contact dermatitis diagnosed in the national institute of dermatology of Colombia. Photodermatol Photoimmunol Photomed 2006;22:189-92.
[11] Hanson KM, Gratton E, Bardeen CJ. Sunscreen enhancement of UV-induced reactive oxygen species in the skin. Free Radic Biol Med. 2006 Oct 15;41(8):1205-12.
[12] Bastien N, Millau JF, Rouabhia M, Davies RJ, Drouin R. The sunscreen agent 2-phenylbenzimidazole-5-sulfonic acid photosensitizes the formation of oxidized guanines in cellulo after UV-A or UV-B exposure. J Invest Dermatol. 2010 Oct;130(10):2463-7
[13] Gulston M, Knowland J. Illumination of human keratinocytes in the presence of the sunscreen ingredient Padimate-O and through an SPF-15 sunscreen reduces direct photodamage to DNA but increases strand breaks. Mutat Res. 1999 Jul 21;444(1):49-60.
[14] Environmental Working Group: Americans Carry Body Burden of Toxic Sunscreen Chemical. 25, 2008. (Available at http://www.ewg.org/node/26212).
[15] Hanson KM, Gratton E, Bardeen CJ. Sunscreen enhancement of UV-induced reactive oxygen species in the skin. Free Radic Biol Med. 2006 Oct 15;41(8):1205-12.
[16] C. A. Downs , Esti Kramarsky-Winter, Roee Segal, John Fauth, Sean Knutson, Omri Bronstein, Frederic R. Ciner, Rina Jeger, Yona Lichtenfeld et al. Toxicopathological Effects of the Sunscreen UV Filter, Oxybenzone (Benzophenone-3), on Coral Planulae and Cultured Primary Cells and Its Environmental Contamination in Hawaii and the US Virgin Islands. Archives of Environmental Contamination and Toxicology Oct 20 2015.
[17] Kasey L. Morris, PhD; Frank M. Perna, EdD, PhD. Decision Tree Model vs Traditional Measures to Identify Patterns of Sun-Protective Behaviors and Sun Sensitivity Associated With Sunburn. JAMA Dermatol. Published online June 27, 2018.
Melanoma risk is prevented by sun exposure. Case closed! -By Marc Sorenson, EdD
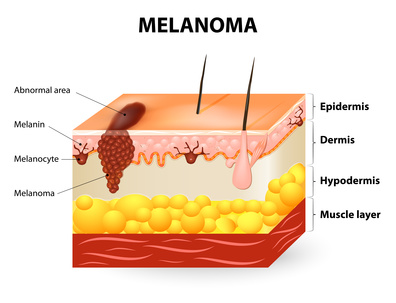
Melanoma risk between persons with high and low vitamin D levels
Melanoma risk is probably the most misunderstood topic in medicine. I recently wrote about the inverse association between vitamin D and melanoma. But I finally decided that my case had insufficient passion and surety. Consequently, I decided to write this addition and provide some new and restated information.
Melanoma risk is directly associated with low levels of vitamin D. That is the conclusion of recent study published in the European Journal of Cancer.[1] The investigators measured the blood vitamin D levels of 137 subjects who had been diagnosed with melanoma. They collected the blood samples at the time of diagnosis of the disease. Another group of 99 healthy subjects served as the control group. The investigators collected the samples of the control group between October and April. The scientists then compared the blood collections of the melanoma group with those of the control group. They then determined whether vitamin D levels had an association with melanoma risk.
The study produced convincing results regarding vitamin D and melanoma risk.
The results were as follows:
- The controls (no melanoma) had vitamin D levels 50% higher than the melanoma group (27.8 ng/ml vs. 18 ng/ml).
- 66.2% of the melanoma group had vitamin D “deficiency,” compared to only 15.2% of the health controls. The scientists defined vitamin D deficiency as being equal to or less than 20 ng/ml. So, the melanoma group had more than four-times the risk of deficiency.
- The scientists defined vitamin D “sufficiency” as being equal to or greater than 30 ng/ml. They found that only 7.4% of melanoma patients were sufficient, compared to 37.4% of healthy controls. Hence, the melanoma group had about one-fifth the likelihood of having sufficient D levels.
More scientific analysis on vitamin D measurements vs. melanoma risk
The scientists then adjusted the data for possible confounding factors such as age, sex and body mass. Then, they performed an analysis that showed the following:
- First of all, a significant inverse association was demonstrated with vitamin D sufficiency versus deficiency. Those who had sufficient levels had only 4% of the melanoma risk when compared to those who were deficient! Hence, this would indicate that those with the lowest vitamin D levels (after adjusting for confounding factors) had 25-times the melanoma risk!
- And, vitamin D insufficiency vs. deficiency was significantly inversely associated with melanoma. Those who were insufficient had a definite advantage over those who were deficient. They had only 13% of the melanoma risk.
Now, let’s get to the most important point about melanoma risk:
In addition, this research proves conclusively that sun deprivation is a major cause of melanoma. Therefore, vitamin D levels are surrogate measurements for sun exposure in nearly every case. And why do I say than this research conclusively proves that sun exposure reduces melanoma risk? Because about 90% of serum vitamin D is produced by sun exposure to the skin.[2] So, the aforementioned research is really research on sun exposure. It indicates that regular sun exposure leads to a profoundly higher vitamin D levels and therefore a profoundly reduced melanoma risk. So, let’s restate the facts about vitamin D, sunlight and melanoma.
- First of all, sunlight exposure to skin produces 90% of the vitamin D levels in the public.
- Secondly, the higher the vitamin D levels, the lower is the risk of melanoma.
- Therefore, high sun exposure reduces melanoma risk.
- Case closed!
Nevertheless, there is more corroborating evidence for the case.
In addition, here are a few more facts indicative of sun exposure’s protective effect against melanoma risk:
- Another supporting fact: 75% of melanomas occur on body areas that are seldom if never exposed to sunlight.[3]
- In addition, sun exposure decreased by 90% since 1935, while melanoma increased by 3,000%.[4]
- Also, in the past four decades, melanoma has increased 400% while sunscreen use also increased 400%.[5]
- Furthermore, sunburn is said to increase melanoma risk. And recent research shows that sunscreen use increases the risk of sunburn from 300-600%.[6]
Could sunlight reduce melanoma through photoproducts beyond vitamin D?
In conclusion: In my new book, Embrace the Sun (coauthored by Dr. William Grant), we note that sun exposure provides more than vitamin D. It also provides other photoproducts such as nitric oxide, serotonin, endorphin, and brain-derived neurotropic factor (BDNF). All of these photoproducts are vital to human health. Could these photoproducts have a positive and protective effect against melanoma risk beyond vitamin D? And, who is to say that the vitamin D produced by sunlight is not superior to that given in pill form?
Finally, this research gives us one more reason to embrace the sun safely without burning. And who would have thought that safe sunlight could be one of the best prophylactics against melanoma risk?
Happy sunning! Do not burn.
The book is available at Amazon: https://www.amazon.com/Embrace-Sun-Marc-B-Sorenson/dp/069207600X
[1] Cattaruzza MS, Pisani D, Fidanza L, Gandini S, Marmo G, Narcisi A, Bartolazzi A, Carlesimo M. 25-Hydroxyvitamin D serum levels and melanoma risk: a case-control study and evidence synthesis of clinical epidemiological studies. Eur J Cancer Prev. 2018 Feb 12. [Epub ahead of print]
[2] Reichrath J. The challenge resulting from positive and negative effects of sun: how much solar UV exposure is appropriate to balance between risks of vitamin D deficiency and skin cancer? Prog Biophys Mol Biol 2006;92(1):9-16
[3] Crombie IK. Distribution of malignant melanoma on the body surface.Br J Cancer. 1981 Jun;43(6):842-9.
[4] Melanoma International Foundation, 2007 Facts about melanoma. Sources: National Cancer Institute 2007 SEER Database, American Cancer Society’s 2007 Facts and Figures, The Skin Cancer Foundation, The American Academy of Dermatology.
[5] Joseph C DiNardo and Craig A Downs. Should We Use Products Containing Chemical UV Absorbing Sunscreen Actives on Children? Clin Dermatol Res J 2019, 4:1.
[6] Kasey L. Morris, PhD; Frank M. Perna, EdD, PhD. Decision Tree Model vs Traditional Measures to Identify Patterns of Sun-Protective Behaviors and Sun Sensitivity Associated With Sunburn. JAMA Dermatol. Published online June 27, 2018.
 An innate need for sunlight exists within the human body and soul.
An innate need for sunlight exists within the human body and soul.
First of all, consider the opening line of a recent article in the New York Times: “Let there be light. Please.” And, the article states that people in New York City (NYC) love to seek apartments with sunlight. It is also especially relevant that such apartments demand premium prices. But sun seekers have a problem because of the continuous building of new high rises. Consequently, they must look at the city’s future building plans before they fulfill their innate need for sunlight. This is because new buildings may be built that block whatever sunlight is available.
Problems encountered in fulfilling the innate need for sunlight in NYC.
Therefore, it is a difficult situation to satisfy the innate need for sunlight in NYC. And no wonder people in the southern states have lower cancer rates, despite their atrocious eating habits.[1] Why? Because they have one of the best cancer fighters: sunlight.
An example of the rather impressive anti-cancer power of sunlight: Iranian research demonstrated the innate need for sunlight. Women who avoided sun exposure had 10 times the breast cancer risk.[2] That is, of course, when they were compared to women who were able to obtain regular sunlight. This is because the innate need for sunlight was being ignored among women forced to avoid sun.
What other diseases are manifest when we ignore our innate need for sunlight?
Lack of sun exposure increases the risk of 16 other cancers, heart disease, vitamin D deficiency, multiple sclerosis, hip fractures, depression and myriad others. (See my book, Embrace the Sun, for a full discussion.) The innate need for sunlight manifests itself in higher rates of these “killer” diseases worldwide.
According to the NYT article, “there are those who view light as an elemental need, one that trumps everything else, including location, closets, level floors, an elevator, a doorman and proximity to Trader Joe’s.” Obviously, the people recognize, at a visceral level, their innate need for sunlight.
Do the Chinese have an innate need for sunlight?
Another article also emphasized the innate need for sunlight.[3] And, this one came from halfway around the world, in Shanghai. It seems like the Chinese should know about sun healing, since their experience in healing goes back thousands of years. Hence, they would not need to read this article to appreciate the innate need for sunlight. A real-estate developer there had to pay a family the equivalent of $15,650.00 for robbing them of their sun. One of the developer’s skyscrapers exceeded the legal height, and partially blocked the sun to their apartment. Consequently, this prevented the family from obtaining their government-mandated sun allotment. The allotment was two hours per day, and the skyscraper allowed only 1-2 hours of sun.
A judge who understands the innate need for sunlight
The judge in the case said, “We can’t live without sunshine” and told the developers they had to respect the rights of the people to enjoy the sun. Due to this judge’s understanding of the innate need for sunlight, justice was done.
Why is the innate need for sunlight not recognized in the U.S? Good question!
The Chinese experience is in stark contrast with the US. First of all, in the 1990s, a president of the American Academy of Dermatology (AAD) made this statement. “In some vision as I grow older I see us moving to more shelters and perhaps underground living because of these hazards” (meaning sun exposure).[4] Also, she stated that melanoma would cause more cancer deaths than any other cancer by about 2010. Since it is now 2018, and we are not yet living underground, she was ridiculously wrong. In addition, melanoma is nowhere near the top of the cancer-deaths charts. It kills far less people than most major cancers like lung, breast, colon and prostate. However, it will probably increase in incidence as more people are convinced by the ADD to avoid their innate need for sunlight.
When it comes to the innate need for sunlight, the Chinese have more smarts!
It appears that the Chinese are a whole lot smarter than the AAD regarding the innate need for sunlight! Therefore, the AAD’s insistence on sun avoidance is likely to destroy public health. And, soaking up some safe, unobstructed, regular sunlight will enhance health. The AAD’s insistence on sun avoidance is much more likely to destroy the health of the American public than soaking up some unobstructed sunshine. So please, PLEASE enjoy some safe, non-burning sun, winter and summer, while you improve your health! And remember that sunscreens inhibit 95% of vitamin D production. Therefore, when you have had enough sun exposure, cover up with clothing or seek shade. Those who use sunscreens have far more sunburns than those who do not use it.[5] Think about it, and read my book, Embrace the Sun so that you can be comfortable while attending to your innate need for sunlight. https://www.amazon.com/Embrace-Sun-Marc-B-Sorenson/dp/069207600X 
[1] Sorenson, M. Vitamin D3 and Solar Power. Chapter 8. 2008.
[2] Bidgoli SA, Azarshab H. Role of vitamin D deficiency and lack of sun exposure in the incidence of premenopausal breast cancer: a case control study in Sabzevar, Iran. Asian Pac J Cancer Prev. 2014;15(8):3391-6.
[3] http://www.shanghaidaily.com/national/Sun-suit-Family-wins-payout/shdaily.shtml
[4] Dr. Wilma Bergfeld, then-president of the American Academy of Dermatology at Derm Update, the AAD’s 1996 annual media day, Nov. 13, 1996.
[5] Silva ESD, Tavares R, Paulitsch FDS, Zhang L. Use of sunscreen and risk of melanoma and non-melanoma skin cancer: a systematic review and meta-analysis. Eur J Dermatol. 2018 Apr 1;28(2):186-201.
Lets talk sunscreens!
 Protection or Cause?
Protection or Cause?
Sales of sunscreens, first of all, are a multi-billion dollar industry. And, it seems like nearly everyone believes that they are a great protection against skin cancer. Especially relevant is the fact that as sales climb higher each year, melanoma risk increases in lock step. Furthermore, sunscreen sales in 1972 were about $18 million per year.[1] And, the total USA market in 2005 had climbed to $640 million a year.[2] Due to inflation, that is equivalent to $320 million in 1972 dollars, an almost 18-fold increase.
What about sunscreens in cosmetics?
In addition, those figures pale by comparison with figures from 2013. The global sun care market generated $5.6 billion US dollars from its sun-protection products segment. Why? Because the sun care market includes sunscreens, many of which are ingredients in women’s cosmetics.[3] Sales increased despite the fact that as early as 2003, it was known that sunscreens may have been partially responsible for increasing the deadliest of skin cancers, melanoma.[4]
Another important study demonstrates that sunscreens do not help prevent melanoma.[5] The researchers’ goal was to determine the efficacy of sunscreens in preventing melanoma. Hence, they compared melanoma rates with sales in 24 countries in Europe, during the period of 1997-1999 to 2008 and 2012. They found that higher income people had significantly higher melanoma incidence. And, increased use of sunscreens had not prevented higher income populations from being at higher risk of melanoma. Consequently, we see this equation: Higher use=higher melanoma risk! One of the reasons for this little-known relationship is most noteworthy. Up to 99% of vitamin D production is stopped by sunscreen.[6] Hence, many of the health benefits of sun are voided.
The latest research
In conclusion, the latest research must have deflated the egos of the sunscreen manufacturers: A meta-analysis of 20 studies showed what we would expect. Both melanoma and non-melanoma skin cancers were not protected by sunscreens.[7] It is most noteworthy that sunscreens were associated with a slight increase in risk. We could probably say from the information I’ve presented that sunscreens are worthless at best, and dangerous at worst. So, who benefits? Those who benefit from sales are pleased, while the people suffer. Therefore, it seems like the manufacturers, and the industries they support, are probably quite pleased with the worthless product.
Be careful about sunscreen ads!
So, when you next view the propaganda, be careful before you drink the Kool-Aid. And, be sure to read my new book, Embrace the Sun. It contains a full section on the chicanery that is prevalent in the sunscreen conspiracy. You will be stunned when you learn the truth. 
Embrace the Sun is available at Amazon: https://www.amazon.com/Embrace-Sun-Marc-B-Sorenson/dp/069207600X/ref=sr_1_1?ie=UTF8&qid=1532229265&sr=8-1&keywords=Embrace+the+sun
[1] Moss, R. Another Dissident Dermatologist.Cancerdecisions.com Newsletter. 2005.
[2] Bonner, C. Contact Kline Co. http://www.klinegroup.com/
[3] http://www.statista.com/topics/1990/sun-care-industry/
[4] Haywood, R. et al. sunscreens inadequately protect against ultraviolet-A-induced free radical damage. Journal of Investigative Dermatology 2003;121:862-68.
[5] Williams SN, Dienes KA. Sunscreen Sales, Socio-Economic Factors, and Melanoma Incidence in Northern Europe: A Population-Based Ecological Study. SAGE Open October-December 2014: 1–6.
[6] Matsuoka LY, Ide L, Wortsman J, MacLaughlin JA, Holick MF. Sunscreens suppress cutaneous vitamin D3 synthesis. Journal of Clinical Endocrinology & Metabolism 1987; 64:1165-68.
[7] Elizabet saes da SILVA, Roberto TAVARES, Felipe da silva PAULITSCH, Linjie ZHANG4. Eur J Dermatol 2018; 28(2): 186-201.
What do you know about melanoma?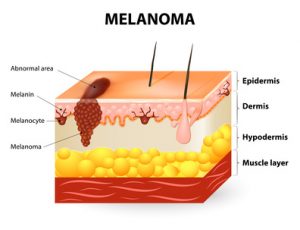
May is Melanoma Awareness Month, Therefore, we will discuss some truths to be aware of:
- First of all, seventy-five percent of these cancers occur on areas of the body that are seldom or never exposed to sunlight.[1] For example, research has shown that melanomas in women occur primarily on the upper legs, and in men more frequently on the back—areas of little sun exposure.
- Most noteworthy, in the U.S., sun exposure has decreased by about 90% since 1935. In the same time, melanoma incidence has increased by 3,000%! [2] [3] [4]
Dr. Diane Godar furnishes this exceptionally important melanoma information:[5]
- The same as in the US, while sun exposure in Europe has profoundly decreased, there has been a spectacular increase in the disease.
- Men who work outdoors have about half the risk as men who work indoors. Hence, sun exposure could not be the cause.
- in addition, outdoor workers, while receiving 3-9 times the sun exposure as indoor workers, have had no increase in melanoma since before 1940, whereas the incidence in indoor workers has increased steadily and exponentially.
- Especially relevant is that sunscreen invention, along with its steadily increasing use, has not reduced the risk of melanoma. Rather, the disease has increased as sunscreen use has increased.
- Increasing melanoma incidence significantly correlates with decreasing personal annual sunlight exposure.
- Also, outdoor workers get many sunburns but still have dramatically lower risk of contracting the disease.
So, since melanoma increases as sun exposure decreases, should we continue to blame the sun?
Here are more facts you should know about the causes of melanoma:
- First of all, people in the highest quintile (fifth) of alcohol consumption have a 65% increase in risk.[6]
- Weekly meat consumption increases the risk of melanoma by 84% and daily fruit consumption reduces the risk by nearly 50%.[7]
- Furthermore, those with the highest levels of blood PCBs have 7-times the risk compared to those with the lowest levels.[8]
- Recent use of Viagra is associated with an 84% increase in risk, and long-term use of the drug is associated with a 92% risk increase.[9]
- Finally, there is a positive association between melanoma and obesity.[10]
Furthermore, Dr. Adele Green found that the strongest risk factor for both limb and trunk melanoma was moles. The presence of more than 10 moles on the arm predicted a 42-times increased risk.[11]
Therefore, please stop blaming the sun. Safely embrace the non-burning sun and reduce your risk of melanoma.
References:
[1] Crombie IK. Distribution of malignant melanoma on the body surface.Br J Cancer. 1981 Jun;43(6):842-9.
[2] Melanoma International Foundation, 2007 Facts about melanoma. Sources: National Cancer Institute 2007 SEER Database, American Cancer Society’s 2007 Facts and Figures, The Skin Cancer Foundation, The American Academy of Dermatology.
[3] Ian D. Wyatt and Daniel E. Hecker. Occupational changes in the 20th century. Monthly Labor Review, 2006 pp 35-57: Office of Occupational Statistics and Employment Projections, Bureau of Labor Statistics.
[4] US Congress, Office of Technology Assessment, Catching Our Breath: Next Steps for Reducing Urban Ozone, OTA-O-412 (Washington, DC: US Government Printing Office, July 1989).
[5] Stephen J Merrill, Samira Ashrafi, Madhan Subramanian & Dianne E Godar. Exponentially increasing incidences of cutaneous malignant melanoma in Europe correlate with low personal annual UV doses and suggests 2 major risk Factors. Dermato-endocrinology 2015;7:1
[6] Millen AE, Tucker MA, Hartge P, Halpern A, Elder DE, Guerry D 4th, Holly EA, Sagebiel RW, Potischman N. Diet and melanoma in a case-control study. Cancer Epidemiol Biomarkers Prev. 2004 Jun;13(6):1042-51.
[7] Gould Rothberg BE, Bulloch KJ, Fine JA, Barnhill RL, Berwick M. Red meat and fruit intake is prognostic among patients with localized cutaneous melanomas more than 1 mm thick. Cancer Epidemiol. 2014 Oct;38(5):599-607.
[8] Gallagher RP, Macarthur AC, Lee TK, Weber JP, Leblanc A, Mark Elwood J, Borugian M, Abanto Z, Spinelli JJ. Plasma levels of polychlorinated biphenyls and risk of cutaneous malignant melanoma: a preliminary study. Int J Cancer. 2011 15;128(8):1872-80.
[9] Li WQ, Qureshi AA, Robinson K, Han J. Sildenafil use and increased risk of incident melanoma in US men: a prospective cohort study. JAMA Intern Med. 2014 Jun;174(6):964-70C
[10] Karimi K, Lindgren TH, Koch CA, Brodell RT. Obesity as a risk factor for malignant melanoma and non-melanoma skin cancer. Rev Endocr Metab Disord. 2016 Sep;17(3):389-403.
[11] Green AC, Siskind V. Risk factors for limb melanomas compared with trunk melanomas in Queensland. Melanoma Res. 2012 ;22(1):86-91.
![]() Sunscreen may be lethal. Yet, there have been suggestions that everyone wear it all day long, including during winter. Furthermore, some are now suggesting that we also wear a special new sunscreen at night. Why? Because, supposedly, this would protect us from the damage that may have already occurred during daytime sun exposure.[1] It seems that the most appropriate description of this message is “insanity.” If the sunscreen used in the day did not prevent damage, why would we need it at night?
Sunscreen may be lethal. Yet, there have been suggestions that everyone wear it all day long, including during winter. Furthermore, some are now suggesting that we also wear a special new sunscreen at night. Why? Because, supposedly, this would protect us from the damage that may have already occurred during daytime sun exposure.[1] It seems that the most appropriate description of this message is “insanity.” If the sunscreen used in the day did not prevent damage, why would we need it at night?
Here is your answer regarding sunscreen:
The assault against the sun is a ploy to sell a product. The sellers are doing well. For example, sunscreen sales are a multibillion-dollar business. Especially relevant is the fact that sales in 1972 were about $18 million per year.[2] But, the total USA market for sunscreens in 2005 had climbed to $640 million a year.[3] In 1972 dollars it is equivalent to $320 million, an almost 18-fold increase. However, those figures pale by comparison with figures from 2013: The global sun care market generated 5.6 billion US dollars from its sun-protection products segment. This segment includes sunscreens—many of which are ingredients in cosmetics.[4]
Most noteworthy is this important fact: the first sunscreens appeared about seven decades ago, and melanoma risk has increased by about 3,000% since that time.[5] It seems like more sunscreens = more melanoma. Consequently, we cannot recommend these noxious products. However, the manufacturers of these products can never satiate their lust for more money. Hence, they and their accomplices are now suggesting 24-hour application.
The Powers of Darkness; purveyors of sunscreen.
The Skin Cancer Foundation, which takes donations from many sunscreen manufacturers, has stated: “for adequate protection against melanoma, non-melanoma skin cancers and photo-aging, everyone over the age of six months should use sunscreen daily year-round, in any weather.” Due to this advice, sunscreen sales go ballistic, while the public suffers poor health. Yes, they are suggesting we use their products even in cloudy weather in the winter! How convenient, for an organization that receives sunscreen dollars, to make such a statement. Could it be due to a conflict of interest here?
Consider common sense when considering sunscreen! 
Each year sunscreen sales increase, and as a result, each year melanoma incidence increases? Does it seem like there is something wrong with that scenario? Those who insist on 24-hour-per-day sunscreen use, probably missed an important study. It compared 571 people with a first diagnosis of melanoma with 913 healthy control subjects. The results, were that those who used sunscreens, were 1.8 times more likely to contract melanoma than those who did not. And, among those who always used sunscreens, so they could stay out longer in the sun, the risk of melanoma was 8.7 times greater than those who did not use them.[6]
How do you protect from too much sun exposure? Not sunscreen!
You may begin to redden or feel too hot. Maybe you should remove yourself from the sunlight? Most of all, do not use sunscreens. And, you should cover up or seek the shade. That is the way God (or Nature if you prefer) intended it. In conclusion, remember that non-burning sunlight is a friend, so enjoy your friend!
[1] Sanjay Premi, Silvia Wallisch, Camila M. Mano Adam B. Weiner, Antonella Bacchiocchi, Kazumasa Wakamatsu. Chemiexcitation of melanin derivatives induces DNA photoproducts long after UV exposure. Science 20 Feb 2015:347: 6224, 842-847.
[2] Moss, R. Another Dissident Dermatologist. Cancerdecisions.com Newsletter. 2005.
[3] Bonner, C. Contact Kline Co.http://www.klinegroup.com/
[4] http://www.statista.com/topics/1990/sun-care-industry/
[5] Melanoma International Foundation, 2007. Facts about melanoma. Sources: National Cancer Institute 2007 SEER Database, American Cancer Society’s 2007 Facts and Figures, the Skin Cancer Foundation, the American Academy of Dermatology.
[6]Westerdahl J, Ingvar C, Mâsbäck A, Olsson H. Sunscreen use and malignant melanoma. Intern J Cancer 2000;87:145-50.
 In research on rheumatoid arthritis, involving studies done on nurses, an interesting result emerged.[1] It was found that among nurses 30-55 years of age who were assessed in 1976, and followed until 2008, there was an inverse association between sun exposure and the risk of rheumatoid arthritis. Those who were exposed to the greatest sun exposure had a 21% reduced risk of the disease. However, among nurses 25-42 years of age who were assessed in 1989 and followed until 2008, rheumatoid arthritis was not associated with greater sun exposure.
In research on rheumatoid arthritis, involving studies done on nurses, an interesting result emerged.[1] It was found that among nurses 30-55 years of age who were assessed in 1976, and followed until 2008, there was an inverse association between sun exposure and the risk of rheumatoid arthritis. Those who were exposed to the greatest sun exposure had a 21% reduced risk of the disease. However, among nurses 25-42 years of age who were assessed in 1989 and followed until 2008, rheumatoid arthritis was not associated with greater sun exposure.
The authors of the researchers offered an explanation regarding the disparate results. They felt that the greater use of sunscreen among the younger subjects
may have made the difference.
I agree with that idea. Sunscreen would have decreased the availability of vitamin D production, which may have lead to the lack of a protective effect on rheumatoid arthritis among the younger nurses.
Rheumatoid arthritis is a disease which causes chronic inflammation of the joints, the tissue around the joints and even in certain organs in the body.[2] It is an autoimmune disease such as lupus, multiple sclerosis and seasonal vitamin D declines may trigger it.[3] Vitamin D is an anti-inflammatory hormone and declines in vitamin D levels, of course, are a result of decreasing sun exposure in colder seasons.
Arthritic joints carry another devastating side effect. Hip replacement surgery is often prescribed for arthritic conditions, and those people who go through total-hip-replacement procedures are 4.7 times as likely to have an ischemic stroke, and 4.4 times as likely to have a hemorrhagic stroke in the first two weeks post surgery.[4] Those stroke risks remain elevated for 6-12 weeks. The term “ischemic” means producing a local deficiency of blood supply by obstructing blood flow.
I would be remiss if I did not also mention the transcendent importance of anti-inflammatory nutrition program. Sunlight is important but what you eat is critical. I would suggest that you google “anti-inflammatory diet.” Learn which foods (primarily fruits and vegetables) will help to decrease or prevent the inflammation that leads to RA. In the meanwhile, enjoy some safe, non-burning sunbathing.
[1] Arkema EV, Hart JE, Bertrand KA, Laden F, Grodstein F, Rosner BA, Karlson EW, Costenbader KH. Exposure to ultraviolet-B and risk of developing rheumatoid arthritis among women in the Nurses’ Health Study. Ann Rheum Dis. 2013 Apr;72(4):506-11
[2] Medicinenet.com. Definition of rheumatoid arthritis. http://www.medterms.com/script/main/art.asp?articlekey=5354.
[3] Cutolo M, Paolino S, Sulli A, Smith V, Pizzorni C, Seriolo B. Vitamin D, steroid hormones, and autoimmunity. Ann N Y Acad Sci. 2014 May;1317:39-46.
[4] Lalmohamed A, Vestergaard P, Cooper C, de Boer A, Leufkens HG, van Staa TP, de Vries F. Hip replacement surgery and stroke. Stroke 2012;43(12):3225-9.
Vitamin D deficiency is increasing rapidly in spite of the fact more people are taking supplements than ever before. According to an article in the Daily Mail (UK), 75% or the U.S. population are deficient in Vitamin D, and among African Americans, 95% are deficient.[1] Recent research in the Journal of the American Osteopath Association places the blame for this deficiency squarely on two factors: (1) sun deprivation through sunscreen use, and (2) chronic diseases.[2]
The paper makes perfect sense. It is known sunscreen use can inhibit up to 99% of the production of vitamin D by the skin.[3] And of course, chronic diseases themselves may be the effect of sunlight/vitamin D deficiency. So, in trying to prevent sunburn and skin damage, we set ourselves up for a spate of illnesses.
Caution is the best prevention for sunburn. One should never stay out until the skin turns red, and in the beginning stages of sun exposure, one should gradually increase it until a tan develops. A tan is a sign the skin is protecting itself against burning. In a landmark paper published in 1993 in the journal Preventive Medicine, Dr. Gordon Ainsleigh stated, “As melanoma research has demonstrated, the best prevention is regular exposure, thereby maintaining a protective tan and high vitamin D blood and tissue levels.”[4] And we now know that sun exposure produces photoproducts beyond vitamin D, such as nitric oxide, endorphins, and serotonin. Staying out of the sun, or blocking its rays, are recipes for health disasters. Queensland, Australia has vigorously promoted sunscreen for decades, and Queensland now has one of highest rates of melanoma in the world,[5] along with a rate of vitamin D deficiency which is becoming critical.[6] The answer from the dermatologists, of course, is to prescribe more sunscreen and frighten more people out of the sun. Is that not the most counterintuitive decision of the century?
A much better choice than sunscreen is to simply leave the sun when it becomes too intense, or cover up with light, reflective clothing. Enjoy the sun, but do it carefully and never burn. And don’t destroy all the salubrious effects of the sun by using a noxious sunblock.
[1] http://www.dailymail.co.uk/health/article-4462730/Too-sunscreen-making-vitamin-D-deficient.html?ITO=1490&ns_mchannel=rss&ns_campaign=1490
[2] Pfotenhauer KM, Shubrook JH. Vitamin D deficiency, its role in heath and disease, and current supplementation recommendations. J Am Osteopath Assoc. 2017; 117(5):301 – See more at: http://www.ajmc.com/newsroom/sunscreen-use-chronic-disease-linked-to-vitamin-d-deficiency#sthash.Yfx4Rbny.dpuf
[3] Matsuoka LY, Ide L, Wortsman J, MacLaughlin JA, Holick MF. Sunscreens suppress cutaneous vitamin D3 synthesis. Journal of Clinical Endocrinology & Metabolism 1987; 64:1165-68.
[4] Ainsleigh G. Beneficial effects of sun exposure on cancer mortality. Preventive Medicine 1993;22:132-140.
[5] Garland CF, Garland FC, Gorham ED. Could sunscreens increase melanoma risk? American Journal of Public Health, Vol. 82, No. 4, April 1992, pp. 614-15.
[6]Van der Mei IA, Ponsonby AL, Engelsen O, Pasco JA, McGrath JJ, Eyles DW, Blizzard L, Dwyer T, Lucas R, Jones G. A high vitamin D insufficiency across Australian populations and latitude. Environmental Health Perspect 2007;115:1132-39.
By Marc Sorenson, EdD. Sunlight Institute…
Most people believe that melanoma incidence is increasing rapidly, and that complete avoidance of sun exposure is the answer to preventing the disease. And of course, we must always wear sunscreen, even in the winter. Occasionally, however, there are research studies that belie those beliefs and quite simply show that sunscreens are at best worthless and at worst toxic.
A very-well-done piece of research in Northern Europe compared melanoma incidence rates with sunscreen use during a period of time from 1997-1999 to 2008 and 2012.[1] One of the most interesting findings was that higher income people had significantly higher melanoma incidence, and that increased sunscreen use by those people had not prevented them from being at higher risk of melanoma. In other words, we see this equation: Higher sunscreen use=higher melanoma risk! We know that people who work outdoors regularly have far less risk of melanoma than those who work indoors.[2] This research backs that fact, because it is obvious that higher-income people spend much more time indoors that poorer people who work outside. Those higher-income people also have more money to spend on sunscreens.
Possibly one of the most profound assessments of sunscreen use and melanoma risk was done by Case Adams, a naturopath. In an article entitled Melanoma Rates Double as More Use Sunscreen, Fewer Sunbathe,[3] he analyzes sunscreen sales statistics from Prezi market analysis. He then demonstrates that sunscreen sales between 1982 and 2012 increased by 38 times or 3800%. During the same years, melanoma risk doubled! He also notes that the number of people who sunbathe has profoundly decreased. Anyone who thinks that increasing sunscreen use has led to a reduction in melanoma is wandering around in the darkness of denial! Dr. Adams also makes this interesting statement: “Thus we cannot logically equate the growth of skin cancer with an increase in sun exposure.”
The best protection against melanoma is regular sun exposure. Safely enjoy it!
[1] Williams SN, Dienes KA. Sunscreen Sales, Socio-Economic Factors, and Melanoma Incidence in Northern Europe: A Population-Based Ecological Study. SAGE Open December 14;1-6.
[2] Garland FC, White MR, Garland CF, Shaw E, Gorham ED. Occupational sun exposure and melanoma in the USA Navy. Arch Environ Health 1990; 45:261-67.
[3] http://www.realnatural.org/melanoma-rates-double-as-more-use-sunscreen-fewer-sunbath/
By Marc Sorenson, EdD. Sunlight Institute….
I sent this letter to a good friend who just suffered a triple compression fracture while doing yoga. She is a dynamic and accomplished person who has been a competitive athlete for much of her life, and has helped many people to save their lives from various diseases through her books and lectures. Many would think her vegan lifestyle would have protected her against weak bones. However, after having a common skin cancer appear on her body, her dermatologist told her to avoid the sun. She stopped most of her sun exposure and didn’t take vitamin D. Her bones had previously been exceptionally strong for her age. Obviously, the change in sun habits had very deleterious effects, as I explained in the letter. Her name has been changed for the purpose of this blog.
Dear Barbara,It is great to hear from you! I only wish the circumstances were better for you.Unless you are sunbathing regularly, the recommendation for 1,000 IU of vitamin D is woefully inadequate. For someone with weak bones, 5,000 IU would be my suggestion. Does my memory serve me right about your having a skin cancer? If you started avoiding sun exposure after that time, then that is the reason for your bone weakness. Sun exposure is the best way to obtain vitamin D and many other photoproducts such as nitric oxide and serotonin. Endorphins are also produced by sun exposure.Women in Spain who actively seek the sun have about 9% of the risk of a fracture as women who stay indoors. Or stated another way, women who avoid the sun have 11 times the risk of fracture. And of course, the few fractures experienced by sun seekers are probably due to some traumatic incident, not weak bones. Sunning per se is far more effective than vitamin D supplementation per se for producing and maintaining strong bones. Sun exposure is also far more effective that a vegan diet, although the diet certainly reduces the risk. Nonetheless, vegans who avoid the sun, because they believe their alkaline diet will totally protect them, are setting themselves up for fractures. Athletes who believe that exercise will protect them are also making a mistake. Sun is the great bone protector.For light-skinned Caucasians, 20 minutes of unprotected sun exposure at midday, on each side of the body, will produce about 20,000 IU of vitamin D. Naked at noon is the best, if you can find a place to be private. Don’t burn as your skin becomes used to it. Remember also that melanoma, the deadly skin cancer, is about twice as common among indoor workers as outdoor workers who are habitually in the sun. Occasional blasts of sun that burn you, however, may increase the risk. Don’t burn. “Habitually” is the operative word for sunbathing.The non-melanoma skin cancers(NMSC), aka common skin cancers, are a different story; sun exposure does increase the risk. However, these cancers are almost never fatal, and if caught early can be removed immediately. People who have high numbers of these cancers have far fewer melanomas. Also, your diet of dark greens and colorful fruits such as blackberries, raspberries, pomegranates, is protective against developing these cancers.Remember also that sunscreens are deadly and their use is associated with an increase in melanoma. They will halt vitamin D production by about 99% in the area that is covered with them.I would suggest that you go to my blog site, http://sunlightinstitute.org/ and search osteoporosis, bone and fracture. I wrote a short article last week on osteoporosis in sunny areas (reason: too much indoor living, and too much clothing). There are many more blogs on the site that talk about bone strength. Go to News and then use the search bar there.Another suggestion. If you still have my book Vitamin D3 and Solar Power, read the section on bone health. There is much more information now, but the information in the book will serve as a guide.My new book, Embrace the Sun should be available sometime this summer.One last thought, women who totally avoid the sun are at 1,000% increased risk for breast cancer compared to women who are regularly exposed.Sunshine and blessings,MarcDon’t make Barbara’s mistake. Safely soak up some midday sun and preserve your bones.

