Sunlight improves public health. By Marc Sorenson, EdD.
Sunlight improves public health. By Marc Sorenson, EdD.
An excellent new paper by Dr. Hoel and Dr. de Gruijl is titled “Sun Exposure Public Health Directives.” It decries the vilification of sunlight and suggests people return to its healthful rays.[1] https://www.mdpi.com/1660-4601/15/12/2794/htm
So is dermatology awakening to the truth about sunlight?
And one of the authors, Dr. de Gruijl, works at a dermatology department in the Netherlands. He is also a photobiologist and melanoma skin cancer research specialist. It seems like the dermatology world is returning to common sense, since other dermatologists have lately suggested more sunlight exposure. And well they should suggest more sunlight! Sunlight can save millions of lives, yet much of the population is dying in the dark due to misinformation. Many dermatologists consider sunlight exposure to be a killer, and thus frighten their patients away from sun exposure. Why? Because they are fearful of skin damage from sunlight, something they need not fear if they advise their patients properly.
Sunlight and skin cancer: the truth
One of my pet peeves is the statement that “sunlight causes cancer.” First of all, there are about 18 major cancers that are reduced by sunlight. And in addition, there are also myriad non-cancer maladies that are reduced or eliminated by safe sun exposure. These disorders run the gamut from arthritis and heart disease to psoriasis, erectile dysfunction and osteoporosis.[2] Secondly, not even skin cancer is caused by sun exposure unless people burn themselves. Therefore, it is a lack of both caution and common sense that leads to skin damage. The authors state that the public has been taught that health benefits of sun exposure are limited to bone health. That is another egregious error (italics mine).
The aforementioned paper reads almost like a synopsis of Embrace the Sun, the book by Marc Sorenson and William Grant,
Here are the major points on sunlight that make the research in the paper so compelling:
- There is a public health message that “overexposure” to the sun causes skin cancer. Nevertheless, those who promote this message do not define overexposure. Therefore, due to the lack of a definition, the public is led to believe that sun exposure is an enemy. In addition, the public is not educated regarding the detriments of “sun avoidance,” or should we say “underexposure.” Due to this omission, the public is exposed to disability, destruction and death (italics mine).
Sunlight deprivation: the staggering cost to human health
Consequently, in Embrace the Sun, we calculated the number of deaths due to diseases associated with high sunlight exposure. And, we then calculated the number of deaths due to diseases associated with sunlight deprivation. As a result, we determined that approximately 1,684,677 yearly deaths are caused by diseases associated with sunlight deprivation. Also, there were about 5125 deaths from diseases associated with high sunlight exposure, producing a ratio of approximately 328.7:1. This is most noteworthy! 328 deaths were associated with diseases of sun deprivation for each death associated with diseases of sun exposure. So, what do you think?
So, is sunlight avoidance risk free?
- Furthermore, the paper states that people believe sun avoidance is risk free. That is a colossal error as previously stated,
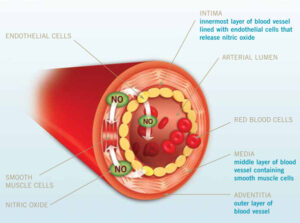
- Another mistake is to believe vitamin D supplements are an adequate substitute for sunlight. That is simply not so. Sun exposure causes the production of serotonin, nitric oxide, endorphin, brain-derived neurotropic factor (BDNF), dopamine and urocanic acid. All of these substances are vital for human health and wellbeing.
- Another important point stated by the authors is as follows: “This public health message is potentially causing significant harm to public health and should be changed immediately.” And, based on the analysis from Embrace the Sun, mentioned above, that should be an easy conclusion.
Is there an inverse association between sunlight and melanoma?
- The authors also state that melanoma risk is reduced by non-burning sun exposure. And only severe sunburns increase risk. In addition, they mention that melanoma in the U.S. has steadily increased at an annual rate of 3–4%. There was 1 case per 100,000 in 1935, when accurate records were established. Yet, there were 25.8 cases per 100,000 in 2015. [That is about a 2,600% increase!]
Our analysis of melanoma in Embrace the Sun was almost identical. It showed a 3,000% increase in melanoma risk accompanied by a 90% decrease in sunlight exposure from 1935 to 2015. And, Sunscreen use also increased dramatically during that period, meaning that more sunscreen use is associated with greater melanoma risk.
And should we use sunscreens to reduce sunlight damage?
The answer to that question is “of course not.”
I was surprised that nothing was said about sunscreens, while I was considering the authors’ comment on severe sunburns, Why? Because recent research has shown that persons who use sunscreens have 4-6 times greater risk of sunburn.[3] In addition, the same research showed that the greatest protection against burning was to seek shade or cover up. Imagine that! Also, a recent meta-analysis showed that sunscreen use made absolutely no difference in the risk of skin cancer.[4].
- The authors also make it clear that the common assertion—that tanned skin affords insignificant protection against sunburn—is not correct.
- In conclusion, the commentary made this statement: “All persons in the world regardless of skin color or latitude of residence, other than those with extraordinary sensitivity to sunlight, should get enough sun exposure to maintain a serum 25(OH)D level well over 20 ng/mL (desirably at 30–60 ng/mL) while taking care to avoid sunburn.
I agree and would like to reiterate that vitamin D supplements are not an adequate substitute for sunlight. Consequently, these measurements should be used only among those who do not take supplements. That is, if we expect to really measure sunlight exposure.
Embrace the Sun is available here. 
Happy sunning!
[1] Hoel D, de Gruijl, F. Sun Exposure Public Health Directives. Int. J. Environ. Res. Public Health 2018;15:2794
[2] Sorenson, Marc, Grant, WB. Embrace the Sun. Sorenson, Publisher 2018. Available at Amazon.
[3] Kasey L. Morris, PhD; Frank M. Perna, EdD, PhD. Decision Tree Model vs Traditional Measures to Identify Patterns of Sun-Protective Behaviors and Sun Sensitivity Associated With Sunburn. JAMA Dermatol. Published online June 27, 2018.
[4] Elizabet saes da SILVA, Roberto TAVARES, Felipe da silva PAULITSCH, Linjie ZHANG. Eur J Dermatol 2018; 28(2): 186-201.