Cytokine storms may cause death and destruction during coronavirus (Covid-19) infection. Therefore, we should take measures to prevent them. In that manner, we can shorten the lethal path of Covid 19.
Answers to the coronavirus epidemic. By Marc Sorenson, EdD
Cytokine storms are major causes of death from coronavirus (Covid-19) and resultant pneumonia.
- This article will present information showing that we may have the tools needed to suppress coronavirus (Covid 19).
- The article will explain how the cytokine storm kills persons with coronavirus infection.
- It will explain the role of vitamin D in suppressing the cytokine storm.
- The presentation will show that non-burning, regular sun exposure is superior to taking a vitamin D supplement.
- It will show, graphically, the seasonal nature of flu-like diseases and make it clear where the sun fits in.
- The article will show the efficacy of sunlight for Covid-19, both outside and inside the body.
- The presentation will include information on the terrific increase in death among African Americans. African Americans need far more sun exposure than people with lighter skin.
- It will present information on the incredibly healthful effects of sunlight both with and beyond vitamin D.
- This article will expose the lies and present the truth about melanoma, to remove the fear of sun exposure for that disease.
- The presentation will elucidate the concerns about different skin types, and present them graphically.
- The presentation will also articulate the truth about sunscreens and explain the best method for preventing damage once one has had sufficient sun exposure.
- The article presents methods to keep vitamin D levels high in areas of little sunlight. It also presents the means to survive winter, when no UVB light exists to produce vitamin D.
- The presentation will discuss information on obesity, diabetes and heart disease, which are each associated closely to death from Covid-19.
- This discussion provides information showing that sunscreen use may quash the ability of sunlight to produce vitamin D. This will inhibit the body’s ability to stop the cytokine storm.
Breaking news!
As I prepared to post this article, Yahoo released news of transcendent importance. They corroborated statements about sunlight being able to kill Coronavirus. I had been making this statement since the first onslaught of the virus. Some people agreed and some ridiculed me. This Yahoo information from the DHS vindicates me!
The headline reads Sunlight destroys virus quickly. [Emphasis mine]. They also stated that “simulated sunlight” killed the virus. The government tests proved the efficacy of sunlight. The remainder of this article now has an even greater validity.
What is coronavirus or Covid-19?
Coronaviruses are a group of viruses that infect birds and mammals. These viruses infect the respiratory passages with such diseases as influenza and the common cold. They also lead to some severe diseases such as Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS). The most recent of these diseases is Covid-19.
An important fact: the most severe respiratory pandemic was the Spanish flu of 1918-1919, which probably killed 50-100 million people. This flu started in March 1918. Vitamin D levels would have been lowest during that time. The flu subsided during the summer (time of highest vitamin D levels), and rebounded with a vengeance in the fall.
A second important fact: If you die from coronavirus, it is likely that your own immune system will kill you. You will die from a cytokine storm.
What is a cytokine?
A cytokine is a specialized protein molecule that attacks and destroys an infection. These proteins can be either pro-inflammatory of anti-inflammatory. For our purposes, we will primarily discuss pro-inflammatory cytokines.
What is a cytokine storm? Usually, the cytokine needed to fight the infected tissue stops its attack after it has won the battle. However, in the case of a disease like influenza (or Covid-19), “friendly fire” occurs. The body’s immune system recruits millions of “extra” or reinforcing cytokines, and those cytokines mount an overwhelming attack against the tissue they initially protected; in other words, they cause a storm. Cytokine storms lead to severe inflammation that weakens or destroys blood vessel membranes in the lungs. This causes fluid to seep through to the air sacs, which leads to pneumonia. A person then ends up drowning in his own body fluids. Dr. Angela Rasmussen describes it thusly: “Basically you’re bleeding out of your blood vessels.” She goes on to say that the problem may not end there. The storm spills into the circulatory system and can create systemic issues across multiple organs.
Does vitamin D thwart the cytokine storm?
Vitamin D leads to the production of cathelicidins and defensins, which are peptides (proteins) with antimicrobial properties. According to Dr. William Grant and colleagues, these peptides lower viral replication rates and reduce concentrations of pro-inflammatory cytokines. These cytokines produce the inflammation that injures the lungs. Nevertheless, the damage does not necessarily end in the lungs.
Recent research shows that the damage from Covid-19 can spread to multiple organ systems. The report on this research suggests that the cytokine storm may be responsible for that spread. The heart, liver, kidneys, neurological system and gastrointestinal tract may all be targets of Covid-19 beyond the lungs.
In addition, Dr. Grant and colleagues list the following reasons to believe that vitamin D could reduce the risk of the coronavirus:
- Inducing production of cathelicidins and defensins that can lower viral survival and replication rates as well as reduce risk of bacterial infection
- Reducing the cytokine storm that causes inflammation and damage to the lining of the lungs that can lead to pneumonia
- Additionally, vitamin D deficiency contributes to acute respiratory distress syndrome, a major cause of death associated with COVID-19.
If what I posit were true, we would expect Covid-19 to be higher in populations with high vitamin D deficiency, and such is the case.
Henry Lahore, one of the great vitamin D scholars, has listed four racial groups with disproportionately high vitamin D deficiency: Elderly Italians, Spanish, Swedish Somalis and African Americans.
Many of you have read of the alarmingly high Covid-19 death rate in African Americans. From my previous research, I know that African Americans also have alarmingly low vitamin D levels. Lahore also cites research that shows 84% of African Americans are vitamin D deficient. In addition, in Chicago, 70% of Covid 19 deaths are among Blacks. The reason for the deficiency? Dark skins take much more time in the sun to produce vitamin D. Unfortunately, our answer to Covid-19 has been to cocoon everyone indoors, which assures that no one can obtain any vitamin D except by supplement; that is, unless they are fortunate enough to own sunlamps or sunbeds (tanning beds).
An alarming situation in Sweden
Even more alarming is that the Swedish Somali population has 40% of the deaths in Sweden. Yet, they comprise only .84% of the Swedish population. In other words, the Dark-skinned Somalis have 4,700% greater risk of death from Covid 19! This can only be due to lack of sufficient sunlight and subsequently, low vitamin D. No such death risk exists in Africa, where sunlight is abundant.
Does sun exposure make a difference?
We live in a world that is mostly vitamin D deficient. Even sunnier states and countries have an increasing problem. However, Northern countries are at much more risk for Covid-19. The reason for the growing risk in sunny countries is the misguided advice to stay out of the sun and wear sunscreens, which can stop the production of up to 99% of vitamin D. I believe we must stop shunning the sun if we wish to halt flu epidemics, including the current Covid-19 epidemic. Otherwise, we will spend our time pursuing vaccines for a disease whose answer is already available. The real pandemic is the pandemic of sunlight deficiency.
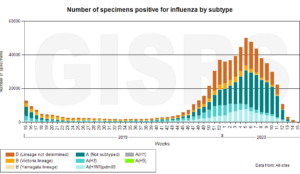
If sunlight makes a positive difference for flu, and suppresses the cytokine storm, we would expect to see decreases in flu during the sunny season.
This is exactly the case. Consider the following chart: (Produced by WHO), sent to me by Goran Olsson, Moscow, Russia).
Observe what happens in the sunny part of the year. The incidence of flu virtually disappears. So, when the experts hypothesize that Covid 19 will spike again this fall, they are correct. That is, unless corrective measures are taken.
There are those who believe that warm temperature halts flu in summer. However, if that were true, we would need only to turn our thermostats up to 90 degrees to kill the virus and stop the cytokine storm. It is sunlight, not warm temperature, which is the great healer.
There are two ways in which sunlight helps halt the flu and probably Covid 19.
First, exposure to sun produces 90% of serum (blood) vitamin D. Supplementation or food sources produce only a minuscule quantity of vitamin D. Full-body sun exposure for 10-15 minutes can cause the skin to produce 20,000 IU of vitamin D. Based on this fact, here is the effect of sun exposure on the Covid 19 equation:
Sunlight-> vitamin D ->inhibition of the cytokine storm-> Prevention or stoppage of death from Covid-19.
Secondly, sunlight is the best disinfectant, and many viruses live longer outside the body when sunlight is lacking. Whether this is true for Covid-19 is conjecture. It would be good to do that research now. Regularly disinfecting homes with UV light would be easy and safe.
A common and dangerous misconception regarding sun exposure and vitamin D: “I don’t need sunshine; I need only vitamin D supplements.”
This statement shows a lack of knowledge. If we are to use sunlight to ramp up our vitamin D and other healthful photoproducts, we must stop fearing the sun. If we want to shut down the cytokine storm, we must develop a friendly, but careful relationship with sunlight. For health, sun exposure goes far beyond vitamin D. Here are more benefits of sunlight, including, but not limited to the benefits of vitamin D. For full documentation of these statements, read Embrace the Sun by Drs. Marc Sorenson and William Grant.
The prevention or reversal of the diseases underlined below do not depend on vitamin D.
- Influenza diminishes almost to nothing during late spring, summer, and early fall, times of greatest sun exposure and vitamin D production. See the graph above.
- Seventy-five percent of melanomas occurs on areas of the body seldom or never exposed to sun.
- Women who sunbathe regularly have half the risk of death during a 20-year period compared to those who stay indoors.
- A Spanish study shows that women who seek the sun have one-eleventh the hip-fracture risk as sun avoiders.
- Men who work outdoors have half the risk of melanoma as those who work indoors.
- Women who avoid the sun have 10-times the risk of breast cancer as those who embrace the sun.
-
More benefits of sunlight exposure
- Multiple sclerosis (MS) is highest in areas of little sunlight, and virtually disappears in areas of year-round direct sunlight.
- Sun exposure decreases heart disease risk through nitric oxide production.
- Sun exposure dramatically improves mood through production of serotonin.
- Those persons who spend many hours daily outdoors have only 1/50 the risk of Parkinson’s disease!
- For each death caused by diseases associated with sun exposure, there are 328 deaths caused by diseases associated with sun deprivation.
- Sun exposure increases the production of BDNF, essential to nerve function.
- Sun exposure can produce as much as 20,000 IU of vitamin D in 20 minutes of full-body sun exposure.
- In the U.S., vitamin D deficiency in children has increased by 83 times during a 14-year period. That is likely due to indoor living and sunscreen use.
Another sunlight concern, which should really be a non-concern: “if people soak up the sun, they will contract melanoma.”
To dispel this myth, here are the facts about melanoma, fully documented in the book, Embrace the Sun. This should belie the misinformation regarding melanoma and sunlight.
Seventy-five percent of melanomas occur on body areas seldom exposed to sunlight.
- In the U.S., as sun exposure has decreased by about 90% since 1935, melanoma incidence has increased by 3,000%. Documentation in Embrace the Sun. See the graph below.
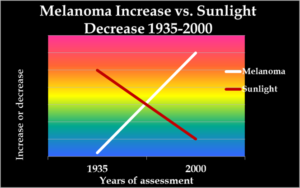
- As in the US, while sun exposure in Europe has profoundly decreased, there has been an exponential increase in melanoma.
- Men who work outdoors have about half the risk of melanoma as men who work indoors.
- Outdoor workers, while receiving 3-9 times the sun exposure as indoor workers, have had no increase in melanoma since before 1940, whereas melanoma incidence in indoor workers has increased steadily and exponentially.
- Sunscreen invention, along with its steadily increasing use, has not reduced the risk of melanoma. In fact, it has melanoma has increased as sunscreen use has increased. Documentation in Embrace the Sun.
- Increasing melanoma incidence significantly correlates with decreasing personal annual Sunlight exposure.
- Outdoor workers do get numerous sunburns but still have a dramatically lower risk of contracting melanoma.
Thus, melanoma increases as sun exposure decreases. Should we continue to blame the sun?
Here are more facts about melanoma and its prevention:
People in the highest quintile (fifth) of alcohol consumption have a 65% increase in melanoma risk.
- Weekly meat consumption increases melanoma risk by 84%. This is important to know for my non-vegetarian friends. (See the graph below.)
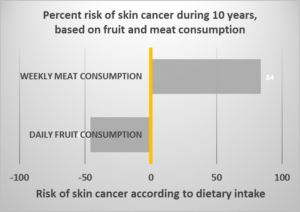
- Daily fruit consumption reduces the risk of melanoma by nearly 50%. (See the graph ).
- Persons with the highest levels of blood PCBs (now-banned industrial chemicals) have 7-times the risk of melanoma as those with the lowest levels.
- Recent use of Viagra is associated with an 84% increase in melanoma risk, while long-term use of the drug is associated with a 92% risk increase.
- There is a positive association between melanoma and obesity. It is interesting that the increases in both diseases have progressed in unison.
A caveat regarding skin type: All people need sun exposure. However, people who have type-one skin must be very cautious.
Type-one skin may not tan, and should not have direct exposure to sunlight, at least in the beginning stages of a sunning program. Nevertheless, those who have type-one skin may carefully go outside and sit in the shade with the sun shining around them, or they could sit under a beach umbrella during a sunny day. The key is the amount of time it takes to show a slight pinkness. If that time is only a minute, then the person should go inside after that minute and cover up with clothing.
How to change your environment when you have had enough sun exposure.
If it takes longer for pinkness to occur, then stay longer. After a few days, the skin will acclimatize somewhat and longer times could be enjoyed. After the sunning session, it would be appropriate to don long pants, large hat, long sleeves and light gloves. The advantage for people with type-one skins is they produce large quantities of vitamin D and other photoproducts in a very short time. They, therefore, can quickly optimize the body’s ability to suppress the cytokine storm and to derive the other benefits of sun exposure that we previously listed. Sunbathing, or “shade bathing,” for those with type-one skin is the best way to obtain vitamin D.
Important information for African Americans, who need more vitamin D to suppress the cytokine storm.
In addition, this is a message to our two dear friends (African Americans) in San Francisco. You must spend much more than 10-15 minutes in the midday sunlight to optimize your vitamin D levels. Try to get at least 40-60 minutes of full-body exposure on each side of the body. This of course, applies to all African Americans. As with all races, be careful not to burn. For a person with very dark skin (type five-six) on the graph below, it takes an hour to produce the same quantity of vitamin D that a type-one can produce in a few minutes.
The following is a chart for determining skin type. Remember, that for every skin type, the primary warning is to avoid sunburn.
Many people believe that a few minutes outside, with face and hands exposed, will optimize vitamin D levels. However, that method takes far more than a few minutes to produce optimization. It may take all day, according to your skin type. If you find an area to sunbathe at midday with little or no clothing, you can produce up to 20,000 IU of vitamin D in as little as 10-15 minutes on each side of the body. After that, you can cover up with long pants, a large hat, long-sleeve shirt and even light gloves and continue to enjoy the outdoors.
An important statement from dermatologists and other organizations in the UK.
Here is a related statement from several health organizations in the UK, including the British Association of Dermatology (hard to believe, I know) “Vitamin D is essential for good bone health, and for most people sun is the most important source of vitamin D. The time required to make sufficient vitamin D varies according to a number of environmental, physical and personal factors, but is typically short and less than the amount of time needed for skin to redden and burn. Enjoying the sun safely, while taking care not to burn, can help provide the benefits of vitamin D without unduly raising the risk of skin cancer.” Documented in Embrace the Sun.
What about Areas of little sunlight?
However, suppose you live in unpredictable sun areas like Ely, Nevada or Ely, Minnesota, or Olympia, Washington or Toronto, Canada. As long as you can access unobstructed, midday summer sunlight twice weekly, as described above, you can count on optimized vitamin D levels. There is an exception for African Americans. An extra day per week would probably be a good idea.
Remember, no vitamin D production occurs during early morning of late afternoon. Nevertheless, many other healthful effects of sunlight are available all day long. Also, remember that in the beginning stages of your suntanning program, be careful not to burn yourself. If you begin to redden, leave the sun. Gradually acclimatize your skin to the sun.
Other facts about Covid-19, death and the cytokine storm:
Obesity is a major factor.
Obesity increases the risk of death from Covid-19. It is an inflammatory disease, as is Covid-19. In addition, it appears that a combination of the two can be deadly. This is predictable, because both the cytokine storm and obesity are inflammatory conditions. It is like pouring gasoline on a fire.
New York is the epicenter for Covid-19 in the U.S. NYU has determined that obesity and age are the two major deciding factors for hospitalization there.
People are thinner when they are outdoors and active.
Thus, the cocooning is likely adding to the likelihood of obesity. In addition, stay-at-home orders are neither conducive to sun exposure nor vitamin D optimization. I do not have the research to prove this point, but I believe that the enforced indoor living has added to the obesity crisis. How many bowls of ice cream do cocooned people consume nightly in front of the TV?
In our sun-drenched health resort, our clients lost more than 100 tons of fat during our careers. Much of that success was due to a mostly animal-free nutrition program. Yet, sun exposure does reduce weight. This is especially true of early-morning sun exposure. Early-morning sun exposure reduces obesity without the benefit of vitamin D. We know this to be true, because early morning sun exposure does not contain the UVB light necessary for vitamin D production. Nitric oxide or serotonin, produced throughout the day, could be the operative factors.
Type-two Diabetes is a major factor for death from Covid-19. Type-one is probably a factor also, but it comprises only 5% of cases. In addition, studies do not exist on the relationship of type-1 to Covid-19. Diabetes, then, is either directly or indirectly associated with the cytokine storm.
According to Morbidity and Mortality Weekly Report, Covid-19 patients taken to the ICU were more likely to have diabetes than any other underlying condition. In our former health resort (very sunny), two-thirds of type-two diabetics were free of all diabetic medications, including injected insulin, in 11.7 days. That number reached 85% in those who stayed four weeks. Of the 15% that were still using medication, almost all of them dramatically reduced their dosages. If people would simply embrace the sun and eat a plant-based diet, diabetes would cease to be a problem. Why? Because diabetes would mostly cease to exist.
Research on sunlight and diabetes:
Several papers have shown an association between sun exposure and diabetes. One paper showed that blood-sugar levels were lower during the summer, and another demonstrated that exposure to sun lamps increased insulin secretion.
In addition, a meta-analysis produced evidence that recreational sun exposure is associated with a reduced risk of type-two diabetes. The study was undertaken because the researchers observed that higher vitamin D levels were consistently associated with lower diabetes risk. Yet, there was not a relationship between vitamin D supplementation and diabetes. I must make a point here: Do not trust a vitamin D capsule to have all the health benefits of sun exposure or other UVB exposure.
Heart disease (cardiovascular disease) is a major factor for death from Covid-19.
Research from the same journal, Morbidity and Mortality Weekly Report, showed “10 % percent of COVID-19 patients with cardiovascular conditions died — the highest rate of fatalities among common underlying conditions — compared with 2.3 percent of the entire population of patients.” At our health resort, clients reduced cholesterol levels (predictive of heart disease, stroke and other vascular diseases) by as much as 700 points.
In addition, they sometimes lowered blood pressure remarkably in only one-four weeks. Angina often disappeared. In my opinion, the plant-based nutrition program, and the predictable sunny days in Saint George, Utah, both contributed to those results. One of our clients who had scheduled himself for open-heart quadruple bypass surgery, checked in at the health institute instead. His heart disease never gave him another problem. He was about 65 years old at that time and is now about 87. He never had a bypass operation.
Research on sunlight and heart disease.
Research indicates that sun exposure in summertime among gardeners correlates to lower cholesterol levels and decreased risk of heart attack. HDL cholesterol is protective against heart disease, and LDL cholesterol is a risk factor. A study in Chile showed that HDL decreases in the winter, and LDL is significantly higher in winter/spring than in summer. Of course, sunlight is much more prevalent in summer, hence the difference. A study on seasonal variations in heart attack rates in Brazil demonstrated a 30% higher risk in winter than summer. One study of hypertensive subjects shows that blood pressure levels average 165/90 in winter but 134/74 in the summer, and both stroke and heart attack rates double in the winter. We could list dozens of additional citations, but these will suffice for this short paper.
Should we use sunscreens while we sunbathe?
The simple answer is “no.” If people feel they have had sufficient sun exposure, they should seek shade, cover up or go inside.
There are many excellent reasons NOT to use sunscreens:
Two major studies in 2019 showed that sunscreens might be worthless or even harmful. The first, a meta-analysis, showed no protective effect of sunscreens against skin cancer. The second showed that people who used sunscreens had up to six times the number of sunburns compared to those that did not use them. This research also demonstrated that those who covered up, or sought shade when they had enough sun, were far less apt to sunburn than those who used sunscreens. In addition, in the last four decades, sunscreen use has increased by 400%, while melanoma incidence has also increased by 400%.
Sunscreens are also destroying coral reefs. Hawaii has banned them. Moreover, and perhaps most importantly, research shows that an SPF 15 sunscreen will decrease sun-stimulated vitamin D production by 99.5%. If it were our desire to thwart Covid-19, and halt the cytokine storm, why would we use sunscreens that suppresses vitamin D?
One of the primary government concerns is that after the summer, Covid 19 will mount a comeback, or second wave. Indeed, it will, if something does not replace the UV light from sunlight. Along with the disease, the cytokine storm will return in force.
Let us consider winter, when sunlight no longer contains UVB light to produce vitamin D. Go to the previous chart above on seasonality of flu and look at the tremendous increase that occurs in winter. How do we keep the virus under control? The answer is to use a sunbed (tanning bed). The sunbed must not be a high-pressure bed, as those beds produce little vitamin D.
I can already hear the collective screams of agony. Those screams emanate from the American Academy of Dermatology (AAD) and others as they read the vitamin D/sunbed statement. They are yelling, “How can he advocate sunbeds!?”
Do you want to read the truth about the AAD and other anti-sun, anti-tanning organizations? Then read the book, Embrace the Sun, which contains a full exposé.
Now, let us present the documented truth about sunbeds—truth that will never be presented by the anti-sun, anti-tanning organizations. Here are the facts about the healthful effects of sunbeds:
- A 20-year study demonstrated that both sun exposure and sunbed exposure reduced the risk of death; women who used sunbeds were 23% less likely to die from any cause than women who did not use them.
-
Sunbed use is associated with increased vitamin D levels.
- People in Canada who use sunbeds have far higher vitamin D levels that the rest of the population. What a protection against the cytokine storm!
- In addition, another study showed that sunbed users had 90% higher vitamin D than non-users. The same study showed higher bone-mineral density, indicative of stronger bones.
- These impressive machines are associated with lower breast-cancer risk.
- Sunbed use can cure psoriasis and eczema, and dermatologists often recommend sunbeds.
- Thrice yearly sunbed use is associated with a 40-50% reduced risk of endometrial cancer.
- Sunbed use is associated with a reduced risk of clots.
- They are also able to alleviate pain.
Refuting the Powers of Darkness (anti-sun organizations) regarding sunbeds. The Powers of Darkness are not interested in your cytokine storms.
Sunbeds (tanning beds), as you have learned, have many healthful properties. They produce vitamin D, strengthen bone and reduce the risk of major cancers. In addition, they may hold a key to stopping Covid 19 and the cytokine storm. Yet, the Powers of Darkness continue to malign them as being a major cause of melanoma. Thus, through misguided legislation, they ban teens in many areas from using them. In addition, tanning- salon owners must live in fear of government overreach that could put them out of business.
Because of this uproar, a group of scientists (some dermatologists), led by Dr. Jörg Reichrath, did a thorough research review. Furthermore, they published their findings in 2020 in a major scientific journal called Anticancer Research. That research presented the truth about melanoma and sunbeds. Here are four results of their review:
1.A study from Europe demonstrated that sunbed use was associated with a 30% reduced risk of developing melanoma.
2.They stated, “We found no studies that demonstrate a causal relationship between moderate solarium use and melanoma risk.”
3.The anti-sun research was low quality, and bias may have existed.
So, do not believe everything you hear about sunbeds from the Powers of Darkness. My belief is that sunbeds may hold the key to stopping the winter spike in Covid-19 cases.
You should always use sunbeds at a tanning salon whose employees are skilled in assessing skin types. That will keep you safe as you optimize your vitamin D and inhibit the cytokine storm.
How do you know if your serum Vitamin D is sufficient to suppress the cytokine storm?
Everyone should have a test for vitamin D levels. The goal is to produce a level between 50 and 70 ng/ml.
How do I know my time outside is producing vitamin D?
- If the media reports a UV index of three or more, and you are outside, not using sunscreen, vitamin D production occurs.
- If your shadow is shorter than your height, you are producing vitamin D. Thus, the shorter the shadow, the better. The shadow will be shortest at midday.
- To produce the greatest amount of vitamin D, find a private area and sunbathe, using as little clothing as possible. As mentioned, this can produce up to 20,000 IU of vitamin D in as little as 10-15 minutes of sun exposure at midday.
What have you learned from this article regarding Covid 19, sunlight, vitamin D and the cytokine storm?
Here is a list:
- This article presented evidence showing that we have the information needed to suppress coronavirus (Covid 19).
- The article explained how the cytokine storm kills persons with coronavirus infection.
- It also discussed the role of sunlight and vitamin D in suppressing the cytokine storm.
- It presented information that non-burning, regular sun exposure is superior to taking a vitamin D capsule.
- The article showed, graphically, the seasonal nature of flu-like diseases.
- This paper showed the efficacy of sunlight for Covid-19, both outside and inside the body.
- The presentation included information on the terrific increase in death among African Americans with Covid 19.
-
More lessons learned regarding sunlight and cytokines.
- The information showed the incredibly healthful effects of sunlight both with and beyond vitamin D.
- The presentation exposed the lies and presented the truth about melanoma, to remove the fear of sun exposure for that disease.
- The presentation elucidated the concerns about different skin types, and presented them graphically.
- The paper articulated the truth about sunscreens and explained the best method for preventing damage once one has had sufficient sun exposure.
- It presented the methods for keeping vitamin D levels high in areas of little sunlight and explained methods for surviving winter, when no UVB light exists to produce vitamin D.
- The presentation gave information on obesity, diabetes and heart disease, which are each associated closely to death from Covid-19.
- This discussion presented information that sunscreen use may quash the ability of sunlight to produce vitamin D. This will inhibit the body’s ability to stop the cytokine storm.
The materials in this paper cover the pertinent facts about Covid-19 and sunlight. However, no one can know all the facts, and this material does not replace your personal health advisors. Consult them before making lifestyle changes.
Please share this material with your physicians, friends, parents, siblings, social-isolating acquaintances, government entities, social media, regular media, and newspapers. The information contained herein may save their health and our economy. Until then, remember that neither sunlight nor sunbeds are enemies. In fact, they may save your life!
Happy sunning!
Sunscreen chemicals. By Marc Sorenson, EdD.
 Sunscreen chemicals are toxic. I have written about them previously and did an analysis of sunscreen chemicals dangers in my book, Embrace the Sun. And now, Science Digest alerts the public of new research. It indicates that even low concentrations of sunscreen chemicals can stimulate breast tissue growth. Thus, these chemicals could lead to breast cancer. Nevertheless, these chemicals affected only breast cells that had estrogen receptors. The sunscreen chemical tested was oxybenzone, which mimics estrogen in some aspects. Oxybenzone and other similar chemicals are known as xenoestrogens. They are also suspected of many injurious effects beyond possibly causing breast cancer.
Sunscreen chemicals are toxic. I have written about them previously and did an analysis of sunscreen chemicals dangers in my book, Embrace the Sun. And now, Science Digest alerts the public of new research. It indicates that even low concentrations of sunscreen chemicals can stimulate breast tissue growth. Thus, these chemicals could lead to breast cancer. Nevertheless, these chemicals affected only breast cells that had estrogen receptors. The sunscreen chemical tested was oxybenzone, which mimics estrogen in some aspects. Oxybenzone and other similar chemicals are known as xenoestrogens. They are also suspected of many injurious effects beyond possibly causing breast cancer.
Other deleterious effects of sunscreen chemicals 1
First of all, several years ago, the CDC released a study showing that 96.8% of Americans at age six are contaminated with oxybenzone. The study also showed that women were 3.5 times as likely to have high concentrations as men.[1] The authors suggest that women’s greater use of personal-care products, most of which contain sunscreens, is the reason for their higher degree of contamination. Oxybenzone is used in 588 sunscreens and in 567 other personal-care products.[2] Another investigation showed that up to 8.7% of oxybnezone is absorbed[3] and accumulates in the body.[4] It is still found in the urine 5 days after application.
Other deleterious effects of sunscreen chemicals 2
Other research papers confirm that sunscreen chemicals are highly absorbed and then detected in urine and breast milk, where they may cause systemic effects, including disruption of the endocrine system.[5], [6]
In addition, pregnant mothers exposed to oxybenzone gave birth to babies with low birth weights, [7] which “programs” the developing child for greater risks of heart disease, hypertension, type-two diabetes and other diseases in adulthood.[8] Furthermore, sun causes the chemical to become a potent allergen[9], [10] and to form free radicals.[11], [12], [13], [14] Free radicals are unstable atoms which lack an electron in their outer shells. One study concluded, “The surprising result is UV filters applied to the skin surface not only lose their screening capability after a period of incubation, but also may lead to enhanced ROS [free radicals] generation in nucleated epidermis through photogeneration.“[15] In fact, after one hour, more free radicals were created by sunlight contacting sunscreen, than sunlight on skin. To me, this is another indication that sunscreens cause more damage than no sunscreens!
Other deleterious effects of sunscreen chemicals 3
In addition to adverse effects on human health, sunscreen chemicals have potential deleterious effects on the environment. A study from the Archives of Environmental Contamination and Toxicology, regarding the detrimental effects of Oxybenzone, stated that Oxybenzone is a photo-toxicant, meaning its adverse effects are exacerbated in the light.[16] Does this toxic chemical sound like something you’d like to apply to your skin or your children’s skin while out in the sun?
The researchers also stated: “Oxybenzone is an emerging contaminant of concern in the marine environment.” They found that a small dollop of sunscreen in six Olympic-sized pools caused a disruption of coral growth. Such disruption leads to a whitening and killing of the marine activity of coral reefs. This is accomplished by ossification of a free-swimming larva called a planula, which kills the growth of coral reefs. And this information has proven to be prophetic. Many beach areas have now prohibited the use of sunscreen chemicals due to concerns about coral-reef destruction.
The final nail in the coffin for sunscreen chemicals: they may lead to sunburns.
I have often stated that sunscreens may be worthless at best and dangerous at worst. Another scientific study accidentally corroborated my conclusion.[17] The researchers wanted to discover which sun-protection behavior was most effective in preventing sunburn. Hence, they designed a cross-sectional investigation using a nationally representative sample of about 32,000 US adults. They interviewed each participant in person. This is especially relevant when attempting to achieve the most accurate results possible. We can conclude, therefore, that their findings regarding sunscreen use and other “sun-protective” behaviors probably have validity. Seeking shade, wearing a hat or visor, and wearing long sleeves and or pants were other sun-protective behaviors included.
The results:
Fifty-four percent of the subjects were women, and 15,992 of all individuals were considered sun-sensitive (fair skinned). Those who used only sunscreen had the highest sunburn likelihood (62.4%). Also, the group with lowest likelihood of sunburn did not use sunscreen, but engaged in the other protective behaviors (24.3% sunburned). In addition, among 12,566 non–sun-sensitive individuals, those engaged in all 4 protective behaviors had the lowest sunburn (6.6%). The highest likelihood of sunburn was among those who used only sunscreen (26.2%). “The most surprising and counterintuitive finding was that regular sunscreen use, in the absence of other protective behaviors, was associated with the highest likelihood of sunburn.” according to Kasey Morris, who led the study.
Finally, a meta-analysis of the best research, involving 313,000 subjects found that neither melanoma nor non-melanoma skin cancer was associated with sunscreen use. And, another study indicated that in the last three decades, melanoma incidence has increased by 400% and sunscreen use has also increased by 400%. Isn’t it time that we stopped using this toxic, chemical soup?

Think carefully about this information when you next see a sunscreen ad. Enjoy the sun safely (without burning).
Happy sunning
[1] Calafat, A. Concentrations of the Sunscreen Agent, Benzophenone-3, in Residents of the United States: National Health and Nutrition Examination Survey 2003–2004. (Available at http://dx.doi.org/).
[2] Environmental Working Group: Americans Carry Body Burden of Toxic Sunscreen Chemical. 25, 2008. (Available at http://www.ewg.org/node/26212).
[3] Hayden CG, Roberts MS, Benson HA. Systemic absorption of sunscreen after topical application. Lancet 1997:350:863-64.
[4] Gonzalez H, Farbrot A, Larkö A-M. Wennberg A. Percutaneous absorption of the sunscreen benzophenone-3 after repeated whole-body applications, with and without ultraviolet irradiation. British J Dermatol 2016;154:137-140.
[5] Krause M, Klit A, Blomberg Jensen M, Søeborg T, Frederiksen H, Schlumpf M, Lichtensteiger W, Skakkebaek NE, Drzewiecki KT. Sunscreens: Are they beneficial for health? An overview of endocrine disrupting properties of UV-filters. Int. J. Androl. 35, 424436 (2012).
[6] Yang Deng, Asiri Ediriwickrema, Fan Yang, Julia Lewis, Michael Girardi and W. Mark Saltzman. A sunblock based on bioadhesive nanoparticles. Nature materials: published online: 28 September 2015.
[7] Mary S. Wolff, Stephanie M. Engel, Gertrud S. Berkowitz, Xiaoyun Ye, Manori J. Silva, Chenbo Zhu, James Wetmur, and Antonia M. Calafat. Prenatal Phenol and Phthalate Exposures and Birth Outcomes. National Institutes of Health USA Department of Health and Human Services.(available at http://dx.doi.org/)
[8] Lau C, Rogers JM. 2004. Embryonic and fetal programming of physiological disorders in adulthood. Birth Defects Res C Embryo Today 2004;72:300-12.
[9] Bryden AM, Moseley H, Ibbotson SH, Chowdhury MM, Beck MH, Bourke J, English J, Farr P, Foulds IS, et al. Photopatch testing of 1155 patients: results of the U.K. multicentre photopatch group. B J Dermatol 2006;155:737-47.
[10] Rodriguez E, Valbuena MC, Rey M, Porras de Quintana L. 2006. Causal agents of photoallergic contact dermatitis diagnosed in the national institute of dermatology of Colombia. Photodermatol Photoimmunol Photomed 2006;22:189-92.
[11] Hanson KM, Gratton E, Bardeen CJ. Sunscreen enhancement of UV-induced reactive oxygen species in the skin. Free Radic Biol Med. 2006 Oct 15;41(8):1205-12.
[12] Bastien N, Millau JF, Rouabhia M, Davies RJ, Drouin R. The sunscreen agent 2-phenylbenzimidazole-5-sulfonic acid photosensitizes the formation of oxidized guanines in cellulo after UV-A or UV-B exposure. J Invest Dermatol. 2010 Oct;130(10):2463-7
[13] Gulston M, Knowland J. Illumination of human keratinocytes in the presence of the sunscreen ingredient Padimate-O and through an SPF-15 sunscreen reduces direct photodamage to DNA but increases strand breaks. Mutat Res. 1999 Jul 21;444(1):49-60.
[14] Environmental Working Group: Americans Carry Body Burden of Toxic Sunscreen Chemical. 25, 2008. (Available at http://www.ewg.org/node/26212).
[15] Hanson KM, Gratton E, Bardeen CJ. Sunscreen enhancement of UV-induced reactive oxygen species in the skin. Free Radic Biol Med. 2006 Oct 15;41(8):1205-12.
[16] C. A. Downs , Esti Kramarsky-Winter, Roee Segal, John Fauth, Sean Knutson, Omri Bronstein, Frederic R. Ciner, Rina Jeger, Yona Lichtenfeld et al. Toxicopathological Effects of the Sunscreen UV Filter, Oxybenzone (Benzophenone-3), on Coral Planulae and Cultured Primary Cells and Its Environmental Contamination in Hawaii and the US Virgin Islands. Archives of Environmental Contamination and Toxicology Oct 20 2015.
[17] Kasey L. Morris, PhD; Frank M. Perna, EdD, PhD. Decision Tree Model vs Traditional Measures to Identify Patterns of Sun-Protective Behaviors and Sun Sensitivity Associated With Sunburn. JAMA Dermatol. Published online June 27, 2018.
Sunbeds can be healthful devices. By Marc Sorenson, EdD.

Sunbeds, also known as tanning beds, have many healthful properties. They produce vitamin D, strengthen bone and reduce the risk of major cancers. Yet, sunbeds are much maligned as being a major cause of melanoma. Thus, teens in many areas have been banned from using them by misguided legislation. In addition, tanning- salon owners must live in fear of government overreach that could put them out of business.
But new research shows that the attack on sunbeds is misguided.
Because of this uproar, a group of scientists (some dermatologists), led by Dr. Jörg Reichrath, did a thorough research review. Furthermore, they published their findings in the scientific journal Anticancer Research, which presented truth about melanoma and sunbeds. This information is most noteworthy since it is contrary to the prevailing papers that emanate from the Powers of Darkness. The Powers of Darkness are those who love to attack both sun exposure and sunbeds.
Especially relevant points regarding sunbeds and melanoma risk, from Anticancer Research:
- First of all, Reichrath and colleagues performed a systematic literature search. This research was undertaken to identify and evaluate research that investigated relationship of solarium use (sunbed use) and melanoma risk. And as a result, they stated the following: “We found no studies that demonstrate a causal relationship between moderate solarium use and melanoma risk.” In addition, they indicated that the quality of the observational studies was low and that bias may have existed.
- Another interesting finding was that although moderate sunbed use had no effect on melanoma, something else did affect melanoma. An unhealthy lifestyle involving extensive sunbathing, alcohol and smoking associated to a 20% increase in the disease. Also, the researchers mention that individuals with unhealthful lifestyles use tanning salons more often.
At this time, I must make a point. Those who are regularly in the sun have stronger bones and less cancer than sun avoiders. So I’m not sure what “extensive” sunbathing entailed. And, another point is this: As time spent in the sun has decreased profoundly in both Europe and the U.S., melanoma has increased exponentially. Read my book, Embrace the Sun, to see the discussion on this topic.
Could sunbeds actually decrease the risk of melanoma?
Another salient finding of the research review: A study from Europe showed that sunbed use was associated with a 30% reduced risk for developing melanoma. Reichrath and colleagues made this comment on that study: “Those findings indicate that solarium [sunbed] use may even have a protective effect.”
Sunbeds: beyond melanoma. Here are a few truths about sunbeds that are seldom discussed:
The transcendent sunbed study showed that during 20-years, women who used them reduced all-cause mortality by 23%. So let’s suppose that that there were some health problems with using sunbeds. That negative possibility pales in comparison to the remarkably reduced risk of death, does it not? And, I am not stating that there were negatives for sunbed use in this research.
What are some of the reasons that sunbed use is associated with a lower risk of all cause death?
Another investigation showed that sunbeds were associated with a reduced the risk of breast cancer.
In addition, research showed that sunbeds were associated with 90% higher vitamin D levels and significantly stronger bones.
Also, they are useful in treating psoriasis and other skin disorders.
Sunbeds are also useful in treating pain and in improving mood.
Finally, these devices have been shown to associate with lower clot risk.
The takeaway from all of these studies is that there is no credible research that melanoma is increased by using sunbeds. And, sunbeds have remarkably healthful effects. When receiving sun exposure or using sunbeds, be sure not to burn.
Happy sunning!
For more information, read the book, Embrace the Sun.
Saving the children by Marc Sorenson, EdD.

Saving the children is a multi-part discussion that emphasizes the critical need for sun exposure in children because of sun deprivation. In the last blog on the subject, we first of all talked about saving the children from myopia (nearsightedness). And this blog will discuss several additional aspects of childhood health that are positively related to sunlight.
Why are we depriving our children of sunlight? Because $ are involved. So, we must not fail to be about the business of saving the children from the Powers of Darkness.
Saving the children from melanoma. With sunlight!

First of all, much noise is made about removing children from sun exposure to protect them from future melanoma. Consequently, we “protect” them from sunlight by keeping them indoors and dutifully slathering them with sunscreen. Furthermore, our children are taught to fear the sun. That is strange, since research shows that children who engage in outdoor activities are less likely to develop melanoma. In that research, outdoor exercise such as soccer and gardening were mentioned as the most noteworthy activities to protect against melanoma.
Saving the children from asthma. With sunlight!
Asthma, an inflammation of the air passages, has become a scourge of both children and adults. And according to the Asthma and Allergy Foundation, each day 40,000 people miss school or work due to asthma. In addition, 30,000 people have an attack daily, and 5,000 people visit the emergency room.[1] Especially relevant is the fact that the disease is increasing most rapidly among black children. Dark skins need more sunshine to produce vitamin D, which may make these children more susceptible. So what does the research say about sunshine and asthma in children? The most important study was probably one from Spain. It showed that children exposed to the most sunlight had much lower risks of asthma than those who were least-exposed. Thus, each with each hour of added sun exposure per day predicted a decreased risk of the disease.[2]
Saving the children from HIV infection (AIDS)
AIDS is a fearful disease, and it is most noteworthy that the children, the most vulnerable among us are victims. Saving the children from AIDS should be a priority, no?
Sunlight exposure leads to the production of vitamin D, and vitamin D may have a profound influence on the development of AIDS. Thus, HIV-positive pregnant women with lowest vitamin D levels had 50% greater risk of transmission of HIV to their children. Also, there was a two-fold increase of HIV transmission by breast feeding. In addition, there was also a 61% increased death risk among children born to women with low Vitamin D levels.[3] Therefore, sunlight is key to saving the children from this horrible disease.
In conclusion, melanoma, asthma and
AIDS are diseases our children should never need to suffer. Furthermore, regular,
non-burning sun exposure should be a part of the daily lives of children
whenever possible.
Learn more my visiting http://sunlightinstitute.org/ And read
the new book, Embrace
the Sun.
[1] Asthma and Allergy Foundation of America: Asthma Facts and Figures. http://www.aafa.org/display.cfm?id=8&sub=42
[2] Arnedo-Pena A, et al. Sunny hours and variations in the prevalence of asthma in schoolchildren according to the International Study of Asthma and Allergies (ISAAC) Phase III in Spain. Int J Biometeorol 2011;55:423-434.
[3] Mehta S, Hunter DJ, Mugusi FM, Spiegelman D, Manji KP, Giovannucci EL, Hertzmark E, Msamanga GI, Fawzi WW: Perinatal Outcomes, Including Mother-to-Child Transmission of HIV, and Child Mortality and Their Association with Maternal Vitamin D Status in Tanzania. J Infect Dis 2009;200:1022-30.
Sunscreens are not toothpaste. By Marc Sorenson, EdD.
Sunscreens, in Australia and New Zealand, are being touted as absolutely indispensable to prevent of skin cancer. And, this has been the mantra for decades. So, experts from the two countries convened to obtain opinions and produce a statement regarding use of sunscreens.[1] Much as I expected, they concluded people should apply sunscreen daily when the UV index reaches 3. And for much of Australia, that means every day.
Thus, as a result of this declaration, a major Australian newspaper weighed in. They stated “Make it like brushing your teeth:”[2] https://www.brisbanetimes.com.au/national/queensland/make-it-like-brushing-your-teeth-experts-urge-daily-sunscreen-use-20190124-p50thn.html. Rather convenient for those who produce sunscreens, no? If this advice is taken to heart by the people, sunscreen manufacturers and their stockholders will make a fortune. However, I guarantee that the people will suffer.
Increasing use of sunscreens and skin cancer through Slip, Slop, Slap.
It is especially relevant that Australians have been using a campaign called Slip, Slop Slap for decades. The campaign pushes everyone to avoid the sun and use sunscreens. And, according to Cancer Council Australia (the biggest manufacturer of sunscreens in Australia and New Zealand), it is remarkably effective.[3] Thus they state, “The Slip Slop Slap slogan has become institutionalized as the core message of Cancer Council’s SunSmart program.” And, they say the campaign has played a key role in the shift in sun protection behavior over two decades. (The program has actually been used for about three decades.) Because of this program, Australians and New Zealanders use more sunscreens than any other countries on earth, and the use of sunscreens continues to rise. But as a result of this sunscreen use, has skin cancer diminished?
How are the sunscreens promotions working for the health of the Australian people?
First of all, this is not new information; it has been known for decades. Dr. David Myers, a dermatologist, thus wrote an article that contains this statement: “The Australian experience provides the first clue. The rise in melanoma has been exceptionally high in Queensland where the medical establishment has long and vigorously promoted the use of sunscreens. Queensland now has more incidence of melanoma per capita than any other place. Worldwide, the greatest rise in melanoma has been experienced in countries where chemical sunscreen have been heavily promoted.”[4] [5]
And Dr. Cedric Garland echoed that statement, saying that Queensland, Australia has vigorously promoted sunscreens for decades. And he also says that Queensland now has one of highest rates of melanoma in the world.[6] [In addition, the rate of vitamin D deficiency there is becoming critical.[7]]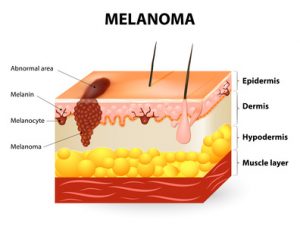
Does the Australian sunscreen declaration run up against some inconvenient truths?
So, we have a declaration suggesting that we should use sunscreens regularly like toothpaste. The declaration obviously implies that sunscreens are protective against skin cancer in Australia. It is hard to explain that conclusion. Why? Because the long-term, exponentially increasing use of sunscreens has been accompanied by an exponential increase in skin-cancer incidence. Therefore, if sunscreens are protective against skin cancer, there is something very wrong with that history.
And, unfortunately, skin cancer also continues to rise. Hence, Australia and New Zealand have more skin cancer than any other country on earth.[8] [9] It seems like this emphasis on sunscreens has not worked. So we come up with this new formula. More use of sunscreens over the years=higher risk of skin cancer. And, it appears that they want to continue using this formula!
But of course, the “experts’” solution is to ignore the historical facts and promote the use of more sunscreens. It seems like these people have not heard the old saying: “Doing the same thing over and over, and expecting different results, is the definition of insanity.” So, shall we be as dedicated to sun screen use as we are to brushing our teeth? Shall we make the use of sunscreens like the use of toothpaste? I have a secret for the people who promote sunscreens: Sunscreens are nothing like toothpaste, because toothpaste may actually accomplish something.
Should North America adopt this Australian recommendation of daily use?
First of all, according to the main research used for this recommendation, the answer is a big NO. One of the Australian researchers, Adele Green, made this statement: “Although the results are directly relevant to people who live in sunny climates like Australia’s and who receive relatively high levels of ambient sun exposure as a matter of course, they also have implications for white people living in temperate climates in North America and Europe who are at increased risk of melanoma because of increased solar UV exposure caused by the predilection for holidays in sunny places.” So they are saying sunscreens are NOT required unless on sunny holidays or if you have a sunburning risk. This doesn’t sound like a recommendation for daily use in North America. And, as European research demonstrated, it is certainly not a useful recommendation for Europe. (See the heading below regarding Europe.)
North American research on sunscreens and skin cancer
Another piece of research[10] looked at sunscreen use in North America and stated the following; “In contrast, for people who live at higher latitudes where UV radiation is weaker and less constant, regular sunscreen use may provide less protection against skin cancer, or even increase the risk of carcinogenesis.” The paper goes on to say “While the current evidence suggests no increased risk of skin cancer related to sunscreen, this systematic review and meta-analysis does not confirm the expected protective benefits of sunscreen use against skin cancer in the general population.” So again, this is NOT a recommendation for daily use of sunscreens. And, it indicates they may do more harm than good.
Are sunscreens counterproductive?
So it appears, based on what has been written so far, that sunscreens may be worthless at best and dangerous at worst. Another recent scientific study on sunscreens and sunburns corroborates this conclusion.[11] The authors of this study expected an outcome opposite of the facts. The goal was to discover which sun-protection behavior, including use of sunscreens, was most effective in preventing sunburn. Hence, they designed a cross-sectional investigation using a nationally representative sample of about 32,000 U.S. adults. And, those conducting the research interviewed each participant in person. This is especially relevant when attempting to achieve the most accurate results possible. We can conclude, therefore, that their findings regarding sunscreen use and other “sun-protective” behaviors have validity. Those other sun-protective behaviors included seeking shade, wearing a hat or visor, and wearing long sleeves and pants.
Sunscreens and sunburn results
In addition, the subjects were identified as sun-sensitive individuals or non-sun-sensitive individuals. Fifty-four percent of the subjects were women, and 15,992 of all individuals were considered sun-sensitive. It is most noteworthy that among sun-sensitive individuals, those who used only sunscreens had the highest sunburn likelihood (62.4%). The group with lowest likelihood of sunburn did not use sunscreens but engaged in the other protective behaviors (24.3% sunburned). In addition, among 12,566 non–sun-sensitive individuals, those engaged in all 4 protective behaviors had the lowest sunburn risk (6.6%). And in that group, the highest likelihood of sunburn was among those who only used sunscreen (26.2%). According to Dr. Kasey Morris, who led the study, “the most surprising and counterintuitive finding was that regular sunscreen use, in the absence of other protective behaviors, was associated with the highest likelihood of sunburn.”[12]
What do dermatologists believe about sunscreen and sunburn?
I have never heard of a dermatologist who didn’t believe that sunburns led to skin cancer. And I have only seldom heard of dermatologists who didn’t believe that sunscreens prevented sunburns. This research turns their beliefs about sunscreen upside down.
I have also been told that the reason sunburn occurs with the use of sunscreens, is this: People get a false sense of safety while using sunscreens. Consequently, they stay out in the sun for excessively long times. To me that doesn’t matter. If sunscreen leads to sunburn, which leads to skin cancer, who cares what the reason is? When using a poison, does it matter what the mechanism of poisoning is if the patient dies? Why use a product that causes harm?
Other sunburn results with sunscreens
Finally, it has been known since 2014 that sunscreen use associates closely with sunburning.[13] Therefore, sunscreens are not good products. We should protect ourselves from overexposure to the sun the way God (or Mother Nature, if you prefer) intended it. 1. Cover up when you start to redden, 2. seek shade or 3. go indoors. And remember that good health depends on obtaining regular, non-burning sun exposure.
Another reason to avoid sunscreens
The state of Hawaii has now banned this noxious product. This is because of the destruction of the coral reefs caused by certain ingredients in this chemical soup. In addition, we know that since the first sunscreens were introduced, the risk of melanoma skin cancer has increased. How much? By about 3,000%. And yes, you read that correctly. If you have other questions, read the sunscreen section of my new book, Embrace the Sun,.https://www.amazon.com/Embrace-Sun-Marc-B-Sorenson/dp/069207600X
Use of sunscreens in Europe
Another important study demonstrates that sunscreens do not help prevent melanoma.[14] The researchers’ goal was to determine the efficacy of sunscreens in preventing melanoma. Hence, they compared melanoma rates with sales in 24 countries in Europe, during the period of 1997-1999 to 2008 and 2012. They found that higher income people had significantly higher melanoma incidence. And, increased sunscreen use had not prevented higher income populations from being at higher risk of melanoma. Consequently, we see this equation again: Higher sunscreen use=higher melanoma risk! One of the reasons for this little-known relationship is most noteworthy. Up to 99% of vitamin D production is stopped by sunscreen.[15] Therefore, many of the health benefits of sun are voided.
Summary on sunscreens and sunlight:
The best sunscreen, when you need it, is covering your skin with clothing, or going indoors. Stay away from the noxious chemicals. Be sure to obtain some non-burning sunlight whenever possible.
Happy sunning!
[1] David C. Whiteman, Rachel E. Neale, Joanne Aitken, Louisa Gordon, Adele C. Green, Monika Janda, Catherine M. Olsen, H. Peter Soyer, on behalf of the Sunscreen Summit Policy Group. When to apply sunscreen: a consensus statement for Australia and New Zealand. When to apply sunscreen: a consensus statement for Australia and New Zealand.
[2] https://www.theage.com.au/national/queensland/make-it-like-brushing-your-teeth-experts-urge-daily-sunscreen-use-20190124-p50thn.html
[3] https://www.cancer.org.au/preventing-cancer/sun-protection/campaigns-and-events/slip-slop-slap-seek-slide.html
[4] http://www.yourhealthbase.com/sunscreens.htm
[5] Garland, Cedric F., et al. Could sunscreens increase melanoma risk? American Journal of Public Health, Vol. 82, No. 4, April 1992, pp. 614-15
[6] Garland CF, Garland FC, Gorham ED. Could sunscreens increase melanoma risk? American Journal of Public Health, Vol. 82, No. 4, il 1992, pp. 614-15.
[7] Van der Mei IA, Ponsonby AL, Engelsen O, Pasco JA, McGrath JJ, Eyles DW, Blizzard L, Dwyer T, Lucas R, Jones G. A high vitamin D insufficiency across Australian populations and latitude. Environmental Health Perspect 2007;115:1132-39.
[8] https://www.rightdiagnosis.com/news/skin_cancer_rate_increasing_in_australia.htm.
[9] https://www.sciencelearn.org.nz/resources/1329-nz-skin-cancer-statistics
[10] Elizabet saes da SILVA, Roberto TAVARES, Felipe da silva PAULITSCH, Linjie ZHANG. Use of sunscreen and risk of melanoma and non-melanoma skin cancer: a systematic review and meta-analysis. Eur J Dermatol 2018; 28(2): 186-201.
[11] Kasey L. Morris, PhD; Frank M. Perna, EdD, PhD. Decision Tree Model vs Traditional Measures to Identify Patterns of Sun-Protective Behaviors and Sun Sensitivity Associated With Sunburn. JAMA Dermatol. Published online June 27, 2018
[12] https://www.reuters.com/article/us-health-sunburns/sun-sensitive-people-need-more-than-sunscreen-to-avoid-sunburn-idUSKBN1K02RB
[13] https://www.webmd.com/beauty/news/20110714/sunscreen-users-more-likely-burn#4
[14] Williams SN, Dienes KA. Sunscreen Sales, Socio-Economic Factors, and Melanoma Incidence in Northern Europe: A Population-Based Ecological Study. SAGE Open October-December 2014: 1–6.
[15] Matsuoka LY, Ide L, Wortsman J, MacLaughlin JA, Holick MF. Sunscreens suppress cutaneous vitamin D3 synthesis. Journal of Clinical Endocrinology & Metabolism 1987; 64:1165-68.
 Sunlight improves public health. By Marc Sorenson, EdD.
Sunlight improves public health. By Marc Sorenson, EdD.
An excellent new paper by Dr. Hoel and Dr. de Gruijl is titled “Sun Exposure Public Health Directives.” It decries the vilification of sunlight and suggests people return to its healthful rays.[1] https://www.mdpi.com/1660-4601/15/12/2794/htm
So is dermatology awakening to the truth about sunlight?
And one of the authors, Dr. de Gruijl, works at a dermatology department in the Netherlands. He is also a photobiologist and melanoma skin cancer research specialist. It seems like the dermatology world is returning to common sense, since other dermatologists have lately suggested more sunlight exposure. And well they should suggest more sunlight! Sunlight can save millions of lives, yet much of the population is dying in the dark due to misinformation. Many dermatologists consider sunlight exposure to be a killer, and thus frighten their patients away from sun exposure. Why? Because they are fearful of skin damage from sunlight, something they need not fear if they advise their patients properly.
Sunlight and skin cancer: the truth
One of my pet peeves is the statement that “sunlight causes cancer.” First of all, there are about 18 major cancers that are reduced by sunlight. And in addition, there are also myriad non-cancer maladies that are reduced or eliminated by safe sun exposure. These disorders run the gamut from arthritis and heart disease to psoriasis, erectile dysfunction and osteoporosis.[2] Secondly, not even skin cancer is caused by sun exposure unless people burn themselves. Therefore, it is a lack of both caution and common sense that leads to skin damage. The authors state that the public has been taught that health benefits of sun exposure are limited to bone health. That is another egregious error (italics mine).
The aforementioned paper reads almost like a synopsis of Embrace the Sun, the book by Marc Sorenson and William Grant,
Here are the major points on sunlight that make the research in the paper so compelling:
- There is a public health message that “overexposure” to the sun causes skin cancer. Nevertheless, those who promote this message do not define overexposure. Therefore, due to the lack of a definition, the public is led to believe that sun exposure is an enemy. In addition, the public is not educated regarding the detriments of “sun avoidance,” or should we say “underexposure.” Due to this omission, the public is exposed to disability, destruction and death (italics mine).
Sunlight deprivation: the staggering cost to human health
Consequently, in Embrace the Sun, we calculated the number of deaths due to diseases associated with high sunlight exposure. And, we then calculated the number of deaths due to diseases associated with sunlight deprivation. As a result, we determined that approximately 1,684,677 yearly deaths are caused by diseases associated with sunlight deprivation. Also, there were about 5125 deaths from diseases associated with high sunlight exposure, producing a ratio of approximately 328.7:1. This is most noteworthy! 328 deaths were associated with diseases of sun deprivation for each death associated with diseases of sun exposure. So, what do you think?
So, is sunlight avoidance risk free?
- Furthermore, the paper states that people believe sun avoidance is risk free. That is a colossal error as previously stated,
- Another mistake is to believe vitamin D supplements are an adequate substitute for sunlight. That is simply not so. Sun exposure causes the production of serotonin, nitric oxide, endorphin, brain-derived neurotropic factor (BDNF), dopamine and urocanic acid. All of these substances are vital for human health and wellbeing.
- Another important point stated by the authors is as follows: “This public health message is potentially causing significant harm to public health and should be changed immediately.” And, based on the analysis from Embrace the Sun, mentioned above, that should be an easy conclusion.
Is there an inverse association between sunlight and melanoma?
- The authors also state that melanoma risk is reduced by non-burning sun exposure. And only severe sunburns increase risk. In addition, they mention that melanoma in the U.S. has steadily increased at an annual rate of 3–4%. There was 1 case per 100,000 in 1935, when accurate records were established. Yet, there were 25.8 cases per 100,000 in 2015. [That is about a 2,600% increase!]
Our analysis of melanoma in Embrace the Sun was almost identical. It showed a 3,000% increase in melanoma risk accompanied by a 90% decrease in sunlight exposure from 1935 to 2015. And, Sunscreen use also increased dramatically during that period, meaning that more sunscreen use is associated with greater melanoma risk.
And should we use sunscreens to reduce sunlight damage?
The answer to that question is “of course not.”
I was surprised that nothing was said about sunscreens, while I was considering the authors’ comment on severe sunburns, Why? Because recent research has shown that persons who use sunscreens have 4-6 times greater risk of sunburn.[3] In addition, the same research showed that the greatest protection against burning was to seek shade or cover up. Imagine that! Also, a recent meta-analysis showed that sunscreen use made absolutely no difference in the risk of skin cancer.[4].
- The authors also make it clear that the common assertion—that tanned skin affords insignificant protection against sunburn—is not correct.
- In conclusion, the commentary made this statement: “All persons in the world regardless of skin color or latitude of residence, other than those with extraordinary sensitivity to sunlight, should get enough sun exposure to maintain a serum 25(OH)D level well over 20 ng/mL (desirably at 30–60 ng/mL) while taking care to avoid sunburn.
I agree and would like to reiterate that vitamin D supplements are not an adequate substitute for sunlight. Consequently, these measurements should be used only among those who do not take supplements. That is, if we expect to really measure sunlight exposure.
Embrace the Sun is available here. 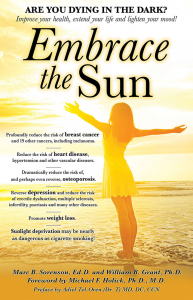
Happy sunning!
[1] Hoel D, de Gruijl, F. Sun Exposure Public Health Directives. Int. J. Environ. Res. Public Health 2018;15:2794
[2] Sorenson, Marc, Grant, WB. Embrace the Sun. Sorenson, Publisher 2018. Available at Amazon.
[3] Kasey L. Morris, PhD; Frank M. Perna, EdD, PhD. Decision Tree Model vs Traditional Measures to Identify Patterns of Sun-Protective Behaviors and Sun Sensitivity Associated With Sunburn. JAMA Dermatol. Published online June 27, 2018.
[4] Elizabet saes da SILVA, Roberto TAVARES, Felipe da silva PAULITSCH, Linjie ZHANG. Eur J Dermatol 2018; 28(2): 186-201.
Melanoma risk between persons with high and low vitamin D levels
Melanoma Risk By Marc Sorenson, EdD, Sunlight Institute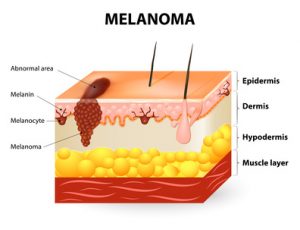
The risk directly associates with low levels of vitamin D. That is the conclusion of recent study published in the European Journal of Cancer.[1] The investigators measured the blood vitamin D levels of 137 subjects who had been diagnosed with melanoma. They collected the blood samples at the time of diagnosis of the disease. Another group of 99 healthy subjects served as the control group. The investigators collected the samples of the control group between October and April. The scientists then compared the blood collections of the melanoma group with those of the control group. They then determined whether vitamin D levels had an association with melanoma risk.
The study produced convincing results regarding vitamin D and melanoma risk.
The results were as follows:
- The controls (no melanoma) had vitamin D levels 50% higher than the melanoma group (27.8 ng/ml vs. 18 ng/ml).
- 66.2% of the melanoma group had vitamin D “deficiency,” compared to only 15.2% of the health controls. The scientists defined vitamin D deficiency as being equal to or less than 20 ng/ml. So, the melanoma group had more than four-times the risk of deficiency.
- The scientists defined vitamin D “sufficiency” as being equal to or greater than 30 ng/ml. They found that only 7.4% of melanoma patients were sufficient, compared to 37.4% of healthy controls. Hence, the melanoma group had about one-fifth the likelihood of having sufficient D levels.
More scientific analysis on vitamin D measurements vs. melanoma risk
The scientists then adjusted the data for possible confounding factors such as age, sex and body mass. Then, they performed an analysis that showed the following:
- First of all, the science demonstrated a significant inverse association with vitamin D sufficiency versus deficiency. Those who had sufficient levels had only 4% of the melanoma risk when compared to those who were deficient! Hence, this demonstrates that those with the lowest vitamin D levels (after adjusting for confounding factors) had 25-times the melanoma risk!
- And, vitamin D insufficiency vs. deficiency was significantly inversely associated with melanoma. Those who were insufficient had a definite advantage over those who were deficient. They had only 13% of the melanoma risk.
Now, this is the most important point about melanoma risk:
In addition, this research proves conclusively that sun deprivation is a major cause of melanoma. I say this because about 90% of serum vitamin D is produced by sun exposure to the skin.[2] So, the aforementioned research is really research on sun exposure. It shows that regular sun exposure leads to a profound reduction in melanoma risk. Therefore, Vitamin D levels are surrogate measurements for sun exposure in nearly every case.
Could sunlight increase health through photoproducts beyond vitamin D?
In conclusion: My new book, Embrace the Sun (coauthored by Dr. William Grant), notes that sun exposure provides more than vitamin D. It also provides other photoproducts such as nitric oxide, serotonin, endorphin, and brain-derived neurotropic factor (BDNF). All of these photoproducts are vital to human health. Could these photoproducts have a positive and protective effect against melanoma risk beyond vitamin D? And, vitamin D produced by sunlight may be superior to that given in pill form.
Finally, this research gives us one more reason to embrace the sun safely without burning. And who would have thought that safe sunlight could be one of the best prophylactics against melanoma risk?
Happy sunning!
The book is available at Amazon: https://www.amazon.com/Embrace-Sun-Marc-B-Sorenson/dp/069207600X/ref=sr_1_1?ie=UTF8&qid=1533923845&sr=8-1&keywords=embrace+the+sun+sorenson
1] Cattaruzza MS, Pisani D, Fidanza L, Gandini S, Marmo G, Narcisi A, Bartolazzi A, Carlesimo M. 25-Hydroxyvitamin D serum levels and melanoma risk: a case-control study and evidence synthesis of clinical epidemiological studies. Eur J Cancer Prev. 2018 Feb 12. [Epub ahead of print]
[2] Reichrath J. The challenge resulting from positive and negative effects of sun: how much solar UV exposure is appropriate to balance between risks of vitamin D deficiency and skin cancer? Prog Biophys Mol Biol 2006;92(1):9-16
What do you know about melanoma?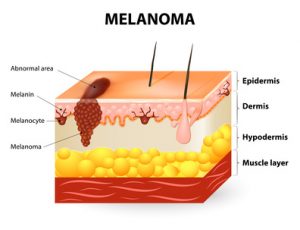
May is Melanoma Awareness Month, Therefore, we will discuss some truths to be aware of:
- First of all, seventy-five percent of these cancers occur on areas of the body that are seldom or never exposed to sunlight.[1] For example, research has shown that melanomas in women occur primarily on the upper legs, and in men more frequently on the back—areas of little sun exposure.
- Most noteworthy, in the U.S., sun exposure has decreased by about 90% since 1935. In the same time, melanoma incidence has increased by 3,000%! [2] [3] [4]
Dr. Diane Godar furnishes this exceptionally important melanoma information:[5]
- The same as in the US, while sun exposure in Europe has profoundly decreased, there has been a spectacular increase in the disease.
- Men who work outdoors have about half the risk as men who work indoors. Hence, sun exposure could not be the cause.
- in addition, outdoor workers, while receiving 3-9 times the sun exposure as indoor workers, have had no increase in melanoma since before 1940, whereas the incidence in indoor workers has increased steadily and exponentially.
- Especially relevant is that sunscreen invention, along with its steadily increasing use, has not reduced the risk of melanoma. Rather, the disease has increased as sunscreen use has increased.
- Increasing melanoma incidence significantly correlates with decreasing personal annual sunlight exposure.
- Also, outdoor workers get many sunburns but still have dramatically lower risk of contracting the disease.
So, since melanoma increases as sun exposure decreases, should we continue to blame the sun?
Here are more facts you should know about the causes of melanoma:
- First of all, people in the highest quintile (fifth) of alcohol consumption have a 65% increase in risk.[6]
- Weekly meat consumption increases the risk of melanoma by 84% and daily fruit consumption reduces the risk by nearly 50%.[7]
- Furthermore, those with the highest levels of blood PCBs have 7-times the risk compared to those with the lowest levels.[8]
- Recent use of Viagra is associated with an 84% increase in risk, and long-term use of the drug is associated with a 92% risk increase.[9]
- Finally, there is a positive association between melanoma and obesity.[10]
Furthermore, Dr. Adele Green found that the strongest risk factor for both limb and trunk melanoma was moles. The presence of more than 10 moles on the arm predicted a 42-times increased risk.[11]
Therefore, please stop blaming the sun. Safely embrace the non-burning sun and reduce your risk of melanoma.
References:
[1] Crombie IK. Distribution of malignant melanoma on the body surface.Br J Cancer. 1981 Jun;43(6):842-9.
[2] Melanoma International Foundation, 2007 Facts about melanoma. Sources: National Cancer Institute 2007 SEER Database, American Cancer Society’s 2007 Facts and Figures, The Skin Cancer Foundation, The American Academy of Dermatology.
[3] Ian D. Wyatt and Daniel E. Hecker. Occupational changes in the 20th century. Monthly Labor Review, 2006 pp 35-57: Office of Occupational Statistics and Employment Projections, Bureau of Labor Statistics.
[4] US Congress, Office of Technology Assessment, Catching Our Breath: Next Steps for Reducing Urban Ozone, OTA-O-412 (Washington, DC: US Government Printing Office, July 1989).
[5] Stephen J Merrill, Samira Ashrafi, Madhan Subramanian & Dianne E Godar. Exponentially increasing incidences of cutaneous malignant melanoma in Europe correlate with low personal annual UV doses and suggests 2 major risk Factors. Dermato-endocrinology 2015;7:1
[6] Millen AE, Tucker MA, Hartge P, Halpern A, Elder DE, Guerry D 4th, Holly EA, Sagebiel RW, Potischman N. Diet and melanoma in a case-control study. Cancer Epidemiol Biomarkers Prev. 2004 Jun;13(6):1042-51.
[7] Gould Rothberg BE, Bulloch KJ, Fine JA, Barnhill RL, Berwick M. Red meat and fruit intake is prognostic among patients with localized cutaneous melanomas more than 1 mm thick. Cancer Epidemiol. 2014 Oct;38(5):599-607.
[8] Gallagher RP, Macarthur AC, Lee TK, Weber JP, Leblanc A, Mark Elwood J, Borugian M, Abanto Z, Spinelli JJ. Plasma levels of polychlorinated biphenyls and risk of cutaneous malignant melanoma: a preliminary study. Int J Cancer. 2011 15;128(8):1872-80.
[9] Li WQ, Qureshi AA, Robinson K, Han J. Sildenafil use and increased risk of incident melanoma in US men: a prospective cohort study. JAMA Intern Med. 2014 Jun;174(6):964-70C
[10] Karimi K, Lindgren TH, Koch CA, Brodell RT. Obesity as a risk factor for malignant melanoma and non-melanoma skin cancer. Rev Endocr Metab Disord. 2016 Sep;17(3):389-403.
[11] Green AC, Siskind V. Risk factors for limb melanomas compared with trunk melanomas in Queensland. Melanoma Res. 2012 ;22(1):86-91.
I have written several blogs making this melanoma case: not only is this deadly cancer not caused by sun exposure, but habitual, or regular, sun exposure has a protective effect against the disease. This blog will serve to reinforce and review the reasoning behind those conclusions.
A friend sent me a scientific paper[1] that I had forgotten or missed—a paper by Dr. Veronique Bataille that brought out several supportive points about how sun exposure protects against the disease. Here are a few of the salient ideas from the paper:
- The increase in melanoma is mostly seen for the thin types, which can’t be attributed to sun exposure but to increasing screening over the last 20 years. The fact is, that incidence appears to increase as the number of dermatologists and public health campaigns also increase. But the increase in melanoma is not real. This idea is perfectly plausible; when more dermatologists are available, and the public is driven to them by health campaigns more melanomas are found. Many “first-stage” or thin “thin” melanomas are discovered and counted that would not have been found in previous decades. This causes numbers to be highly inflated compared to the days when there were fewer dermatologists and fewer public health campaigns.
Comment: Another fact was not mentioned in the paper: Stunningly, a worldwide study of melanoma diagnosis and accuracy, published in the American Academy of Dermatology (AAD) showed that most diagnoses were incorrect.[2] Approximately 44 different authors from many different clinics and countries, including the US, contributed to the report. They made an accuracy-in-detection analysis based on the actual number of melanomas that were excised during a period of ten years, compared with the number that really needed to be excised. Many clinics in different countries were involved in assessing the numbers. The AAD research showed that only about 3.5% of diagnoses in non-specialized clinics, and 14.7% in specialized clinics, resulted in actually being melanoma. From this information, it is evident that many melanoma surgeries are bogus and may inflate the incidence of this deadly skin cacner.
What do we take away from this? There may be no real increase in melanoma, only an increase in assessment and excision.
- Low vitamin D levels are common in melanoma patients and have a deleterious effect on their risk and survival.
Comment: Low vitamin D levels are caused by sunlight deprivation; we are told to avoid the sun, but sun avoidance leads to vitamin D deficiency, which further leads to melanoma. If our population regularly enjoyed non-burning sun exposure, vitamin D levels would be much higher and the risk of melanoma much lower. This is corroborated by the fact that people who habitually work outdoors have a far lower risk of the disease. Dr. Cedric Garland and his colleagues showed that those who worked indoors had a 50% greater risk of than those who worked both indoors and outdoors.[3]
- An excess of naevi (moles), not sun exposure, is the strongest risk factor for melanoma, and when comparing the risk created by sunburns and fair skin to the risk created by an excess of moles, the moles create a 15-30 times higher risk.
Comment: Some very important research by Dr. Adele Green found that the strongest risk factor for both limb melanoma and trunk melanoma was the presence of more than 10 moles on the arm, which predicted a 42-times increased risk. [4] This means that public health campaigns should promote mole awareness! Unfortunately, they promote sun avoidance, which increases the risk of melanoma.
- Attempts to decrease melanoma incidence and mortality, by reducing sun exposure, has not been proven to work and may be harmful.
Comment: the statement is obviously true. In the U.S., Sun exposure has decreased by about 90% since 1935. During that same period, melanoma has increased by 3,000%.[5] Data from the Bureau of Labor statistics showed that indoor occupations such as “professional, managerial, clerical, sales, and service workers (except private household service workers) grew from one-quarter to three-quarters of total employment between 1910 and 2000.” The BLS also stated, during the same period, the outdoor occupation of farming declined by 96% from 33% to 1.2% of total employment. The data also show approximately 66% of the decline in the occupation of farmers and 50% of the decline in the occupation of farm laborers occurred after 1935.
Further information, this time from the Environmental Protection Agency (EPA) determined as of 1986, about 5 percent of adult men worked mostly outside, and about 10 percent worked outside part of the time. The proportion of women who worked outside was thought to be even lower.[6] These data demonstrate a dramatic shift from outdoor, sun-exposed activity to indoor, non-sun-exposed activity during the mid-to-late 20th Century. This change, nonetheless, has been accompanied by a 30-times increase in risk since 1935, the MIF-baseline year.
- Photoageing, which is skin ageing due to sunlight exposure, is not greater in melanoma patients than patients who do not have the disease. In fact, patients with the cancer exhibit less photoageing than those who do not have the disease.
Comment: This was a new research for me and it belied the idea that sun exposure caused melanoma. If sun exposure causes skin photoageing, and there is less photoageing on cancer sites, sun exposure cannot possibly be causing melanoma. Enough said.
We need our sunshine, and one of the reasons for that need is to prevent deadly cancers.
[1] Bataille V. Melanoma. Shall we move away from the sun and focus more on embryogenesis, body weight and longevity? Medical Hypotheses 81 (2013) 846–850.
[2] Argenziano G, Cerroni L, Zalaudek I, Staibano S, Hofmann-Wellenhof R, et al. Accuracy in melanoma detection: a 10-year multicenter survey.J Am Acad Dermatol. 2012 Jul;67(1):54-9.
[3] Garland FC, White MR, Garland CF, Shaw E, Gorham ED. Occupational sunlight exposure and melanoma in the U.S. Navy. Arch Environ Health. 1990 Sep-Oct;45(5):261-7.
[4] Green AC, Siskind V. Risk factors for limb melanomas compared with trunk melanomas in Queensland. Melanoma Res. 2012 Feb;22(1):86-91.
[5] Melanoma International Foundation, 2007 Facts about melanoma. Sources: National Cancer Institute 2007 SEER Database, American Cancer Society’s 2007 Facts and Figures, The Skin Cancer Foundation, The American Academy of Dermatology.
[6] US Congress, Office of Technology Assessment, Catching Our Breath: Next Steps for Reducing Urban Ozone, OTA-O-412 (Washington, DC: US Government Printing Office, July 1989).
 Ovarian cancer, like most cancers, is nothing to trifle with. There are 22,280 new cases of ovarian cancer and 14,240 deaths annually in the U.S.[1] Compare that death statistic to melanoma, which has a death rate of only 9,730.[2] (And I might mention that people who are regularly in the sun have a reduced risk of melanoma.) But are there any indications that ovarian cancer is reduced by sun exposure? Yes. The National Cancer Institute’s Cancer Mortality Map also shows that ovarian cancers are much less common in sunnier Southern and Southwestern States than in the North and Northeast,[3] indicating a protective effect of sun exposure.
Ovarian cancer, like most cancers, is nothing to trifle with. There are 22,280 new cases of ovarian cancer and 14,240 deaths annually in the U.S.[1] Compare that death statistic to melanoma, which has a death rate of only 9,730.[2] (And I might mention that people who are regularly in the sun have a reduced risk of melanoma.) But are there any indications that ovarian cancer is reduced by sun exposure? Yes. The National Cancer Institute’s Cancer Mortality Map also shows that ovarian cancers are much less common in sunnier Southern and Southwestern States than in the North and Northeast,[3] indicating a protective effect of sun exposure.
Research has also demonstrated a relationship between high sun exposure and low risk of ovarian cancer. For example, an Australian investigation showed that women in the highest third of sun exposure, over a lifetime, had a 30% reduced risk of all endothelial ovarian cancers, a 53% reduced risk of borderline tumors and 22% reduced risk of invasive tumors.[4] And, in one piece of research using the Nurses’ Health Study ll, sun exposure was associated with a 33% reduced risk of ovarian cancer.[5] Ovarian cancer mortality rates were also found to be strongly inversely correlated with solar UVB doses in an ecological study by Drs. William Grant and Cedrick Garland.[6]
Sun avoidance is one of the most deadly practices ever perpetrated on the public. Women, carefully embrace the sun and reduce your risk of this potentially deadly disease.
[1] Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016 Jan;66(1):7-30.
[2] American Cancer society statistics, 2017.
[3] Grant, W B. Information available at SUNARC.org, and at the National Cancer Institute’s Cancer Mortality Maps and Graphs.
[4] Tran B, Jordan SJ, Lucas R, Webb PM, Neale R; Australian Ovarian Cancer Study Group. Association between ambient ultraviolet radiation and risk of epithelial ovarian cancer. Cancer Prev Res (Phila). 2012 Nov;5(11):1330-6.
[5] Prescott J, Bertrand K, Poole E, Rosner B, Tworoger S. Surrogates of Long-Term Vitamin D Exposure and Ovarian Cancer Risk in Two Prospective Cohort Studies. Cancers 2013, 5, 1577-1600;
[6] Grant WB, Garland CF. The association of solar ultraviolet B (UVB) with reducing risk of cancer: multifactorial ecologic analysis of geographic variation in age-adjusted cancer mortality rates. Anticancer Res. 2006 Jul-Aug;26(4A):2687-99.