New research from New Zealand shows that children who live in South Island of New Zealand have at least three times the risk of bowel disease such as Crohn’s disease (CD) and ulcerative colitis (UC)[1] when compared to those who live on the North Island. According to an article referencing this research, these bowel diseases usually appear in the pre-teen or teenage years and are incurable. The researchers believe that sun exposure and one of its photoproducts, Vitamin D, may play a part, although the low selenium content of the soil may also have an influence on bowel diseases.
New research from New Zealand shows that children who live in South Island of New Zealand have at least three times the risk of bowel disease such as Crohn’s disease (CD) and ulcerative colitis (UC)[1] when compared to those who live on the North Island. According to an article referencing this research, these bowel diseases usually appear in the pre-teen or teenage years and are incurable. The researchers believe that sun exposure and one of its photoproducts, Vitamin D, may play a part, although the low selenium content of the soil may also have an influence on bowel diseases.
In the southern hemisphere, of course, the farther south one travels, the colder and cloudier the weather becomes. Hence, the South Island has far less sun exposure than the North Island.
Although the researchers did not know for sure that the sunlight and vitamin D hypothesis was correct regarding bowel disease, their idea certainly has plenty to back it up. Crohn’s disease is closely correlated to vitamin D deficiency and winter season,[2] indicating an inverse relationship with sun exposure and vitamin D production. A study of female nurses in the US found that “compared with women residing in northern latitudes [in the northern hemisphere] at age 30, the multivariate-adjusted risk for UC for women residing in southern latitudes was less than half.”[3] Also, in a 12-year investigation of hundreds of thousands of bowel disease patients, hospitalizations, and prolonged hospitalizations, for both UC and CD were higher among those who had low sun exposure compared to those with very high sun exposure.[4]
It is important to understand that bowel disease causes malabsorption of nutrients in the gut, leading to diseases of malnutrition.[5] Vitamin D is one of the “nutrients” that may not be absorbed efficiently, and therefore sun exposure, not supplements, may be the only viable source of vitamin D for a person with bowel disease.
So for a healthy gut, sun exposure plays a vital role. Be sure to enjoy safe, non burning sun exposure whenever possible.
[1] http://www.radionz.co.nz/news/national/340048/shining-light-on-bowel-disease-rates
[2] Gilman J, Shanahan F, Cashman KD. Determinants of vitamin D status in adult Crohn’s disease patients, with particular emphasis on supplemental vitamin D use. Eur J Clin Nutr. 2006 Jul;60(7):889-96.
[3] Khalili H, Huang ES, Ananthakrishnan AN, Higuchi L, Richter JM, Fuchs CS, Chan AT. Geographical variation and incidence of inflammatory bowel disease among US women. Gut. 2012 Dec;61(12):1686-92.
[4] Limketkai BN, Bayless TM, Brant SR, Hutfless SM. Lower regional and temporal ultraviolet exposure is associated with increased rates and severity of inflammatory bowel disease hospitalization. Aliment Pharmacol Ther. 2014 Sep;40(5):508-17.
[5] Margulies SL, Kurian D, Elliott MS, Han Z. Vitamin D deficiency in patients with intestinal malabsorption syndromes–think in and outside the gut. J Dig Dis. 2015 Nov;16(11):617-33.
 Some time ago I wrote a blog on sun exposure and depression, emphasizing the importance of a protein called brain derived neurotropic factor (BDNF). This is an update.
Some time ago I wrote a blog on sun exposure and depression, emphasizing the importance of a protein called brain derived neurotropic factor (BDNF). This is an update.
BDNF is a factor in nerve growth and maturation, and is essential in synapse formation and plasticity. A lack of of it is implicated in psychiatric disorders such as schizophrenia, intellectual disability, autism and depression. Interestingly, it has been shown that unless there is sufficient BDNF in the brain, conventional antidepressants do not work very well,[1] and when BDNF is infused directly into the brains of rodents, it produces an antidepressant effect.[2]
It has also been shown that BDNF has a seasonal variation in concentration correlating with the amount of ambient sun; it increases in the spring and summer and decreases in fall and winter. [3] The authors of this research described the importance of their findings thusly: “This finding is important for our understanding of those factors regulating BDNF expression and may provide novel avenues to understand seasonal dependent changes in behavior and illness such as depression.”
BDNF has been shown to increase significantly after bright light exposure,[4] and in what we would consider to be a remarkably important study, both light exposure and treadmill exercise increased its expression of
in rats,[5] or as the researchers showed, exercise and/or bright light promoted neurogenesis (new nerve cell growth) in the adult rat brain. How important is this finding for adults who are worried about cognitive decline? We are actually seeing an example of new brain cells being built by bright light and exercise. What a wonderful way to help prevent Alzheimer’s disease and maintain mental sharpness into old age! Don’t forget your (safe) sunlight!
[1] Björkholma C, Monteggiab, L. BDNF — a key transducer of antidepressant effects. Neuropharmacology. 2016 March ; 102: 72–79.
[2] Siuciak JA, Lewis DR, Wiegand SJ, Lindsay RM. Antidepressant-like effect of brain-derived neurotrophic factor (BDNF). Pharmacol. Biochem. Behav. 1997; 56(1):131–137.
[3] Molendijk ML, Haffmans JP, Bus BA, Spinhoven P, Penninx BW, Prickaerts J, Oude Voshaar RC, Elzinga BM. Serum BDNF concentrations show strong seasonal variation and correlations with the amount of ambient sun. PLoS One. 2012;7(11):e48046.
[4] Tirassa P1, Iannitelli A, Sornelli F, Cirulli F, Mazza M, Calza A, Alleva E, Branchi I, Aloe L, Bersani G, Pacitti F. Daily serum and salivary BDNF levels correlate with morning-evening personality type in women and are affected by light therapy. Riv Psichiatr. 2012 Nov-Dec;47(6):527-34.
[5] Kwon SJ, Park J, Park SY, Song KS, Jung ST, Jung SB, Park IR, Choi WS, Kwon SO. Low-intensity treadmill exercise and/or bright light promote neurogenesis in adult rat brain. Neural Regen Res. 2013 Apr 5;8(10):922-9.
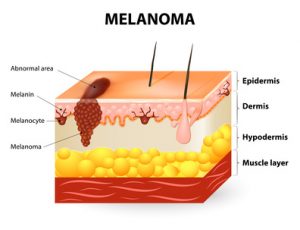
I have written several blogs making this melanoma case: not only is this deadly cancer not caused by sun exposure, but habitual, or regular, sun exposure has a protective effect against the disease. This blog will serve to reinforce and review the reasoning behind those conclusions.
A friend sent me a scientific paper[1] that I had forgotten or missed—a paper by Dr. Veronique Bataille that brought out several supportive points about how sun exposure protects against the disease. Here are a few of the salient ideas from the paper:
- The increase in melanoma is mostly seen for the thin types, which can’t be attributed to sun exposure but to increasing screening over the last 20 years. The fact is, that incidence appears to increase as the number of dermatologists and public health campaigns also increase. But the increase in melanoma is not real. This idea is perfectly plausible; when more dermatologists are available, and the public is driven to them by health campaigns more melanomas are found. Many “first-stage” or thin “thin” melanomas are discovered and counted that would not have been found in previous decades. This causes numbers to be highly inflated compared to the days when there were fewer dermatologists and fewer public health campaigns.
Comment: Another fact was not mentioned in the paper: Stunningly, a worldwide study of melanoma diagnosis and accuracy, published in the American Academy of Dermatology (AAD) showed that most diagnoses were incorrect.[2] Approximately 44 different authors from many different clinics and countries, including the US, contributed to the report. They made an accuracy-in-detection analysis based on the actual number of melanomas that were excised during a period of ten years, compared with the number that really needed to be excised. Many clinics in different countries were involved in assessing the numbers. The AAD research showed that only about 3.5% of diagnoses in non-specialized clinics, and 14.7% in specialized clinics, resulted in actually being melanoma. From this information, it is evident that many melanoma surgeries are bogus and may inflate the incidence of this deadly skin cacner.
What do we take away from this? There may be no real increase in melanoma, only an increase in assessment and excision.
- Low vitamin D levels are common in melanoma patients and have a deleterious effect on their risk and survival.
Comment: Low vitamin D levels are caused by sunlight deprivation; we are told to avoid the sun, but sun avoidance leads to vitamin D deficiency, which further leads to melanoma. If our population regularly enjoyed non-burning sun exposure, vitamin D levels would be much higher and the risk of melanoma much lower. This is corroborated by the fact that people who habitually work outdoors have a far lower risk of the disease. Dr. Cedric Garland and his colleagues showed that those who worked indoors had a 50% greater risk of than those who worked both indoors and outdoors.[3]
- An excess of naevi (moles), not sun exposure, is the strongest risk factor for melanoma, and when comparing the risk created by sunburns and fair skin to the risk created by an excess of moles, the moles create a 15-30 times higher risk.
Comment: Some very important research by Dr. Adele Green found that the strongest risk factor for both limb melanoma and trunk melanoma was the presence of more than 10 moles on the arm, which predicted a 42-times increased risk. [4] This means that public health campaigns should promote mole awareness! Unfortunately, they promote sun avoidance, which increases the risk of melanoma.
- Attempts to decrease melanoma incidence and mortality, by reducing sun exposure, has not been proven to work and may be harmful.
Comment: the statement is obviously true. In the U.S., Sun exposure has decreased by about 90% since 1935. During that same period, melanoma has increased by 3,000%.[5] Data from the Bureau of Labor statistics showed that indoor occupations such as “professional, managerial, clerical, sales, and service workers (except private household service workers) grew from one-quarter to three-quarters of total employment between 1910 and 2000.” The BLS also stated, during the same period, the outdoor occupation of farming declined by 96% from 33% to 1.2% of total employment. The data also show approximately 66% of the decline in the occupation of farmers and 50% of the decline in the occupation of farm laborers occurred after 1935.
Further information, this time from the Environmental Protection Agency (EPA) determined as of 1986, about 5 percent of adult men worked mostly outside, and about 10 percent worked outside part of the time. The proportion of women who worked outside was thought to be even lower.[6] These data demonstrate a dramatic shift from outdoor, sun-exposed activity to indoor, non-sun-exposed activity during the mid-to-late 20th Century. This change, nonetheless, has been accompanied by a 30-times increase in risk since 1935, the MIF-baseline year.
- Photoageing, which is skin ageing due to sunlight exposure, is not greater in melanoma patients than patients who do not have the disease. In fact, patients with the cancer exhibit less photoageing than those who do not have the disease.
Comment: This was a new research for me and it belied the idea that sun exposure caused melanoma. If sun exposure causes skin photoageing, and there is less photoageing on cancer sites, sun exposure cannot possibly be causing melanoma. Enough said.
We need our sunshine, and one of the reasons for that need is to prevent deadly cancers.
[1] Bataille V. Melanoma. Shall we move away from the sun and focus more on embryogenesis, body weight and longevity? Medical Hypotheses 81 (2013) 846–850.
[2] Argenziano G, Cerroni L, Zalaudek I, Staibano S, Hofmann-Wellenhof R, et al. Accuracy in melanoma detection: a 10-year multicenter survey.J Am Acad Dermatol. 2012 Jul;67(1):54-9.
[3] Garland FC, White MR, Garland CF, Shaw E, Gorham ED. Occupational sunlight exposure and melanoma in the U.S. Navy. Arch Environ Health. 1990 Sep-Oct;45(5):261-7.
[4] Green AC, Siskind V. Risk factors for limb melanomas compared with trunk melanomas in Queensland. Melanoma Res. 2012 Feb;22(1):86-91.
[5] Melanoma International Foundation, 2007 Facts about melanoma. Sources: National Cancer Institute 2007 SEER Database, American Cancer Society’s 2007 Facts and Figures, The Skin Cancer Foundation, The American Academy of Dermatology.
[6] US Congress, Office of Technology Assessment, Catching Our Breath: Next Steps for Reducing Urban Ozone, OTA-O-412 (Washington, DC: US Government Printing Office, July 1989).
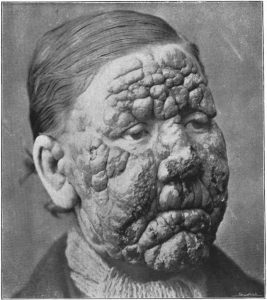 Leprosy is a bacterial disease that has been historically mentioned as a scourge, when it was considered to be incurable and disfiguring. Symptoms that develop include granulomas (inflammation caused by a collection of immune cells) of the nerves, respiratory tract, skin, and eyes. This may result in a lack of ability to feel pain, followed by the loss of parts of extremities, due to repeated injuries or infection of unnoticed wounds.[1] About 180,000 people worldwide are diagnosed with leprosy yearly, and about 100 people are diagnosed in the U.S. each year.[2] Leprosy has been considered to be a disease which has been eradicated, but such is not the case. For example, an article in an Indian paper shows it is much more prevalent in highly urbanized areas (areas of less sun) than in rural or less polluted areas[3] (areas of more sun). Also, when the bacteria that cause leprosy are exposed to ultraviolet light, the procedure kills half of the bacteria.[4] Therefore, sunlight may fight leprosy as it fights other bacteria, by stopping them at the source. Sun is a potent bactericide. Dr. Kime, in his book, Sunlight Could Save Your Life, reviewed the results of research conducted between 1886 and 1909. It showed the following bacteria were killed by ultraviolet light: anthrax, plague, streptococci, tubercle bacillus, cholera, staphylococcus, colon bacillus and dysentery bacillus. Sun was virtually forgotten with the advent of antibiotic drugs, but now the interest has returned. While watching a newscast, I noticed the news ticker announcing, “Sunshine is the most effective anti-infection therapy.” I believe that is true; sun exposure is provided to the earth to help prevent myriad diseases, but many of us try to avoid its healing powers. Non-burning sun exposure is a magnificent healer, and also a preventer of disease in those cases where it cleans the environment of noxious microorganisms.
Leprosy is a bacterial disease that has been historically mentioned as a scourge, when it was considered to be incurable and disfiguring. Symptoms that develop include granulomas (inflammation caused by a collection of immune cells) of the nerves, respiratory tract, skin, and eyes. This may result in a lack of ability to feel pain, followed by the loss of parts of extremities, due to repeated injuries or infection of unnoticed wounds.[1] About 180,000 people worldwide are diagnosed with leprosy yearly, and about 100 people are diagnosed in the U.S. each year.[2] Leprosy has been considered to be a disease which has been eradicated, but such is not the case. For example, an article in an Indian paper shows it is much more prevalent in highly urbanized areas (areas of less sun) than in rural or less polluted areas[3] (areas of more sun). Also, when the bacteria that cause leprosy are exposed to ultraviolet light, the procedure kills half of the bacteria.[4] Therefore, sunlight may fight leprosy as it fights other bacteria, by stopping them at the source. Sun is a potent bactericide. Dr. Kime, in his book, Sunlight Could Save Your Life, reviewed the results of research conducted between 1886 and 1909. It showed the following bacteria were killed by ultraviolet light: anthrax, plague, streptococci, tubercle bacillus, cholera, staphylococcus, colon bacillus and dysentery bacillus. Sun was virtually forgotten with the advent of antibiotic drugs, but now the interest has returned. While watching a newscast, I noticed the news ticker announcing, “Sunshine is the most effective anti-infection therapy.” I believe that is true; sun exposure is provided to the earth to help prevent myriad diseases, but many of us try to avoid its healing powers. Non-burning sun exposure is a magnificent healer, and also a preventer of disease in those cases where it cleans the environment of noxious microorganisms.
[1] https://en.wikipedia.org/wiki/Leprosy
[2] http://www.webmd.com/skin-problems-and-treatments/guide/leprosy-symptoms-treatments-history#1
[3] Kumar, R. Urbanites More Prone to Leprosy. Merinews April 14, 2008. (available at http://www.merinews.com/catFull.jsp?articleID=132447)
[4] Truman RW, Gillis TP. The effect of ultraviolet light radiation on Mycobacterium leprae. Int J Lepr Other Mycobact Dis. 2000 Mar;68(1):11-7.
 Sun exposure is crucial to preventing multiple sclerosis (MS), the terrible, debilitating autoimmune disease in which T-cells initiate an inflammatory response against myelin, the protective cover of nerves.[1],[2] This leaves the nerves bare and susceptible to “short circuiting,” a process known as demyelination. This attack prevents proper functioning within the brain and body, which leads to a variety of symptoms like vision changes, muscle spasms, and numbness. These symptoms profoundly decrease the ability to function and destroy the quality of life.
Sun exposure is crucial to preventing multiple sclerosis (MS), the terrible, debilitating autoimmune disease in which T-cells initiate an inflammatory response against myelin, the protective cover of nerves.[1],[2] This leaves the nerves bare and susceptible to “short circuiting,” a process known as demyelination. This attack prevents proper functioning within the brain and body, which leads to a variety of symptoms like vision changes, muscle spasms, and numbness. These symptoms profoundly decrease the ability to function and destroy the quality of life.
We have known for decades that people who live in areas of low sun exposure, such as far-northern or far southern countries, have a far greater risk of contracting MS than those who live in countries closer to the equator. In fact, there is more than 100 times the risk of MS in far northern as in equatorial areas, where sun is intense, and the rate of MS approaches zero.[3],[4],[5]
I ran across an interesting study demonstrating that the age at which the low sun exposure occurs is also a predictive factor in the risk of MS.[6] It showed that in Norway, the amount of sun exposure in the period of life between 16-18 years of age was critical in predicting the disease. Those youngsters who experienced the lowest sun exposure during those ages were 83% more likely to develop MS. The same research showed that in Italy the critical period was between birth and age 5 years, with those receiving the lowest sun exposure being 56% more likely to develop MS.
I spite of incontrovertible research that proves regular, non-burning sun exposure is critical for human health, the sunscare movement continues to promote the idea that we should avoid the sun. The blood is on their hands.
[1] Racke, M. Immunopathogenesis of multiple sclerosis. Ann Indian Acad Neurol. 2009 Oct–Dec; 12(4): 215–220.
[2] Markovic-Plese S, McFarland HF. Immunopathogenesis of the multiple sclerosis lesion. Curr Neurol Neurosci Rep 2001;1:257-62
[3] Alter M, Yamoor M, Harshe M. Multiple sclerosis and nutrition. Arch Neuroll974;31:267-72.
[4] Kurtkze, J. Geography in multiple sclerosis. J Neurol1977;215:1-26.
[5] Hayes CE, Cantorna MT, DeLuca HF. Vitamin D and multiple sclerosis. Proc Soc Exp Biol Med 1997;216:21-27
[6] Bjørnevik K, Riise T, Casetta I, Drulovic J, Granieri E. et al. Sun exposure and multiple sclerosis risk in Norway and Italy: The EnvIMS study. Mult Scler. 2014 Jul;20(8):1042-9.
Diabetes and sun exposure By Marc Sorenson, EdD.
Diabetes is a disease of chronically high blood glucose leading to blindness, nerve damage, heart disease and numerous other maladies. Diabetes comes in two forms: (1) Type-one, in which there is damage to the islet cells of the pancreas. This is usually due to an autoimmune response, and the damage prevents production of insulin responsible for removing glucose from the blood. (2) Type-two, in which insulin is produced, but blood glucose remain high due to insulin resistance. In this article, we will discuss type-two, which is by far the most common type. As with heart and vascular disease, we must realize a paucity of sunlight is not the cause of either type of diabetes; rather it is caused by deleterious nutrition habits, primarily high meat consumption,[1] [2] [3] sugar consumption,[4] [5] egg consumption,[6] low consumption of fruits and vegetables, and too many fried foods.[7] In the case of type-one, milk consumption may be the most important nutritional factor.[8] However, sunlight may act as a prophylactic against either type of diabetes. With either type of diabetes, it is not usually the diabetes that kills, but other diseases resulting from it.
There are several studies showing a relationship between type-two diabetes mellitus (DM) and sun exposure or UVB exposure. One paper showed blood-sugar levels were lower during the summer,[9] and another demonstrated exposure to sun lamps increased insulin secretion.[10] It has also been found there is a direct and significant association between low 25(OH)D levels (a surrogate measure for low sun exposure) and increased risk of type-two.[11]
In addition, a meta-analysis produced moderate evidence that recreational sun exposure is associated with a reduced risk of type-two.[12] The study was undertaken because of the observation by researchers showing that although higher 25(OH)D levels were consistently associated with a lower risk of diabetes, supplementing 25(OH)D had shown no such effects. They hypothesized sun exposure could have influences not related to vitamin D, and such seems to have been the case.
Another of the more important investigations showed that women who had “active sun exposure habits” had a 30% reduced risk of type-two.[13]
Diabetes is increasing very rapidly and may someday overwhelm the health-care system. In my opinion, it is the most easily reversed of all degenerative diseases, so this is a tragedy. Proper nutrition, exercise and safe sun exposure can prevent almost all type-two diabetes. At our former resort, about two-thirds of type-two diabetics were free of all medication in two weeks. It is a totally unnecessary disease. If you don’t have it, prevent it. If you have it, reverse it. Start today.
[1]FeskensEJ, Sluik D, van WoudenberghGJ. Meat consumption is an important risk factor Meat consumption, diabetes, and its complications. Curr Diab Rep. 2013 Apr;13(2):298-306.
[2]Kim Y, Keogh J, Clifton P. A review of potential metabolic etiologies of the observed association between red meat consumption and development of type 2 diabetes mellitus. Metabolism. 2015 Jul;64(7):768-79.
[3]Muntoni S, Mereu R, Atzori L, Mereu A, Galassi S, Corda S, Frongia P, Angius E, Pusceddu P, Contu P, Cucca F, Congia M, Muntoni S. High meat consumption is associated with type 1 diabetes mellitus in a Sardinian case-control study. Acta Diabetol. 2013 Oct;50(5):713-9.
[4] Imamura F, O’Connor L, Ye Z, Mursu J, Hayashino Y, Bhupathiraju SN, ForouhiNG.Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-analysis, and estimation of population attributable fraction. BMJ. 2015 Jul 21;351:h3576.
[5] Lamb MM, Frederiksen B, Seifert JA, Kroehl M, Rewers M, Norris JM. Sugar intake is associated with progression from islet autoimmunity to type 1 diabetes: the Diabetes Autoimmunity Study in the Young. Diabetologia. 2015 Sep;58(9):2027-34.
[6]DjousséL1, Gaziano JM, Buring JE, Lee IM. Egg consumption and risk of type 2 diabetes in men and women.Diabetes Care. 2009 Feb;32(2):295-300
[7]McEvoy CT, Cardwell CR, Woodside JV, Young IS, Hunter SJ, McKinley MC.A posteriori dietary patterns are related to risk of type 2 diabetes: findings from a systematicreview and meta-analysis.J Acad Nutr Diet. 2014 Nov;114(11):1759-75.
[8] Karjalainen J, Martin JM, Knip M, Ilonen J, Robinson BH, Savilahti E, Akerblom HK, Dosch HM. A bovine albumin peptide as a possible trigger of insulin-dependent diabetes mellitus. N Engl J Med. 1992 Jul 30;327(5):302-7.
[9] Ishii H,Suzuki H, Baba T, Nakamura K, Watanabe T. Seasonal variation of glycemic control in type-2 diabetic patients. Diabetes Care 2001;24;1503.
[10] Colas C, Garabedian M, Fontbonne A, Guillozo H, Slama G, Desplanque N, Dauchy F, Tchobroutsky G. Insulin secretion and plasma 1,25(OH)2D after UV-B irradiation in healthy adults. Hormone and Metabolic Research 1988;21:154-155.
[11] Song Y, Wang L, Pittas AG, Del Gobbo LC, Zhang C, Manson JE, Hu FB. Blood 25-hydroxy vitamin D levels and incident type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2013 May;36(5):1422-8.
[12] Shore-Lorenti C, Brennan SL, Sanders KM, Neale RE, Lucas RM, EbelingPR.Shining the light on Sunshine: a systematic review of the influence of sun exposure on type 2 diabetes mellitus-related outcomes. Clin Endocrinol (Oxf). 2014 Dec;81(6):799-811.
[13]Lindqvist PG, Olsson H, Landin-Olsson M. Are active sun exposure habits related to lowering risk of type 2 diabetes mellitus in women, a prospective cohort study? Diabetes Res Clin Pract. 2010 Oct;90(1):109-14.
By Marc Sorenson, EdD, for sun exposure…
A new research paper on sun exposure and cancer has some interesting observations and some errors.[1] It is entitled, Does Sunlight protect us from cancer? Here is the abstract of the article, verbatim.
“The Ultraviolet (UV) radiation contained in sunlight is a powerful mutagen and immune suppressant which partly explains why exposure to solar UV is the biggest risk factor for the development of cutaneous tumors. Evidence is building that sunlight may be protective against some internal malignancies. Because patients with these tumors are often vitamin D deficient, this has led some to propose that vitamin D supplementation will be beneficial in the treatment of these cancers. However, the results from already completed trials have been disappointing which has given weight to the argument that there must be something else about sunlight that explains its cancer-protecting properties.”
The first sentence, of course, is false. The idea, that sun exposure is the biggest risk factor for skin cancer, is erroneous. We have presented materials many times, proving that melanoma is not caused by sun exposure, and that sun exposure is protective against that disease. And as regards common skin cancers, we have shown that high-fat nutrition, lack of antioxidants, meat consumption and alcohol intake are all risk factors. Search the blogs on this site to read the different articles.
The statement is correct, of course, that sunlight is protective against many internal cancers. Dr. Bill Grant and I are finishing our book, Embrace the Sun, where we present nearly all of the research on the protective influence of sun exposure against cancer.
The statement that vitamin D research has been disappointing is both true and false. Randomized controlled studies (RCTs) have shown the vitamin D supplements do have a protective effect against internal cancers, contrary to the statement by the researchers.
Finally, let’s look at the statement that there is something beyond vitamin D that explains the cancer-protecting properties of sun exposure. That is partially true. Beyond vitamin D, the sun causes the production of nitric oxide, serotonin, endorphin and BDNF, all of which are vital to human health, and may have their own cancer-protective properties.
The bottom line? Eat correctly (avoid junk), REGULARLY soak up some sun around midday and get plenty of exercise. That advice will be a boon to your health in myriad ways.
Sun and cognitive ability by Marc Sorenson, EdD, Sunlight Institute…
If you have depression, you may also have cognitive impairment, according to older research that I just became aware of. The researchers measured cognitive abilities among approximately 14,000 depressed subjects and then exposed them to either one day of sunlight or two weeks of sunlight. They then determined if cognitive disabilities were associated with the sun they obtained.[1]
The results were impressive: Those who were sun-deprived for two weeks had 2.5 times the risk of being cognitively impaired, compared to those who had sufficient sunlight. A one-day exposure made no significant difference in cognition.
Results of other research, based on a 15-year residential history of varying degrees of sun exposure, has also shown that cognitive impairment in persons who were below the median exposure to sun, was 88% greater than those who were above the median.[2] The researchers mentioned vitamin D as a possible mechanism by which sun positively influenced cognition, but they also remarked that regulation of the circadian rhythm by sunlight could be a factor.
Several other studies showed a close, positive association between vitamin D levels and cognition, and as we know, vitamin D levels in most cases are a surrogate measurement for sun exposure.
The message is to get plenty of sunlight to improve mental clarity. Happy thinking!
[1] Shia T Kent, Leslie A McClure, William L Crosson, Donna K Arnett, Virginia G Wadley and Nalini Sathiakumar. Effect of sunlight exposure on cognitive function among depressed and non-depressed participants: a REGARDS cross-sectional study. Environmental Health 2009, 8:34
[2] Kent ST, Kabagambe EK, Wadley VG, Howard VJ, Crosson WL, Al-Hamdan MZ, Judd SE, Peace F, McClure LA. The relationship between long-term sun radiation and cognitive decline in the REGARDS cohort study. Int J Biometeorol. 2014 Apr;58(3):361-70.
In a new scientific paper, Dr. MS Razzaque shows that there may be some downsides to vitamin D supplementation, including “cardiovascular events and beyond.” He also states that “since hypovitaminosis D status usually reflects reduced sunlight exposure, the obvious primary replacement should be safe sunlight exposure, and not exogenous supplements.”[1]
The paper specifically mentions that avoiding sunlight exposure may influence the initiation and progression of different types of tumors [cancer], high blood pressure, type 1 diabetes and multiple sclerosis. It also points out that there may be some deleterious consequences of vitamin D supplementation, although in my opinion, the dosage would need to by quite high.
As I have indicated in many of my posts on the Sunlight Institute site, sun exposure is the most natural way to obtain vitamin D, and it has no toxicity, since it is self-regulated.
What wasn’t mentioned was the production of health-promoting substances when sun touches the skin, e.g. endorphins and nitric oxide. And of course, the sun helps the brain to produce serotonin and BDNF, which are critical for proper brain function.
So soak up your sunlight but don’t burn.
[1] Razzaque MS. Sunlight exposure: Do health benefits outweigh harm? J Steroid Biochem Mol Biol. 2016 Sep 16. [Epub ahead of print].
By Marc Sorenson, EdD. Sunlight Institute
Although I occasionally try to balance the messages about tanning beds, this blog is meant neither to discourage nor promote their use. The readers should make up their minds after weighing the evidence. In a recent blog, I mentioned some positive messages about tanning-bed use, which included the following:[1] Note: all references for the following list are found in the blog under footnote 1.
- Tanning-bed use is associated with a reduced risk of clots.
- Tanning-bed use is associated with increased vitamin D levels.
- Tanning-bed use is associated with stronger bones
- Tanning-bed use can cure psoriasis and eczema and tanning beds are often recommended by dermatologists.
- Tanning-bed use more than three times yearly is associated with a 40-50% reduced risk of endometrial cancer.
- Tanning-bed use is associated to lower breast-cancer risk.
After I posted the above information, a friend from Canada reminded me of research by Dr. Pelle Lindqvist and his colleagues, which demonstrated that both sun exposure and tanning-bed exposure reduced the risk of death during a 20-year study.[2] Women who used tanning beds were 23% less likely to die of any cause than women who did not use them.
In addition, I remembered an older study that showed that tanning beds were able to take winter vitamin D levels up to summer levels in a period of five weeks.[3]
So, along with the bad rap tanning beds are receiving, there is some good news. Who wouldn’t want to live longer in better health? Still, as with all decisions, weigh the evidence and then decide.
[1] http://sunlightinstitute.org/defending-the-sun-from-the-lies-damn-lies-duplicity-deception-death-and-disease-of-the-anti-sun-business-part-3/
[2] Lindqvist P. Epstein E, Landin-Olsson M, Ingvar C, Nielsen K, Stenbeck M, Olsson H. Avoidance of sun exposure is a risk factor for all-cause mortality: Results from the Melanoma in Southern Sweden cohort
[3] Moan J, Lagunova Z, Cicarma E, Aksnes L, Dahlback A, Grant WB, Porojnicu AC. Sunbeds as vitamin D sources. Photochem Photobiol. 2009 Nov-Dec;85(6):1474-9.