By Marc Sorenson, EdD. Sunlight Institute…
This Blog is meant neither to promote the use of tanning beds nor to discourage such use; rather, it is designed to balance the message. Seldom is anything positive said about tanning beds, although there is research that shows many positive benefits; such research is usually ignored because it does not conform to a preconceived notion. We therefore want to present some of that research to demonstrate that there are other opinions that provide some balance to the messages. You, the reader, can then make up your mind based on the research. Knowing the entire truth about any subject is important prior to making up one’s mind regarding that subject.
Sun exposure and tanning have been vilified by many (but not all) dermatologists. Tanning beds have been demonized to an even greater degree and are called “cancer machines” by many in the medical profession and in the popular press. There are movements afoot to make it illegal for those under the age of 18 to even use them, which is woefully misguided and ill-advised. Every beneficial effect of vitamin D that is produced by sun exposure is also produced by the use of high-quality tanning beds, and endorphins and nitric oxide are also produced, just as with the sun. The following is a list and discussion of tanning-bed benefits.
- Many so-called experts have said that tanning beds do not create higher vitamin D levels, but the research belies that falsehood. In a study that compared 50 subjects who used a tanning bed at least once weekly to 106 control subjects who did not use tanning beds, it was shown that tanning-bed users had 90% higher vitamin D levels than non-users, and they also had significantly higher bone-mineral density, indicative of stronger bones.[1] Parathyroid hormone (PTH) levels were also taken and were 18% lower among the tanners. High PTH levels are often associated with weak bones and low vitamin D levels. The researchers compared dark-skinned people with Caucasians and found that tanning-bed sessions increased vitamin D levels almost identically in both ethnic groups.[2]
I am part of an email list of scientists and researchers who are intensely interested in sun research, and who share articles on sun and vitamin D. I received a most interesting email from Rufus Greenbaum, who lives in the UK and who organizes vitamin D symposiums. He recounted how he had met a man who had used tanning beds twice weekly since 1970, and who had just completed a bone densitometer test, known as a DEXA scan. His doctor stated, “You have the strongest bones that I have ever seen.” That news certainly came as no shock. Conventional tanning beds produce large quantities of vitamin D in short periods of time,[3] and vitamin D is absolutely essential for optimal absorption of calcium in the gut.[4] [5] Without calcium absorption, consuming vast quantities of calcium makes little difference to bone strength; much of the calcium will be flushed down the toilet.
- Tanning beds can cure psoriasis and eczema and are often recommended by dermatologists as a way to overcome these diseases. Some common-sense scientists understand that UV light is nearly 100% effective for many dermatologic conditions, and that tanning beds are very convenient sources of UV for patients who cannot otherwise afford the rigorous travel and time commitments necessary to visit the dermatologist.[6] Their investigation involved an arduous search of PubMed and Google Scholar for papers that reported on tanning beds and their salutary effects on different skin diseases.
The searches showed convincingly that tanning beds were a valid use for psoriasis, but also indicated tanning beds could be useful “as a treatment option for atopic dermatitis [eczema], mycosis fungoides, acne, scleroderma, vitiligo, and pruritus, as well as other UV sensitive dermatoses.”
The conclusion they reached was amazing, considering negative reports that are regularly touted by the press. They stated: “Unsupervised sun exposure is a standard recommendation for some patients to obtain phototherapy. Selected use of commercial tanning beds in the treatment of dermatologic conditions may be another useful and effective treatment for those patients with an inability to access office-based or home-based phototherapy.”[Italics mine]
One of the dermatologists who recommends unsupervised sun exposure as stated above is Dr. Julie Moore of Gottlieb Memorial Hospital. She says that sun is one of the best ways to treat psoriasis, so she recommends that her patients “sit out on the deck and give their affected areas a good sun bath.[7]” Hallelujah! Common sense is beginning to penetrate the dermatology profession, as more dermatologists are climbing on the sun bandwagon each year.
- Whereas a daily 400 IU vitamin D supplement does not maintain healthful levels, tanning bed use increases vitamin D levels by 150% in only seven weeks.
- Tanning-bed use reduces chronic pain.[9] [10] In a study by dermatologists, using persons with fibromyalgia symptoms including pain, those who used UV-producing tanning beds experienced a decrease of .44 points on a scale of pain score when compared to those who did not receive UV light. Feelings of well-being and relaxation were also reported among the tanners.[11]
- Sun lamps are now being recommended for use by pregnant women who will give birth in a winter month. The recommendation is being made to protect the unborn child from osteoporosis during adulthood.[12]
- Research from Sweden demonstrated that women who use tanning beds more than three times yearly, had a reduced risk of endometrial cancer of 40- 50%.[13] The authors surmised that the effects observed were likely due to stimulating higher vitamin D levels in winter.
- Tanning-bed use reduces the risk of clots.[14] In an eleven-year study of the sun-exposure habits venous thrombotic (clotting) events of 40,000 women, it was found that women who sunbathed during the summer, on winter vacations, or when abroad, or used a tanning bed, were at 30% reduced risk of venous thrombotic events compared to those who did not. The authors again speculated that increased vitamin D, which has anticoagulant properties, resulted in these positive results.
- Tanning-bed use is associated to lower breast-cancer risk.[15]
- High quality tanning beds, because they provide UVB to both sides of the body simultaneously, stimulate the production of up to 10,000 IU of vitamin D in less than ten minutes. Ten minutes of tanning bed exposure can be done on a lunch break. That means they are more efficient than summer sun. Of course, those with darker skin will require a longer time to produce the same amount of vitamin D.
- It is likely that all benefits of sun can be provided by tanning beds, including increased resistance to cancer, osteoporosis, heart disease, diabetes, periodontitis, arthritis, infection and other maladies.
- Tanning beds may be used regardless of outside weather.
- Tanning beds may be used during “vitamin D winter.” This is especially important at higher latitudes that lack sufficient UVB from winter sun to stimulate adequate vitamin D production by the skin.
The truth about tanning beds and melanoma
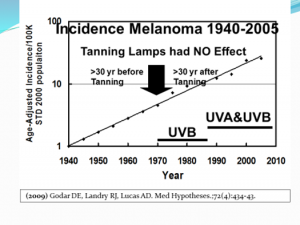
As we have shown, it is impossible to establish sun as the cause of melanoma; yet through chicanery and dishonesty, as established by Dr. Ackerman, we continue to see that the desire for profit produces chicanery, dishonesty and hypocrisy, which leads to the continuing mantra of the anti-sun movement—that melanoma is caused by our friend, the sun. That mantra is ludicrous, and the purveyors of the message are beginning to sound silly. We expect that due to the worry that the sun/melanoma message is ready to crash and burn, these same people are now attacking the tanning industry. One of the claims is that since the advent of tanning beds—in about 1970—melanoma has increased dramatically. While that is true, it has nothing to do with tanning beds. Melanoma was increasing steadily and exponentially long before tanning beds hit the scene and that rate of increase was not influenced by tanning beds. Dr. Diane Godar has produced a graph showing that tanning beds made no difference at all in the increase in melanoma. You will note that the rate of increase in melanoma is exactly the same now as it was since 1940. Dr. Godar’s graph is presented below.
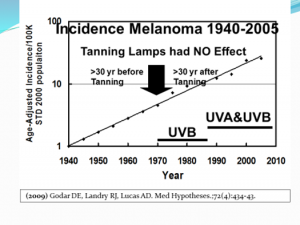
Those who oppose the use of tanning beds can conveniently ignore the rate of increase prior to the first tanning beds to make it appear that the tanning bed is the culprit. This is intellectual dishonesty, and it reminds me of the old saying, “There are lies and damn lies, and then there are statistics.” Twisting or ignoring the facts should be criminal.
Several studies have investigated the relationship of tanning-bed use to melanoma and a review of 22 investigations done from 1979 through 2002 showed that only four indicated tanning beds increased melanoma risk; eighteen showed no association.[16] One that showed an increased melanoma risk was conducted by Dr. Philippe Autier and colleagues in Belgium in 1991.[17] However, in 2002 Dr. Autier conducted another study in which no association between tanning bed use and melanoma was found.[18] This report stated, “No result suggested a dose-response curve, and no association was even present for subjects who reported more than 35 hours of cumulated tanning-bed use at least 19 yrs. before the interview. Our study doesn’t support the possibility that tanning bed use could increase melanoma risk.”
I looked for other studies that might have come to contrary conclusions and found one from 2007.[19] It was a meta-analysis of 19 studies that concluded tanning beds do increase the melanoma risk. However, when Dr. Grant assessed the meta-analysis, he noted that the studies failed to take skin type into consideration.[20] He re-analyzed the data and determined: “These results indicate that when studies largely influenced by inclusion of people with skin phenotype 1 [light-skinned non-tanners] without adjustment for skin phenotype are removed from the meta-analysis, no significant relation is found between tanning bed use and risk of CMM [cutaneous malignant melanoma].”
Several studies between 2003 and 2008 showed mixed results. One showed no significant increase in melanoma with tanning bed use.[21] Another study of five European countries showed that in France, where 20% of the population used tanning beds, their use was associated with a 19% increase in risk of melanoma.[22] In Sweden, where 83% of the population used tanning beds, there was a 38% decrease in melanoma. Overall, the risk of melanoma was reduced by 10% in tanning-bed users, although individuals with fair skin and a high number of moles were at increased risk. Clearly, studies that indict tanning beds, without taking into consideration skin type are flawed, and if they do not also differentiate between tanning and burning, they are doubly flawed.
Remember that excessive ultraviolet light exposure, whether it comes from sun or tanning lamps, causes burning. We have clearly established that burning may correlate to an increased risk of melanoma. Unfortunately, most of the studies that associated tanning beds with increased melanoma did not control for burning. Use of either sun exposure or tanning beds must be done prudently, so it is best to use professional tanning salons with trained personnel who assess skin type and make recommendations for the maximum time clients should tan.
Dr. Grant also reminds us that UVB is the most beneficial wavelength. UVA does have health benefits, including stimulating the production of nitric oxide, but excessive UVA is harmful in that it penetrates more deeply and generates free radicals that can lead to skin aging and DNA damage, as several studies have shown.[23] [24] [25] However, the tan produced by UVA serves as a protection against damage by further UVA. It is important to use tanning beds with outputs that mimic the midday, mid-latitude spring-and-summer UVB portion of total UV—roughly 3.5-5%. European countries limit UVB emitted from tanning beds to 1.5% of total UV radiation[26] [27]—a huge mistake. Tanning beds in the USA emit a much higher percentage of UVB, about 5% on average.[28] Prior to 1983, tanning beds used in Norway and Sweden were rich in UVB and there was no association between tanning-bed use and melanoma. Both the lamps and the acrylic sheet between the lamps and the person affect the UVB/UVA ratio; the acrylic, as it ages, decreases the UVB transmission more than UVA.
Personally, I have no qualms about using tanning beds, but I am not telling you to do the same. Read all the facts and then make up your own mind. Considering the numerous health benefits from high serum vitamin D levels and the production of endorphins, nitric oxide and other photoproducts, the slightly increased chance of rarely-fatal common skin cancer does not concern me.
A very light skin that does not tan, or a skin condition that is sensitive to UV may preclude tanning-bed use by some individuals. Those with freckles and red hair do not generally tan well, and should avoid tanning beds or limit themselves to very short exposures. In addition, it is a good idea to cover the face and genitals as those areas may be excessively sensitive to ultraviolet light. Others who may have adverse effects to tanning bed exposure are organ transplant recipients, those with many nevi (moles) or those taking photosensitive prescription drugs.[29] If you do not know if your drug is photosensitive, ask a pharmacist. Avoid even the least amount of burning.
Finally, it is a good idea to be checked regularly by a dermatologist to assess any changes that may occur to your skin. That advice, however, is even more important for those who do not use tanning beds or get regular sun, since more melanomas occur among those who receive little or no UVB, or in those irregularly exposed. In some cases, tanning beds may help the physical and mental health of people residing in the far north.
In one instance, tanning beds for Canadian military personnel may be essential to survival. The Canadian armed forces most remote outpost is also the northernmost community on Earth, and its purpose is to gather radio signals and other electronic intercepts from Russia and pass them to military analysts in the South.[30] The sun disappears on October 14 and does no reappear until February 28. During that time, temperatures drop to 5+ degrees below zero, and if the wind blow, the chill factor is incredibly low. The facility is build with most of the comforts of home, including gym facilities, and tanning machines that increase vitamin D levels are considered essential to life. We expect that if anyone were to try to take away those machines, it would cause an insurrection. In the previous blog, it was also mentioned that scientists have suggested the use of tanning beds for psoriasis when they were too far away from the dermatologists’ offices for a convenient visit.[31]
Tanning beds and other sources of ultraviolet light can be of great value to human health if they are used safely; the same can be said about the sun.
Are phototherapy sessions in a dermatologist’s office safe?
As we have indicated, dermatologists and their organizations, with certain refreshing exceptions, promote the idea that both tanning beds and natural sun exposure are detrimental to health. Yet, thousands of dermatologists use UVR light to reduce the risk of many skin diseases. They claim that their UVR exposure is totally safe. That is an blatant example of duplicity at its worst. Recently, Dr. Anne Haas, President of the California Dermatology Society, made an egregiously false statement at a regulatory hearing regarding UVR devices, saying that whereas tanning beds were cancer causers, the UVR devices used in dermatologists’ offices had never been shown to cause any cancer problems. Watch this short video to hear her statement:
Her statement, that there is no evidence UV devices in the dermatologist’s office cause cancer, is deceitful. Here is the truth:
- The light used by dermatologists is the same type of light used in tanning beds.[32] [33]
- The use of phototherapy in the dermatologist offices definitely do lead to an increase in skin cancer.[34] And some of that skin cancer was sufficiently noteworthy that the researchers concluded their study with this warning: “A noteworthy number of NMSC were diagnosed in this Mediterranean population of patients exposed to high-dose UV treatment. A thorough risk-benefit evaluation should always be done before UV treatment and patients should be carefully monitored for skin cancer during and after treatment discontinuation.”[35]
- The National Psoriasis Foundation recommends brief, frequent exposures of sunlight as a therapy and report that 80% of those who do it improve or totally clear psoriasis.[36]
- Many honest dermatologists recommend tanning-bed use to their patients to clear psoriasis. Obviously it is effective for that disease, and if phototherapy in the dermatologist’s office causes skin cancer, what seems to be the problem? Both therapies work. Why deny someone with psoriasis the benefits of a lower cost and possibly easier accessibility to treatment?[37]
So why the deception? The answer lies in money. When scientists such as those in the last quoted paper advocate tanning beds for therapy, it could cost the dermatology industry a fortune.
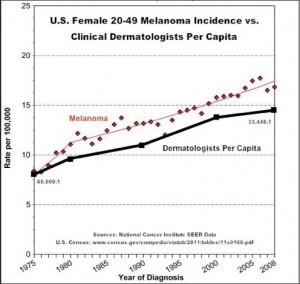
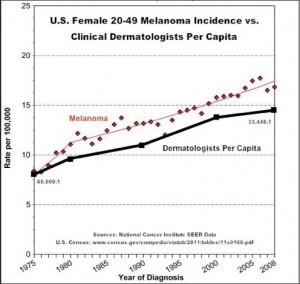
Your will note in the graph below that melanoma incidence has increased nearly in lockstep with the increase in the number of dermatologists. What a business! Is there any doubt why they don’t want the tanning industry absorbing the money made from their lucrative and expensive office treatments? Think about it.
Now you know a few more facts about sunlight, tanning beds, health and the deception of the anti-sun groups. Let it sink in and then make your own decision abut sun or tanning bed exposure. And while you decide, please consider the calculation I’ve made in my new book to be released soon: For every death caused by diseases that associate with sun exposure, there are about 350 deaths associated with sun deprivation. Which way would you like to bet?
[1] Tangpricha V, Turner A, Spina C, Decastro S, Chen TC, Holick MF. Tanning is associated with optimal vitamin D status (serum 25-hydroxyvitamin D concentration) and higher bone mineral density. Am J Clin Nutr 2004;80:1645-49.
[2] Hakim OA, Hart K, McCabe P, Berry J, Francesca R, Rhodes LE, Spyrou N, Alfuraih A, Lanham-New S. VITAMIN D PRODUCTION IN UK CAUCASIAN AND SOUTH ASIAN WOMEN FOLLOWING UVR EXPOSURE. J Steroid Biochem Mol Biol. 2016 Mar 22. pii: S0960-0760(16)30072-3. doi: 10.1016/j.jsbmb.2016.03.025. [Epub ahead of print] Review.
[3] Grant, W. Personal communication with the author, June, 2006
[4] Heaney RP, Dowell MS, Hale CA, Bendich A. Calcium Absorption Varies within the Reference Range for Serum 25-Hydroxyvitamin D. Journal of the American College of Nutrition 2003; 22: 142–146.
[5] Heaney, R. Vitamin D and calcium interactions: functional outcomes. Am J Clin Nutr 2008;88(suppl):541S–4S
[6] Radack KP, Farhangian ME, Anderson KL, Feldman SR. A review of the use of tanning beds as a dermatological treatment. Dermatol Ther (Heidelb). 2015 Mar;5(1):37-51.
[7] Science News, August 6, 2013. Summer sun good for psoriasis sufferers says Gottlieb dermatologist.
[8] Holick, M. Boston University. “Effects Of Vitamin D And Skin’s Physiology Examined.” Science Daily 21 February 2008 <http://www.sciencedaily.com¬ /releases/2008/02/080220161707.htm>.
[9] Kaur M, Feldman SR, Liguori A, Fleischer AB Jr. Indoor tanning relieves pain. Photodermatol Photoimmunol Photomed. 2005 Oct;21(5):278.
[10] Taylor SL, Kaur M, LoSicco K, Willard J, Camacho F, O’Rourke KS, Feldman SR. Pilot study of the effect of ultraviolet light on pain and mood in fibromyalgia syndrome. J Altern Complement Med. 2009 Jan;15(1):15-23.
[11] No authors listed. Tanning Beds Provide Potential Pain Relief for Fibromyalgia Patients. Wake Forest Baptist Medical Center Press release, 2009.
[12] Bukhari, M. Quoted in London Times April 27, 2008.
[13] Epstein E, Lindqvist PG, Geppert B, Olsson H. A population-based cohort study on sun habits and endometrial cancer. Br J Cancer. 2009 Aug 4;101(3):537-40.
[14] Lindqvist PG, Epstein E, Olsson H. Does an active sun exposure habit lower the risk of venous thrombotic events? A D-lightful hypothesis. J Thromb Haemost. 2009 Apr;7(4):605-10.
[15] Yang L, Veierød MB, Löf M, Sandin S, Adami HO, Weiderpass E. Prospective study of UV exposure and cancer incidence among Swedish women. J Intern Med. 2014 Jul;276(1):77-86
[16] International Smart Tan Network 2006. Research shows no connection between tanning and melanoma: Why this is misunderstood.
[17] Autier P1, Joarlette M, Lejeune F, Liénard D, André J, Achten G. Cutaneous malignant melanoma and exposure to sunlamps and sunbeds: a descriptive study in Belgium. Melanoma Res. 1991 Apr-May;1(1):69-74.
[18] Autier P, Tanning bed use and risk of melanoma: results from a large multicentric European study. Poster at the XVIII International Pigment Cell conference held 9-13 September 2002 at Egmond The Netherlands.
[19] International Agency for Research on Cancer Working Group on artificial ultraviolet light (UV) and skin cancer. The association of use of tanning beds with cutaneous malignant melanoma and other skin cancer: a systematic review. Int J Cancer 2007;120:1116-22.
[20] Grant, W. Insufficient evidence exists to link tanning bed use to risk of melanoma for other than those with skin phenotype 1. Sun, Nutrition and Health Research Center ( SUNARC). March 9, 2007. www. SUNARC org.
[21] Clough-Gorr KM1, Titus-Ernstoff L, Perry AE, Spencer SK, Ernstoff MS. Exposure to sunlamps, tanning beds and melanoma risk. Cancer Causes Control. 2008 Sep;19(7):659-69.
[22] Bataille V, Boniol M, De Vries E, Severi G, Brandberg Y, Sasieni P A multicentreepidemiological study on sunbed use and cutaneous melanoma in Europe. Eur J Cancer 2005;41:2141-49.
[23]Garland CF, Garland FC, Gorham ED. Epidemiologic evidence for different roles of ultraviolet A and B radiation in melanoma mortality rates. Ann Epidemiol. 2003;13:395-404.
[24] Moan J, Dahlback A, Setlow RB. Epidemiological support for an hypothesis for melanoma induction indicating a role for UVA radiation. Photochem Photobiol. 1999;70):243-7.
[25] Moan J, Porojnicu AC, Dahlback A, Setlow RB. Addressing the health benefits and risks, involving vitamin D or skin cancer, of increased sun exposure. Proc Natl Acad Sci U S A. 2008;15;105(2):668-73.
[26] Grant, W. Insufficient evidence exists to link tanning bed use to risk of melanoma for other than those with skin phenotype 1. Sun, Nutrition and Health Research Center (SUNARC). March 9, 2007. www. SUNARC org.
[27] Autier P. Perspectives in melanoma prevention: the case of tanning beds. Eur J Cancer 2004;40:2367-76.
[28] Grant W. Insufficient evidence exists to link tanning bed use to risk of melanoma for other than those with skin phenotype 1. Sun, Nutrition and Health Research Center (SUNARC). March 9, 2007. www. SUNARC org.
[29] Grant, WB. Personal communication with author.
[30] Matthew Fisher at CFS Alert: Canada’s “frozen Chosen” at top of the world have been in the dark since Oct 14. National Post February 2, 2013.
[31] Radack KP, Farhangian ME, Anderson KL, Feldman SR. A review of the use of tanning beds as a dermatological treatment. Dermatol Ther (Heidelb). 2015 Mar;5(1):37-51.
[32] Archier E1, Devaux S, Castela E, Gallini A, Aubin F, Le Maître M, Aractingi S, Bachelez H, Cribier B, Joly P, Jullien D, Misery L, Paul C, Ortonne JP, Richard MA. Carcinogenic risks of psoralen UV-A therapy and narrowband UV-B therapy in chronic plaque psoriasis: a systematic literature review. J Eur Acad Dermatol Venereol. 2012 May;26 Suppl 3:22-31.
[33] Radack KP, Farhangian ME, Anderson KL, Feldman SR. A review of the use of tanning beds as a dermatological treatment. Dermatol Ther (Heidelb). 2015 Mar;5(1):37-51.
[34] Egeberg A, Thyssen JP, Gislason GH, Skov L. Skin cancer in patients with psoriasis. J Eur Acad Dermatol Venereol. 2016 Mar 2. doi: 10.1111/jdv.13619. [Epub ahead of print].
[35] Maiorino A, De Simone C, Perino F, Caldarola G, Peris K. Melanoma and non-melanoma skin cancer in psoriatic patients treated with high-dose phototherapy. J Dermatolog Treat. 2016 Jan 28:1-5. [Epub ahead of print].
[36] National Psoriasis Foundation web site Oct. 2005.
[37] Radack KP, Farhangian ME, Anderson KL, Feldman SR. A review of the use of tanning beds as a dermatological treatment. Dermatol Ther (Heidelb). 2015 Mar;5(1):37-51.