First of all, to think is to prevent poor test scores, win at business and otherwise be successful. And, if I think and remember clearly, I also prevent mental disabilities such as Alzheimer’s. Consequently, there are innumerable pills on the market that purportedly increase the ability to think. But you may need only one pill to improve your cognitive ability: the sunshine pill. It is most noteworthy that I’m not talking about vitamin D. Therefore, the sunshine pill is not really a pill at all. Rather, it is exposure to the UV light of sunlight itself, which helps prevent myriad diseases. Maybe we should call it the “magnificent non-pill.”
First of all, to think is to prevent poor test scores, win at business and otherwise be successful. And, if I think and remember clearly, I also prevent mental disabilities such as Alzheimer’s. Consequently, there are innumerable pills on the market that purportedly increase the ability to think. But you may need only one pill to improve your cognitive ability: the sunshine pill. It is most noteworthy that I’m not talking about vitamin D. Therefore, the sunshine pill is not really a pill at all. Rather, it is exposure to the UV light of sunlight itself, which helps prevent myriad diseases. Maybe we should call it the “magnificent non-pill.”
How does the sunshine pill help us to think?
Recent research shows that exposure to sunlight causes a cascade of chemical reactions that help us to think.[1] Especially relevant is the fact that exposure to UV elevates a natural chemical known as blood urocanic acid (UCA). This chemical then crosses the blood-brain barrier. This chemical is then converted by a metabolic process to glutamate, and consequently, nerve synapses in the brain are enhanced. As a result, there were improvements in both physical learning (motor learning) and object recognition memory, which is an ability to think.
Is there more research indicating that sun exposure enhances the ability to think?
In addition, the ability to think has been shown in many research studies to improve with sunlight. Most noteworthy is a 2013 article, published in the journal Neurology.[2] It reveals that among people with high sun exposure, the risk of Alzheimer’s disease (AD) is profoundly decreased. Therefore, they are able to think more clearly than those who receive low sun exposure.
Finally, research published in the journal Endocrinology, sums up the effects of the sun on the brain and body: It is entitled, “How ultraviolet light touches the brain and endocrine system through skin, and why.”[3] The authors begin their abstract by stating that “the skin is a self-regulating protective barrier organ that is empowered with sensory and computing capabilities to counteract the environmental stressors to maintain/restore disrupted cutaneous homeostasis.” In other words, the skin has the ability to take on what life deals it, and maintain its equilibrium and balance. In addition, the skin communicates bidirectionally with the central nervous, endocrine and immune systems. Thus, it helps to maintain balance for all body systems, including the ability to think.
Safely soak up the non-burning sunlight and enhance your intelligence!
[1] Zhu et al., 2018, Cell 173, 1–12, June 14, 2018
[2] White RS, Lipton RB, Hall CB, Steinerman JR. Nonmelanoma skin cancer is associated with reduced Alzheimer disease risk. Neurology. 2013 21;80(21):1966-72.
[3] Slominski AT, Zmijewski MA, Plonka PM, Szaflarski JP, Paus R. How ultraviolet light touches the brain and endocrine system through skin, and why. Endocrinology. 2018 Mar 12. [Epub ahead of print]
 New book, Embrace the Sun, recommends non-burning sun exposure, citing research on sun exposure, vitamin D, and disease risk.
New book, Embrace the Sun, recommends non-burning sun exposure, citing research on sun exposure, vitamin D, and disease risk.
Available on Amazon, Embrace the Sun, by authors Marc B. Sorenson, Ed.D. and William B. Grant, Ph.D., claim that sun avoidance may be nearly as hazardous to your health as cigarette smoking! Will there soon be a Surgeon General’s warning about staying indoors or putting on too much sunscreen? Is this book based on science or pure science fiction?
The book is based on science and research. Together, Sorenson and Grant have worked 62 years studying and practicing health, nutrition, and the proper relationship with sunlight. A mountain of evidence exists showing that sunlight can promote weight loss, reduce depression, and profoundly decrease the risk of today’s common diseases including most cancers, heart disease, autism, diabetes, osteoporosis, multiple sclerosis, infertility, preterm birth and psoriasis. Do I have your attention? This book provides solid evidence towards a case for regular, sensible sun.
“Marc Sorenson and Bill Grant take us on a delightful journey to better understand the health benefits of our magnificent sun at a time when our sun has been demonized by various health organizations, including the dermatology community, which has been essentially unchallenged for the past 50 years,” said Michael F. Holick, Ph.D., M.D., Boston University Medical Center, “Embrace the Sunis an easy read that is chock-full of valuable information about the health benefits of sensible sun exposure. It provides a very practical guide on how to take advantage of our Magnificent Sun.”
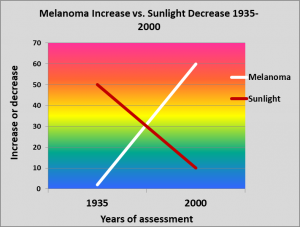 According to the book, 75% of all melanomas occur on areas of the body that are seldom or never exposed to sunlight. Additionally, sun exposure has decreasedby about 90% in the U.S. population since 1935. During that same period, melanoma incidence has increasedexponentially, by approximately 3,000%! This evidence debunks the myth that melanoma is caused primarily by the sun, and instead suggests that the disease is at least partially caused by sun deprivation.
According to the book, 75% of all melanomas occur on areas of the body that are seldom or never exposed to sunlight. Additionally, sun exposure has decreasedby about 90% in the U.S. population since 1935. During that same period, melanoma incidence has increasedexponentially, by approximately 3,000%! This evidence debunks the myth that melanoma is caused primarily by the sun, and instead suggests that the disease is at least partially caused by sun deprivation.
“This book is a tour de force for health effects of exposure to the sun,” said Cedric F. Garland, Dr. Ph. F.A.C.E., University of California at San Diego. “It is written simply enough and in such a light-hearted vein that any intelligent fifth grader can and should read it. It also should be required reading for every upcoming doctor in training and all health care professionals.”
Sorenson and Grant prepare the reader to make an informed choice. With summer coming, is it wise to get out regularly at midday, exercise, and soak up some rays? Or better to stay indoors, continuing the current regimen? Could it be that something so central to nature, the sun, which has been part of the human race for thousands of years is now bad for us? In this blip that is the late 20thand beginning 21stcentury has sun avoidance been helpful or hurtful? Read Embrace the Sun and find out!
About Marc B. Sorenson, Ed. D.
Dr. Sorenson is a doctor of education (EdD) with a health background. He and his wife, Vicki, developed one of the world’s top resorts (National Institute of Fitness). During 20 years, their clients lost over 100 tons of fat; two thirds of diabetic guests were freed of medication in two weeks; and others recovered from cholesterol, arthritis, and myriad additional maladies. Sorenson has written ten books and hundreds of blogs for his site, Sunlight Institute. On the recommendation of Senator Orrin Hatch, a flag was flown over the U.S. Senate building to honor his contributions to world health.
About William B. Grant, Ph.D.
Dr. William Grant is an epidemiologist and founder of the nonprofit organization Sunlight, Nutrition and Health Research Center. Grant holds a PhD in Physics from UC Berkeley and worked as a senior research scientist in the field of optical and atmospheric sciences at SRI International, JPL, and NASA Langley.
He published the first paper linking dietary factors to risk of developing Alzheimer’s disease in 1997. Since 2000, he has focused on ultraviolet-B (UVB) radiation and vitamin D and their relation to cancer and other diseases. He has written over 256 peer-reviewed articles, editorials, and letters to the editor on vitamin D and health.
What is Alzheimer’s disease?
By Marc Sorenson, EdD, Sunlight Institute
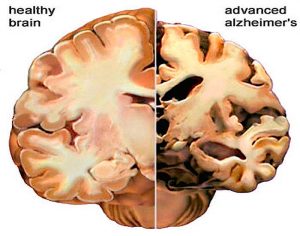
Alzheimer’s disease is a plague in our modern world. It is a progressive mental deterioration that can occur in middle or old age, due to degeneration of the brain. Alzheimer’s is also the most common cause of premature senility. The United States will see a 44 percent increase in individuals with Alzheimer’s disease by 2025.[1] First of all, the disease occurs because amyloid plaques appear in brain tissue. These plaques consist of tangles of amyloid protein (a complex protein resembling starch) in nervous tissue. They are pathological markers of the disease that are found in spaces between the brain’s nerve cells. As a result of these plaques, the brain loses its ability to function properly.
Our experience with Alzheimer’s sufferers
My wife, Vicki, and I worked with residents of an assisted-care facility for over three years. We conducted and supervised church meetings for many disabled, elderly people. Because we worked up close and personally with these residents, we understood the devastating effects of Alzheimer’s. Many of these residents could not find their way to the church meeting room without our assistance. Therefore, they obviously had the disease. Additionally, it was manifest because many of them were unable to recognize us after our being away for a day. Also, they were prone to simply get up and leave the building and be found (if lucky) wandering outside.
Does sun exposure help to reduce Alzheimer’s?
First of all, research indicates that vitamin D and omega 3 fatty acids may help in removing the aforementioned plaques.[2] Therefore, they reduce the risk or severity of AD. So, the disease may be lessened by sun exposure, since 90% of vitamin D produced in the US population is due to sun exposure.[3]
Hence, it is no surprise that the latest research paper found high risk in low-sunlight countries. Consequently, the researchers stated: “According to sunlight data, we can conclude that countries with low average sunlight have high AD (Alzheimer’s disease) death rate.[4]”
Are there other indications that sun exposure is associate to reduced risk?
Sun exposure directly correlates to non-melanoma skin cancer (NMSC). Therefore, the latter is often used as a sun-exposure indicator. It is thus compared with various diseases to evaluate the relationship between them and sun exposure. A 2013 article, published in the journal Neurology, reveals that among people with NMSC, the risk of Alzheimer’s disease (AD) is profoundly decreased:[5] Those with NMSC had a 79% reduction in disease risk. Stated another way, those without NMSC had about five times the risk of Alzheimer’s! Of course, this demonstrates the importance of sun exposure in reducing the risk, whether due to vitamin D production of from other photoproducts of the sun.
So, what is the bottom line? Be sure to obtain some unscreened, non-burning sun exposure and keep your marbles!
[1] Disease growth: U.S. will see average 44 percent increase in Alzheimer’s disease by 2025. Alzheimer’s Association 2015. https://www.alz.org/alzwa/documents/alzwa_resource_ad_fs_ad_state_growth_stats.pdf
[2] Champeau R. Vitamin D, omega-3 help clear amyloid plaques found in Alzheimer’s. UCLA Newsroom 2013.
[3] Reichrath J. The challenge resulting from positive and negative effects of sun: how much solar UV exposure is appropriate to balance between risks of vitamin D deficiency and skin cancer? Prog Biophys Mol Biol 2006;92(1):9-16
[4] Câmara AB, de Souza ID, Dalmolin RJS. Sunlight Incidence, Vitamin D Deficiency, and Alzheimer’s Disease. J Med Food. 2018 Mar 22 [Epub ahead of print].
[5] White RS, Lipton RB, Hall CB, Steinerman JR. Nonmelanoma skin cancer is associated with reduced Alzheimer disease risk. Neurology. 2013 21;80(21):1966-72.
MS prevention by sunlight. By Marc Sorenson, Ed.D. Sunlight Institute
What is MS?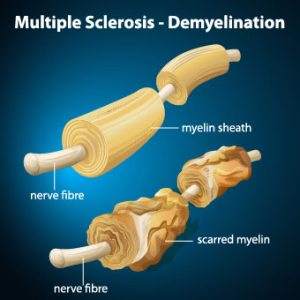
MS is a painful, debilitating, crippling, disease in which immune cells initiate an inflammatory response against myelin. Myelin is the nerves’ protective cover. It is rather like an electric wire that has lost its rubber cover. So, this process, known as demyelination, leaves the nerves bare and susceptible to “short circuiting.” From 85 to 170 people per 100,000 in the USA suffer from MS, and the rate among women, during the period from 1991 through 1994, has increased by 50% compared to the period from 1982 through 1986. Also, as of 2010, the last year for which we could find statistics, there were 350,000-400,000 cases diagnosed in the USA.
There is no doubt that sunshine reduces the risk of MS, because The risk of multiple sclerosis in far northern areas, where there is little sunshine, is more than 100 times greater than it is in equatorial areas. So, in those areas, where sunlight is intense, due to directness of the sun, the rate of MS approaches zero. [1], [2], [3]
And do you know anyone who suffers from multiple sclerosis? They should probably read this blog and then obtain plenty of non-burning sun exposure.
The latest Research on MS, sun exposure and vitamin D.
A study carried out in Southern California corroborates the sun exposure benefits to MS reduction.[4] First of all, the researchers recruited members of three different ethnicities (blacks, Hispanics and whites). In addition, they further divided those ethnicities into those who suffered from MS (known as cases) and those who were free from the disease (controls). They then simultaneously examined lifetime sun exposure and blood vitamin D levels, accounting for genetic ancestry and other factors. The results were impressive:
- Among blacks, the highest lifetime sun exposure was associated with a 47% lower risk, independently of blood levels of vitamin D.
- Among whites, the highest lifetime sun exposure was associated with a 32% lower risk. In this group, highest vitamin D levels also associated with a lower risk of MS.
- Among Hispanics, the highest lifetime sun exposure was associated with a 34% lower risk, independently of blood levels of vitamin D.
This is just the latest research to determine that sun exposure lessened the risk of MS independently of vitamin D. In addition, researchers used animals with experimental autoimmune encephalomyelitis (EAE) (an experimental form of MS). It was induced in animals in a lab setting and then used to determine the relative influences of UVR and vitamin D on MS. In conclusion, they stated, “These results suggest UVR [sun] is likely suppressing disease independent of vitamin D production. Thus, vitamin D supplementation alone may not replace the ability of sun (UV) to reduce MS susceptibility.”[5]
More on sunlight and MS from the same researchers
Later on, some of these same researchers investigated the mechanism by which sun exposure suppressed the disease and determined that UV light selectively inhibits spinal cord inflammation and demyelination.[6]
Furthermore, in another study, scientists performed an investigation with UVR. UVR is the same radiation emitted by the sun and sunbeds or sunlamps. It was administered to animals with EAE.[7] First of all, the researchers found that UVR treatments stopped inflammation and demyelination of the spinal cord. It did so by inhibiting a chemical known as a chemokine, also known as a cytokine. Cytokines are specialized proteins that are either inflammatory or anti-inflammatory in their nature. Therefore, inflammatory cytokines or chemokines are the cause of inflammation and autoimmune attacks resulting in MS. In addition, UVR directly initiated the MS-ameliorating effects, independent of vitamin D.
To conclude:
Finally, as wonderful as vitamin D is, we should realize this: The production of vitamin D is only one of the profoundly healthful effects that are due to Sun Exposure. Hence, those who take vitamin D and believe they will derive all the benefits of sun exposure, are wrong. Consequently, they could be “dead wrong” in the case of a scourge like MS. So, be sure to obtain your full share of non-burning sunlight whenever possible. It could save your life. And, it could save the lives of those who have the disorder or who might be susceptible to it. Maybe we should start paying more attention to our sun exposure?
This is one of many blogs that I and others have written on this subject. In addition, here are a few more that may interest you:
http://sunlightinstitute.org/research-shows-sun-exposure-thwarts-multiple-sclerosis-ms/
http://sunlightinstitute.org/a-vitally-important-study-on-sunlight-and-multiple-sclerosis-ms/
Embrace the sun! Without burning, of course
[1] Alter M, Yamoor M, Harshe M. Multiple sclerosis and nutrition. Arch Neurol l974;31:267-72.
[2] Kurtkze, J. Geography in multiple sclerosis. J Neurol 1977;215:1-26.
[3] Hayes CE, Cantorna MT, DeLuca HF.Vitamin D and multiple sclerosis. Proc Soc Exp Biol Med 1997;216:21-27
[4] Langer-Gould A, Lucas R, Xiang AH, Chen LH, Wu J, Gonzalez E, Haraszti S, Smith JB, Quach H, Barcellos LF. Nutrients. 2018 Feb 27;10(3).
[5] Becklund BR, Severson KS, Vang SV, DeLuca HF. UV radiation suppresses experimental autoimmune encephalomyelitis independent of vitamin D production. Proc Natl Acad Sci U S A. 2010;107:6418-23.
[6] Wang Y, Marling SJ, Beaver EF, Severson KS, Deluca HF. UV light selectively inhibits spinal cord inflammation and demyelination in experimental autoimmune encephalomyelitis. Arch Biochem Biophys. 2015 1;567:75-82
[7] Wang Y, Marling SJ, Beaver EF, Severson KS, Deluca HF. UV light selectively inhibits spinal cord inflammation and demyelination in experimental autoimmune encephalomyelitis. Arch Biochem Biophys. 2015 1;567:75-82.
Marc Sorenson, EdD, for breast cancer prevention. 
While many doctors know that ultraviolet radiation (UVR) from sunlight reduces risk of breast cancer, they have missed something. UVR stimulates production of vitamin D in human skin. Therefore, many health professionals assume that vitamin D is responsible for the reduced cancer risk. This may lead them to advocate the use of vitamin D supplementation and totally miss the bigger picture. In addition to vitamin D, UVR from sunlight or sunlamps produces many supplementary healthful photoproducts. Among others, nitric oxide, serotonin, endorphin and BDNF are produced by sunlight, and these photoproducts are vital to health. And, it is likely that these healthful photoproducts lead to an inhibition of breast cancer.
New research shows that sun exposure per se is capable of reducing the risk of breast cancer.
Consequently, it should not surprise us that for breast cancer, sunlight’s effects go beyond vitamin D.[1] Researchers at Children’s Hospital Oakland Research Institute, used a murine model (mice) that easily develops breast cancer, and treated them with UVR. Much as we might expect, they found that UVR treatments produced significant anti-cancer effects. Furthermore, they found that neither dietary vitamin D nor topical vitamin D influenced cancer risk. Because of their findings, they stated the following: “UVR’s inhibitory effects occur irrespective of whether or not the treatment increases circulating D3 in the mice.” Also, they made one more important comment regarding their research on breast cancer and UVR. “Therefore, supplemental D3 may not mimic all possible beneficial effects of UVR, and uncovering non-D3-mediated mechanisms of UVR tumor inhibition may lead to novel strategies for cancer prevention.”
An important point about vitamin D, sunlight and breast cancer.
Finally, there is no doubt that vitamin D has anticancer benefits. This research however, is especially relevant in that it corroborates what I have said in my soon-to-be-released book, Embrace the Sun. First of all, we must not put all of the benefits of sunlight in the vitamin D box. Secondly, sun exposure performs myriad miracles beyond vitamin D. One of those miracles may be breast cancer prevention and inhibition. Thirdly, if we erroneously believe that we can obtain all of the sun’s benefits from popping a vitamin D pill, we may miss the holistic effects of the sun, which provide a cornucopia of salubrious results.
So, safely (without burning) embrace the sun and ease your mind about breast cancer.
[1] Anastasia M. Makarova, Flora Frascari, Parastoo Davari, Farzam Gorouhi, Philip Dutt, Lynn Wang, Akash Dhawan, Grace Wang, Jeffrey E. Green, Ervin H. Epstein, Jr. Ultraviolet radiation inhibits mammary carcinogenesis in an ER negative murine model by a mechanism independent of vitamin D3. Downloaded from cancerpreventionresearch.aacrjournals.org on April 12, 2018.
Marc Sorenson, EdD
What is IBD?
First of all, IBD consists of two primary diseases, ulcerative colitis (UC)  and Crohn’s disease (CD). UC is a chronic inflammatory condition characterized by relapsing and remitting episodes of inflammation limited to the mucosal layer of the colon.[1] Crohn’s disease, however, can involve any part of the gastrointestinal tract from the mouth to the anus. Yet, it most commonly affects the small intestine or the colon, or both.[2]
and Crohn’s disease (CD). UC is a chronic inflammatory condition characterized by relapsing and remitting episodes of inflammation limited to the mucosal layer of the colon.[1] Crohn’s disease, however, can involve any part of the gastrointestinal tract from the mouth to the anus. Yet, it most commonly affects the small intestine or the colon, or both.[2]
The gift of sunlight
First of all, there is a beautiful gift that may prevent or lessen IBD. The gift, (sunlight) awaits us, but if we do not accept the gift, we are no better off than if we didn’t have it. So it is in Italy, where those who suffer from IBD are shown to have far less sun exposure than those who do not have the disease.[3] Therefore, this may indicate that part of the cause of IBD is lack of sunlight. And in Italy, low sun exposure probably indicates a reluctance to step outside because, Italy is a sunny country. Maybe, many of the Italians who succumb to IBD, have obviously not accepted the gift. Either that, or they are using too much sunscreen, since sunscreen blocks the sun.
Furthermore, IBD patients are at an increased risk for fractures. Hence, one may conclude that both maladies may be due to low sun exposure.
Embrace the sun to prevent IBD
Another investigation, conducted over 12 years and involving hundreds of thousands of IBD patients produced remarkable outcomes. Hospitalizations for both UC and CD were far higher among those with low sun exposure.[4] And, the same relationship was shown between sun exposure, bowel surgeries and deaths: more surgeries were needed for those patients who experienced the lowest sun exposure. Also, more deaths occurred among those with low exposure.
And what about non-IBD patients?
Another side note to this investigation was the large number of non-IBD patients analyzed for sun exposure levels. It is most noteworthy that the same relationship existed as with the IBD patients. Low sun exposure associated with prolonged hospitalizations and more deaths when compared with high exposure. Especially relevant is other research involving the association of Crohn’s disease to surgery. It found that surgery for the disease was significantly reduced among patients who received more sun exposure.[5]
The north-south gradient
In addition, research shows that in the US, there is a north-south gradient for IBD risk.[6], [7], [8], [9] The risk of developing the disease is significantly lower in southern latitudes (because sun exposure is greater).
An important nutritional note about IBD:
In addition to what we have heretofore described, it is especially relevant to understand that IBD causes malabsorption of nutrients in the gut. Consequently, it leads to diseases of malnutrition.[10] And, vitamin D is one of the “nutrients” that may not be absorbed efficiently. Therefore, sun exposure (or sunlamps) may be the only viable source of vitamin D for a person with IBD.
Most of all, remember that non-burning sun exposure is essential to human health. It seems like a good idea to obtain your share, and protect your gut from IBD.
[1] Peppercorn M, Cheifetz, A, Rutgeerts P, Grover S. Definition, epidemiology, and risk factors in inflammatory bowel disease. http://www.uptodate.com/contents/definition-epidemiology-and-risk-factors-in-inflammatory-bowel-disease.
[2] Web MD http://www.webmd.com/ibd-crohns-disease/crohns-disease/inflammatory-bowel-syndrome.
[3] Vernia P, Burrelli Scotti G, Dei Giudici A, Chiappini A, Cannizzaro S, Afferri MT, de Carolis A. Inadequate sunlight exposure in patients with inflammatory bowel disease. J Dig Dis. 2018 Jan;19(1):8-14
[4] Limketkai BN, Bayless TM, Brant SR, Hutfless SM. Lower regional and temporal ultraviolet exposure is associated with increased rates and severity of inflammatory bowel disease hospitalization. Aliment Pharmacol Ther. 2014 Sep;40(5):508-17.
[5] Govani SM, Higgins PD, Stidham RW, Montain SJ, Waljee AK. Increased ultraviolet light exposure is associated with reduced risk of inpatient surgery among patients with Crohn’s disease. J Crohns Colitis. 2015 ;9(1):77-81
[6] Schultz M, Butt AG. Is the north to south gradient in inflammatory bowel disease a global phenomenon? Expert Rev Gastroenterol Hepatol. 2012 Aug;6(4):445-7.
[7] Kappelman MD, Rifas-Shiman SL, Kleinman K, Ollendorf D, Bousvaros A, Grand RJ, Finkelstein JA. The prevalence and geographic distribution of Crohn’s disease and ulcerative colitis in the United States. Clin Gastroenterol Hepatol. 2007 Dec;5(12):1424-9.
[8] Sonnenberg A. Similar geographic variations of mortality and hospitalization associated with IBD and Clostridium difficile colitis. Inflamm Bowel Dis. 2010 Mar;16(3):487-93.
[9] Holmes EA, Xiang F, Lucas RM. Variation in incidence of pediatric Crohn’s disease in relation to latitude and ambient ultraviolet radiation: a systematic review and analysis. Inflamm Bowel Dis. 2015 ;21(4):809-17
[10] Margulies SL, Kurian D, Elliott MS, Han Z. Vitamin D deficiency in patients with intestinal malabsorption syndromes–think in and outside the gut. J Dig Dis. 2015 Nov;16(11):617-33.
Health benefits of UV by Marc Sorenson, Ed.D.
How important is UV?  A transcendentally important scientific paper, by Dr. AT Slominski and colleagues, has added significant information about UV (sunlight) for skin. In addition, it explains the intricate connection between sunlight and the immune, endocrine and central nervous systems.[1] The name of the research paper, published in the journal Endocrinology, is How ultraviolet light touches the brain and endocrine system through skin, and why. The authors begin the abstract by stating that “the skin is a self-regulating protective barrier organ that is empowered with sensory and computing capabilities to counteract the environmental stressors to maintain/restore disrupted cutaneous homeostasis.” In other words, the skin has the ability to take on what life deals it and maintain its equilibrium and balance. In addition, the skin communicates bidirectionally with the central nervous, endocrine and immune systems. Thus, it helps to maintain balance for all body systems.
A transcendentally important scientific paper, by Dr. AT Slominski and colleagues, has added significant information about UV (sunlight) for skin. In addition, it explains the intricate connection between sunlight and the immune, endocrine and central nervous systems.[1] The name of the research paper, published in the journal Endocrinology, is How ultraviolet light touches the brain and endocrine system through skin, and why. The authors begin the abstract by stating that “the skin is a self-regulating protective barrier organ that is empowered with sensory and computing capabilities to counteract the environmental stressors to maintain/restore disrupted cutaneous homeostasis.” In other words, the skin has the ability to take on what life deals it and maintain its equilibrium and balance. In addition, the skin communicates bidirectionally with the central nervous, endocrine and immune systems. Thus, it helps to maintain balance for all body systems.
How does UV work?
First of all, ultraviolet energy (UV and UVB light) triggers all of these marvelous processes. UV, of course is available from sunlight, sunbeds or sunlamps. Its electromagnetic energy, through the skin, converts to chemical, hormonal and neural signals. These signals promote positive effects on the immune system, the endocrine system and the brain. Furthermore, endorphins (opioid-like substances) are increased and immune-system proteins are mobilized; consequently, health improves with UV. And, sun exposure regulates the endocrine system, by way of exposure to the skin, to produce or diminish hormones as needed. Especially relevant is that these effects take place independently of vitamin D synthesis.
Health increases with UV due to the magnificent sun, and our magnificent skin. As a result of the above information, it seems like it would be a good idea to soak up some non-burning sun each day when available. And, when it is not, we should find another UV source. In our soon-to-be-published book, Embrace the Sun, we discuss many facts about the healthful effects sun exposure:
A few healthful effects of sun (UV) exposure
- prevents and reverses obesity
- Improves longevity by reducing the risk of death by 50% over 20 years
- reduces the risk of hip fracture by 90% when compared to sun avoidance
- prevents the risk of breast cancer by 90% when compared to sun avoidance
- reduces by 50% the risk of melanoma in outdoor workers compared with indoor workers
- increases heart and vascular strength
- dramatically improves mood
- reduces the risk of multiple sclerosis
- reduces risk of most internal cancers
- cures psoriasis and eczema
- reduces risk of nervous system disorders
- prevents memory loss
- prevents myopia
The above list is not surprising in view of this new research, nor is the list complete. UV has many more healthful effects, which I’m sure the authors of this research acknowledge. Hence, the scientists sum up their research in this manner: “Thus, UV touches the brain and central neuroendocrine system to reset body homeostasis. This invites multiple therapeutic applications of UV radiation, for example in the management of autoimmune and mood disorders, addiction, and obesity.”
In conclusion, this seem like more compelling evidence to safely embrace the sun, no?
[1] Slominski AT, Zmijewski MA, Plonka PM, Szaflarski JP, Paus R. How ultraviolet light touches the brain and endocrine system through skin, and why. Endocrinology. 2018 Mar 12. [Epub ahead of print]
The superbugs are among us. Should we return to the use of sanatoria?
By Marc Sorenson, EdD
First of all, one should know that sanatoria are secluded hospitals. In addition, they usually specialize in healing through good food, fresh air and sunlight. Some scientists are now suggesting that we reestablish the use of sanatoria for healing.[1] They feel that sanatoria may be just the answer we seek for the prevention and healing of infectious diseases.
Interestingly, sanatoria were used effectively in the early 20th century (before antibiotics) and were really large outdoor solariums (sunrooms). These facilities allowed patients to be in natural surroundings, and in some cases, to expose themselves to direct sunlight. To demonstrate the efficacy of these facilities in curing tuberculosis (TB), consider the following history of Dr. Aguste Rollier:
Should we use sanatoria for healing TB?
First of all, records of 1,129 TB cases showed solariums cured 87% of “closed cases” and 76% of “open cases. “Among 158 patients with tuberculosis of the hip, 125 were cured and 102 “regained complete recovery of articular function.”[2] Dr. Rollier also had other successes. “During a time just following World War I, 1,746 of 2,167 tubercular patients under his care completely recovered. Furthermore, the only failures were among those who had allowed their tuberculosis to enter its most advanced stages.”[3]
Superbugs arrive from Peru.
In 2009, the first case of drug-resistant TB arrived in the US from Peru.[4] It was nearly 100% resistant to antibiotics. Consequently, it could cause an immense killer epidemic with the return of TB. There seems to be no answer to the “superbug” causing it. Or is there an answer? Could the sun provide a solution to this health threat? The superbugs are upon us like a bad horror movie. When they start to take over the earth, there will be few cures. But, UV light from the sun, or sun lamps, are remedies that still exist. Therefore, we would be well-advised to have our defenses set up in advance by enjoying daily sun exposure.
Another more recent historical perspective regarding sanatoria and sun exposure.
I recently happened across research that should be of interest to those who love the Sun. It gave a historical perspective of TB in the city of Bern, Switzerland. In addition, it showed how Bern wiped out most of its TB problems. Especially relevant is the fact that the city used lifestyle changes, not drugs. And, those changes included greater access to sun exposure.[5] The authors studied TB incidence during the period from 1856-1950. There were three areas of the city assessed for their historical TB problems. One was known as the Black Quarter, where during 1911-1915 there were 550 cases of TB per 100,000 people. The second was the City Center with 327 cases per 100,000 people. The third area was the Outskirts, with 209 cases per 100,000 people. There were three living conditions correlating closely to TB:
- The number of persons per room. A higher number predicted a greater risk of TB.
- A greater number of rooms without sunlight predicted a greater risk of TB.
- A greater number of windows per apartment predicted a diminished risk of TB
Consequently, the country worked to address these problems by reducing room crowding, providing open-air schools and building sanatoria. As a result, TB risk dropped from 330 cases per 100,000 in 1856 to 33 per 100,000 in 1950—a 90% drop! Also, I expect that health care cost dramatically decreased.
With the superbugs gaining strength each year, maybe we should reestablish the use of sanatoria?
Another thought: sun exposure probably works as well with many other diseases as it does with TB. Hence, the day may come when sanatoria, especially solariums, may be the only choice for curing infections. Finally, why not sunbathe daily in a non-burning fashion? In addition, sunlamps (in the absence of sunny days) could be valuable to the the health, because they also produce some of the same types of healing light (UVB and UBA) as the sun. Safely and regularly embrace the sun to protect your health!
[1] Greenhalgh I, Butler AR. Sanatoria revisited. Sunlight and health. J R Coll Physicians Edinb. 2017;47(3):276-280.
[2] Clark, W. Treatment of Bone and joint tuberculosis with Tuberculin and Heliotherapy. Journal of Bone and Joint Surgery 1923;5:721-39.
[3] Fielder, J. Heliotherapy: the principles & practice of sunbathing. Soil and Health Library (online) http://www.soilandhealth.org/index.html
[4] http://www.sphere.com/nation/article/first-case-of-highly-drug-resistant-tuberculosis-in-US/19294836?icid=main|htmlws-main-n|dl1|link3|http%3A%2F%2Fwww.sphere.com%2Fnation%2Farticle%2Ffirst-case-of-highly-drug-resistant-tuberculosis-in-US%2F19294836
[5] Zürcher K, Ballif M, Zwahlen M, Rieder HL, Egger M, Fenner L. Tuberculosis Mortality and Living Conditions in Bern, Switzerland, 1856-1950. PLoS One. 2016 16;11(2):e0149195
Two recent scientific analyses show that years of negative press about sunbeds has been misleading at best and mendacious at worst.
By Marc Sorenson, Ed.D.
After years of being told there is “no such thing as a safe tan”, new research is showing that exposure to sunbeds, those that mimic sunlight, may have been healthful all along. Many problems have existed with the research used to frighten the people away from sunlight and sunbeds. Two recent peer reviewed papers have exposed the lack of scientific accuracy by large organizations—organizations that appear to have pursued not the truth, but an agenda bent on discrediting the use of sunbeds. These disclosures were published in Anticancer Research, the Journal of the International Institute of Anticancer Research. The writers concluded that two reports, one by the World Health Organization (WHO) and a second European report called the SCHEER were unbalanced, biased and inaccurate. It is exceptionally important to understand that neither of these reports were peer reviewed. To me, this indicates that they were opinion pieces, not science. The authors of the first paper in the International Journal of Cancer Research and Treatment concluded their findings regarding the WHO and SCHEER thusly: “The stance taken by both agencies is not sufficiently supported by the data and in particular, current scientific knowledge does not support the conclusion sunbed use increases melanoma risk.” The authors of the second paper in the same Journal came to a similar conclusion after doing their analysis of the reports: “Current scientific knowledge is mainly based on observational studies with poor quality data, which report associations but do not prove causality. At present, there is no convincing evidence that moderate/responsible solarium [sunbed] use increases melanoma risk.” It’s almost as if the WHO and Scheer reports, with their twisted reasoning, were making a ridiculous argument, analogous to the following: Water causes drowning; swimming takes place in water; therefore, swimming causes drowning. None of this, of course, is meant to imply that humans should expose themselves to enough water to drown. Neither should they tan excessively. Tanning, like all other activities should be done in moderation, in other words, in a non-burning fashion.
Governments rely on research to advise the public regarding products and services. If there is a perceived risk, then they move forward with legislation to protect the consumer. But suppose that the researchers from WHO and SCHEER have already made up their minds on the risks and benefits of a product? The next step is to prove what they think they already know. That is not science! They accept every piece of research that might lend credence to their hypothesis, and they disregard or denigrate any research that disproves their hypothesis. They make sure that any benefits are removed or discredited. Of course, this allows them to form a conclusion that matches their hypothesis. This has happened with both sunlight and sunbeds. The concern about the risk of skin cancer has stopped agenda-driven “scientists” from even considering the remarkable benefits attributable to sunlight. This has given the world a biased and wholly unbalanced message.
An international group of 16 researchers headed by Professor Dr. Jörg Reichrath, Deputy Director of the Department of Dermatology, Venereology and Allergology at Saarland University Hospital in Homburg/Saar came together to review these reports that they believed to be unbalanced, biased, and full of confounders and inaccuracies. They also believe that the reports have downplayed the benefits of sunbed exposure.
Since most people don’t have the time to read the complete research paper, here are some interesting findings from the papers that I’d like to share with you. These are direct quotes from each paper:
Reichrath et al 2018
- In conclusion, both the SCHEER (1) and WHO (2) reports claim to assess health effects of sunbed use. Unfortunately, however, as such they are partially unbalanced and inaccurate. Both documents mainly assess negative health effects of UV exposure, conceal the large body of evidence demonstrating beneficial health effects of UV radiation, and major conclusions drawn are not sufficiently supported by current scientific knowledge. It should be emphasized that the main conclusions drawn by the SCHEER (1) and WHO (2) reports are not in accordance with generally accepted principles of evidence-based medicine, they not only are not in line with recommendations of the Oxford Centre for Evidence-based Medicine
- …the resulting evidence levels and grades of recommendation are not “strong”, as inaccurately stated in the SCHEER report (which used a highly questionable classification of evidence levels) (1), but are very weak (e.g. level 3a− for systematic reviews of case–control studies with heterogeneity, and grade of recommendation D for outcome “ever” vs. “never” use of a solarium). In conclusion, our present scientific knowledge does not support the notion that sunbed use per se may increase melanoma risk.
- It further underlines the unbalanced view of the SCHEER and WHO reports, that they conceal the large body of evidence demonstrating beneficial health effects of UV radiation.” And “The SCHEER and WHO reports do not adequately consider the large body of evidence demonstrating the negative health consequences of vitamin D deficiency.
- The most known and well-documented beneficial health effects of UV radiation are mediated via vitamin D. However, other factors might be involved, indicating that preventing and treating vitamin D deficiency may not account for all beneficial effects of solar or artificial UV exposure.”
- “Therefore, we rebut these conclusions by addressing the incomplete analysis of the adverse health effects of UV and sunbed exposure (what is‘safe’?) and the censored representation of beneficial effects, not only but especially from vitamin D production.
- While these reports were purportedly based on the best available scientific evidence, we are deeply concerned about their scientific quality and obvious lack of objectivity, most likely owing to an infusion with the laudable zeal to combat alarming increases in skin cancer. Both publications show an implicit tendency toward an unbalanced view and must be criticized because of many scientific misinterpretations and shortcomings.
- Several meta-analyses of poor quality consolidate the observational study data and compound the flaws of these studies.
- For example, dermatological phototherapy is often included when only sunbed use should be assessed [e.g. Landi et al.], and in many studies, subgroups of individuals with presumably high UV exposure in the past (e.g. individuals with history of ‘non-melanoma skin cancer’ or ‘dermatological conditions’) are excluded from controls but not cases (control selection bias).
- Additionally, it should be noted that studies available are characterized by high heterogeneity and by difficulties in adjusting for important confounding factors, including solar UV and lifestyle: only a minority of studies report odds ratios (ORs) adjusted for the same confounding factors, 12 studies not for a single confounder.
- Moreover, because individual confounders were assessed using different interrogations, these studies are only partly comparable limiting the ability to interpret results of a combined estimate. And these results should not be considered reliable (56).
- In this context, the same results and risk estimates as given in Boniol et al. (44) and
- Colantonio et al. could well be obtained in the following scenario, as indicated elsewhere. Sunbed use has no effect on melanoma risk, lifestyle factors such as extensive sunbathing in the summer as a sun worshipper or an ‘unhealthy lifestyle’ (e.g. alcohol, smoking use), do increase melanoma risk with true OR=1.2 (it has been reported previously that sun worshippers and individuals with an ‘unhealthy lifestyle’ go more frequently to tanning salons
- Many of the confounding factors, including extensive sunbathing in the summer and unhealthy lifestyle, have not been adequately and systematically considered in studies performed to date. For example, the comparison of sunbed users to non-users is confounded by their lifestyle habits, with typical sunbed users found to be females who tend to smoke cigarettes and drink alcohol more frequently than non-users, as well as eating less healthy food.
- Both the SCHEER and WHO reports underappreciate the large body of evidence from epidemiological and animal studies that demonstrates no increase in melanoma risk following chronic (moderate) UV exposure.
- Many other studies also support the concept that sub-erythemal exposure to UV doses not only does not increase melanoma risk, but may even be protective.
- It further underlines the unbalanced view of the SCHEER and WHO reports, that they conceal the large body of evidence demonstrating beneficial health effects of UV radiation.
- Moreover, epidemiological evidence provides support for solar UVB protection against a number of cancer types, including breast, colorectal, lung, ovarian, pancreatic and prostate cancer.
- Moreover, reductions of melanoma mortality rates during the past decades do not support the hypothesis that UV radiation from sunbeds may have increased melanoma risk.
- It has been suggested that better detection methods have been in use to detect melanoma earlier, which is also a possible reason for the increased risk that has been observed.
- Unfortunately, however, as such they are partially unbalanced and inaccurate. Both documents mainly assess negative health effects of UV exposure, conceal the large body of evidence demonstrating beneficial health effects of UV radiation, and major conclusions drawn are not sufficiently supported by current scientific knowledge.
- With this unscientific approach, both the SCHEER (1) and WHO (2) reports are not adequate and do not properly summarize current knowledge on comparing beneficial and adverse effects of UV exposure from sunbeds.
Burgard et al 2018
- “Moreover, in our opinion, the attempts of Boniol et al and others to attribute melanoma cases to solarium use are speculative and scientifically not sufficiently supported.”
- “As many as 35.5% (n=11) of all the included studies did not account for a single confounder.”
- Overall, quality of included studies was poor as a result of severe limitations, including possible recall and selection bias, and due to lack of interventional trials.
- However, for all outcomes analyzed, overall study quality and resulting levels of evidence (3a−) and grades of recommendation (D) were low due to lack of interventional studies and severe limitations including unobserved or unrecorded confounding.
- Many studies have investigated the impact of indoor tanning on melanoma risk (8-59), however, most of them have been criticized for limitations, unbalanced view, errors or incorrectness (11, 17). While some reports suggest that solarium use may increase melanoma risk (e.g. 19, 29, 32), other investigations found no or even a protective effect (e.g. 20-22, 24, 35).
- It should be emphasized that the results of these cohort and case–control studies represent associations and do not prove causality.
- According to the Oxford Centre for Evidence based Medicine, for the outcome ever-exposure to UV radiation from a solarium, we determined an evidence level of 3a− (systematic review of poor quality cohort and case–control studies) and a grade D of recommendation.
- As an example, incorrectness in one of the main findings of the study of Boniol et al. (8) forced the authors to publish a correction (16). As Colantonio et al. point out, comparison of five previously published systematic reviews on this topic demonstrates an alarming tendency for copying data without referencing the original article, and without checking for errors (11).
- As an example, the influential review of the IARC Working group published in 2007 (10) has been criticized for numerous errors in content and typography [e.g. giving wrong numbers for the controls reported 1989 by MacKie et al. (38) and 1981 from Adam et al. (19)], which are also present in two subsequent reviews (11). Furthermore, the numbers of participants from several included studies (31, 43) published in the IARC review could not be derived by us and others (11) from the original articles.
- Moreover, in our opinion, the attempts of Boniol et al. (8) and others (12) to attribute melanoma cases to solarium use are speculative and scientifically not sufficiently supported.
- For recruitment before 1991, a higher OR [increased risk] was found as compared with recruitment from 1991-1999 or since 2000.
- Moreover, both the resulting level of evidence and grade of recommendation of studies investigating the association of melanoma risk with solarium use are weak.
- In summary, our review has highlighted the poor quality of the evidence available at present on this topic. We conclude that (i) results of our and previously published meta-analyses most likely overestimated the association of melanoma risk with solarium use, (ii) both the level of evidence and grade of recommendation of studies published previously investigating the association of melanoma risk with solarium use are weak, and therefore (iii) present scientific knowledge does not support the hypothesis of an increased melanoma risk due to solarium use, and questions studies that try to attribute melanoma cases to indoor tanning, and does not support initiatives that aim to ban responsible/moderate solarium use for tanning purposes.
Sadly, some “science” follows the paths of deception. Many writers have let a bias toward a particular outcome color their judgement and even misinterpret their results. You can find many examples of bad science by doing an internet search for that term. Because a result was printed in a scientific journal, or stated by a multinational organization, it does not necessarily denote truth.
As you can see, the 2 reports on sunbeds have concluded that sunbeds were dangerous and would lead to cancer. The research compiled to reach this conclusion was of poor quality and biased. It also left out relevant information—information that would have completely changed the result. Obviously, these results were born of a need to produce the result they wanted, not a need to find the truth.
The statement, that there is no need to use sunbeds, as there are no health benefits, is an egregious misstatement of the facts. Here are several citations that belie the idea that there are no health benefits of sunbed use:
- Vitamin D production and bone strength.
In a study comparing 50 subjects who used a sunbed at least once a week to 106 control subjects who did not use sunbeds, it was shown that tanning-bed users had 90% higher 25(OH)D levels than non-users, and that they also had significantly higher bone-mineral density, indicative of stronger bones.[1] Another study showed that whereas a daily 400 IU vitamin D supplement did not maintain healthful 25(OH)D levels, sunbed use increased 25(OH)D levels by 150% in only seven weeks.[2]
- Sunbeds can control psoriasis and eczema.
They are often recommended by dermatologists as a way to overcome these diseases. Scientists have stated that UV light is nearly 100% effective for many dermatologic conditions, and that sunbeds are very convenient sources of UV rays for patients who cannot otherwise afford the rigorous travel and time commitments necessary to visit the dermatologist.[3] This was the conclusion they reached: “Unsupervised sun exposure is a standard recommendation for some patients to obtain phototherapy. Selected use of commercial sunbeds in the treatment of dermatologic conditions may be another useful and effective treatment for those patients with an inability to access office-based or home-based phototherapy.”
- Sunbed use reduces chronic pain.
A study of pain in fibromyalgia patients, conducted by dermatologists, revealed that those who used UV-producing sunbeds experienced a decrease of 0.44 points on a 10 point scale (Likert scale) determined by subject questionnaire, when compared to those who did not receive UV light.[4], [5]
- Sunbeds may reduce endometrial cancer. Research from Sweden demonstrated that women who use sunbeds more than three times yearly had a 40-50% reduction of the risk for endometrial cancer.[6] The authors surmised that the effects observed were likely due to stimulating higher 25(OH)D levels in winter.
- Sunbed use reduces the risk of clots. In an eleven-year study of the sun-exposure habits of 40,000 women, venous thrombotic (clotting) events were measured. It was found that women who sunbathed during the summer, on winter vacations, or when abroad, or used a sunbed, had a 30% decrease in the risk of clots compared to those who did not sunbathe.[7] The authors again speculated that increased vitamin D, which has anticoagulant properties, had provided these positive results.
- Sunbed use is associated with lower breast-cancer risk.[8]
- Perhaps the most important research on sunbeds was a 20-year study in Sweden by Dr. Pelle Lindqvist and his colleagues, who showed that women who used sunbeds were 23% less likely to die from any cause than women who did not use them.[9] This research also showed that low sun exposure as a risk factor for all-cause death was comparable in magnitude to smoking, and women with active sun exposure habits were found to live 1 to 2 years longer as compared to those with the lowest sun exposure habits.
I couldn’t agree more with the latest research.
[1] Tangpricha V, Turner A, Spina C, Decastro S, Chen TC, Holick MF. Tanning is associated with optimal vitamin D status (serum 25-hydroxyvitamin D concentration) and higher bone mineral density. Am J Clin Nutr 2004;80:1645-49.
[2] Holick, M. Boston University. “Effects Of Vitamin D And Skin’s Physiology Examined.” Science Daily 21 February 2008 <http://www.sciencedaily.com¬ /releases/2008/02/080220161707.htm>.
[3] Radack KP, Farhangian ME, Anderson KL, Feldman SR. A review of the use of tanning beds as a dermatological treatment. Dermatol Ther (Heidelb). 2015 Mar;5(1):37-51.
[4] Kaur M, Feldman SR, Liguori A, Fleischer AB Jr. Indoor tanning relieves pain. Photodermatol Photoimmunol Photomed. 2005 Oct;21(5):278.
[5] Taylor SL, Kaur M, LoSicco K, Willard J, Camacho F, O’Rourke KS, Feldman SR. Pilot study of the effect of ultraviolet light on pain and mood in fibromyalgia syndrome. J Altern Complement Med. 2009 Jan;15(1):15-23.
[6] Epstein E, Lindqvist PG, Geppert B, Olsson H. A population-based cohort study on sun habits and endometrial cancer.Br J Cancer. 2009 Aug 4;101(3):537-40.
[7] Lindqvist PG, Epstein E, Olsson H. Does an active sun exposure habit lower the risk of venous thrombotic events? A D-lightful hypothesis. J Thromb Haemost. 2009 Apr;7(4):605-10.
[8] Yang L, Veierød MB, Löf M, Sandin S, Adami HO, Weiderpass E. Prospective study of UV exposure and cancer incidence among Swedish women. J Intern Med. 2014 Jul;276(1):77-86
[9] Lindqvist PG, Epstein E, Landin-Olsson M, Ingvar C, Nielsen K, Stenbeck M, Olsson H. Avoidance of sun exposure is a risk factor for all-cause mortality: results from the Melanoma in Southern Sweden cohort. J Intern Med. 2014 Jul;276(1):77-86.
 UVB is a spectrum of sunlight with many effects. These include the suppression of inflammation in the skin. It has been used to very successfully treat skin diseases such as psoriasis and eczema.
UVB is a spectrum of sunlight with many effects. These include the suppression of inflammation in the skin. It has been used to very successfully treat skin diseases such as psoriasis and eczema.
Since inflammation is necessary to produce the condition of atherosclerosis (plugging of the arteries). It would be interesting to know whether UVB might also have the same anti-inflammatory effects in the arteries. If so, the effect could inhibit or eliminate atherosclerosis, and thus provide an entirely new treatment for heart disease. It would also protect against vascular events such as stroke and intermittent claudication.
The idea that UVB could prevent atherosclerosis by reducing inflammation in arteries was recently studied by Japanese researchers.[i] Using a mouse model, they demonstrated that UVB light irradiation, applied once a week for 14 weeks, leads to an increase in the action of T-regulatory cells, thereby inhibiting inflammation. In addition, exposure reduced the production of another type of T-cell which is pro-inflammatory and thereby pro-atherogenic (leading to the production of atherosclerosis). These two effects of UVB light reduce the development and progression of atherosclerosis.
Stated differently, the research shows that sun exposure is a critically-important therapy to reduce and prevent diseases of the heart and blood vessels. Protect your heart by being sure to obtain sufficient non-burning sunlight from sun exposure or other sources such as sun lamps. It is also important to note that neither skin cancer nor skin inflammation were observed following UVB exposure in this breakthrough study, which again emphasizes the importance of sun exposure for human health.
If these findings are true, then we would expect that there would be fewer cardiovascular events such as heart attacks and strokes during times of less sun exposure. Accordingly, Research has demonstrated that those below the median level of serum vitamin D suffer 57% more heart attacks than those whose levels were above the median[i] (low vitamin D levels are a surrogate for sun exposure). They also noted that the greatest number of heart attacks occurred in winter and early spring. These seasons, of course, are the times of lowest sun exposure. And, according to what we have learned, they are also the times of greatest inflammation.
Let there be light, and safely apply it to your skin. Be sure not to burn.
[i] Scragg R, Jackson R, Holdaway IM, Lim T, Beaglehole R. Myocardial infarction is inversely associated with plasma 25-hydroxyvitamin D3 levels: a community-based study. Int J Epidemiol 1990;19:559-63.
[i] Sasaki N, Yamashita T, Kasahara K, Fukunaga A, Yamaguchi T, et al. UVB Exposure Prevents Atherosclerosis by Regulating Immunoinflammatory Responses. Arterioscler Thromb Vasc Biol. 2016;36:00-00