A review published in the journal Nutrients discusses a great deal of research that indicates vitamin D provides protection against internal infection.[1] It regulates both innate (inborn, quick acting, short lived) immunity and acquired (promoted by response to an invasive organism and producing a long-lasting effect) immunity. 
The researchers extoll the virtues of vitamin D in increasing the strength of both forms of immunity, and state that vitamin D deficiency is associated with an increased risk for various infections, including HIV, respiratory tract and HCV infection. However, when discussing the efficacy of vitamin D supplementation, they state that “robust data from controlled trials investigating the use of vitamin D as a preventive or therapeutic agent are missing.”
Unfortunately, the researchers indicate that sun exposure would be a good way to obtain vitamin D in correct amounts, but then destroy that argument by stating that …”UVB radiation is also the main cause of human skin cancer, thus it is difficult, if not impossible, to make a general recommendation to expose the skin to the sun for sufficient vitamin D synthesis.”
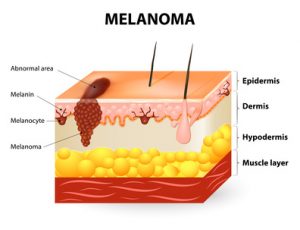
They are wrong, of course. Common skin cancers cause very few deaths, and melanoma, the deadly cancer, is far less common in people who are regularly exposed to sunlight, compared to those who avoid the sun. Outdoor workers have about half the risk of contracting melanoma as do indoor workers.[2]
Another problem that the researchers have with sun exposure as a vitamin D source is this: People who live at high latitudes do not produce any vitamin D from sun exposure in the winter, because there is no UVB light at that time of year. My response to this is the following: Use UVB lamps or sunbeds. Such a suggestion would probably cause the authors of this researchers to melt down. I can hear them screaming “melanoma!” already. I would then direct them to a 20-year study from Sweden, which showed that women who used sunbeds during that 20 years had a 23% reduction in all-cause death risk compared to those who avoided sunbeds.[3] And, they were not at increased risk of melanoma. Also, the subjects in the study who avoided sun exposure were twice as likely to die of any cause compared to those who had the highest sun exposure.
At almost any place on earth, we now have either the sunshine or UVB lamps that can give us the vitamin D we need and the other photoproducts that protect us from myriad diseases, including various infections. It is a shame that too many fail to take advantage.
[1] Juliana de Castro Kroner, Andrea Sommer and Mario Fabri. Vitamin D Every Day to Keep the Infection Away? Nutrients 2015, 7, 4170-4188.
[2] Godar D, Landry, R, Lucas, A. Increased UVA exposures and decreased cutaneous Vitamin D3 levels may be responsible for the increasing incidence of melanoma. Med Hypotheses 2009;72(4):434-43.
[3] Pelle G. Lindqvist, Elisabeth Epstein, Mona Landin-Olsson, Christian Ingvar, Kari Nielsen, Magnus Stenbeck & Håkan Olsson. Avoidance of sun exposure is a risk factor for all-cause mortality: results from the Melanoma in Southern Sweden cohort. J Intern Med. 2014 Jul;276(1):77-86.
 Some time ago I wrote a blog on sun exposure and depression, emphasizing the importance of a protein called brain derived neurotropic factor (BDNF). This is an update.
Some time ago I wrote a blog on sun exposure and depression, emphasizing the importance of a protein called brain derived neurotropic factor (BDNF). This is an update.
BDNF is a factor in nerve growth and maturation, and is essential in synapse formation and plasticity. A lack of of it is implicated in psychiatric disorders such as schizophrenia, intellectual disability, autism and depression. Interestingly, it has been shown that unless there is sufficient BDNF in the brain, conventional antidepressants do not work very well,[1] and when BDNF is infused directly into the brains of rodents, it produces an antidepressant effect.[2]
It has also been shown that BDNF has a seasonal variation in concentration correlating with the amount of ambient sun; it increases in the spring and summer and decreases in fall and winter. [3] The authors of this research described the importance of their findings thusly: “This finding is important for our understanding of those factors regulating BDNF expression and may provide novel avenues to understand seasonal dependent changes in behavior and illness such as depression.”
BDNF has been shown to increase significantly after bright light exposure,[4] and in what we would consider to be a remarkably important study, both light exposure and treadmill exercise increased its expression of
in rats,[5] or as the researchers showed, exercise and/or bright light promoted neurogenesis (new nerve cell growth) in the adult rat brain. How important is this finding for adults who are worried about cognitive decline? We are actually seeing an example of new brain cells being built by bright light and exercise. What a wonderful way to help prevent Alzheimer’s disease and maintain mental sharpness into old age! Don’t forget your (safe) sunlight!
[1] Björkholma C, Monteggiab, L. BDNF — a key transducer of antidepressant effects. Neuropharmacology. 2016 March ; 102: 72–79.
[2] Siuciak JA, Lewis DR, Wiegand SJ, Lindsay RM. Antidepressant-like effect of brain-derived neurotrophic factor (BDNF). Pharmacol. Biochem. Behav. 1997; 56(1):131–137.
[3] Molendijk ML, Haffmans JP, Bus BA, Spinhoven P, Penninx BW, Prickaerts J, Oude Voshaar RC, Elzinga BM. Serum BDNF concentrations show strong seasonal variation and correlations with the amount of ambient sun. PLoS One. 2012;7(11):e48046.
[4] Tirassa P1, Iannitelli A, Sornelli F, Cirulli F, Mazza M, Calza A, Alleva E, Branchi I, Aloe L, Bersani G, Pacitti F. Daily serum and salivary BDNF levels correlate with morning-evening personality type in women and are affected by light therapy. Riv Psichiatr. 2012 Nov-Dec;47(6):527-34.
[5] Kwon SJ, Park J, Park SY, Song KS, Jung ST, Jung SB, Park IR, Choi WS, Kwon SO. Low-intensity treadmill exercise and/or bright light promote neurogenesis in adult rat brain. Neural Regen Res. 2013 Apr 5;8(10):922-9.
I have written several blogs making this melanoma case: not only is this deadly cancer not caused by sun exposure, but habitual, or regular, sun exposure has a protective effect against the disease. This blog will serve to reinforce and review the reasoning behind those conclusions.
A friend sent me a scientific paper[1] that I had forgotten or missed—a paper by Dr. Veronique Bataille that brought out several supportive points about how sun exposure protects against the disease. Here are a few of the salient ideas from the paper:
- The increase in melanoma is mostly seen for the thin types, which can’t be attributed to sun exposure but to increasing screening over the last 20 years. The fact is, that incidence appears to increase as the number of dermatologists and public health campaigns also increase. But the increase in melanoma is not real. This idea is perfectly plausible; when more dermatologists are available, and the public is driven to them by health campaigns more melanomas are found. Many “first-stage” or thin “thin” melanomas are discovered and counted that would not have been found in previous decades. This causes numbers to be highly inflated compared to the days when there were fewer dermatologists and fewer public health campaigns.
Comment: Another fact was not mentioned in the paper: Stunningly, a worldwide study of melanoma diagnosis and accuracy, published in the American Academy of Dermatology (AAD) showed that most diagnoses were incorrect.[2] Approximately 44 different authors from many different clinics and countries, including the US, contributed to the report. They made an accuracy-in-detection analysis based on the actual number of melanomas that were excised during a period of ten years, compared with the number that really needed to be excised. Many clinics in different countries were involved in assessing the numbers. The AAD research showed that only about 3.5% of diagnoses in non-specialized clinics, and 14.7% in specialized clinics, resulted in actually being melanoma. From this information, it is evident that many melanoma surgeries are bogus and may inflate the incidence of this deadly skin cacner.
What do we take away from this? There may be no real increase in melanoma, only an increase in assessment and excision.
- Low vitamin D levels are common in melanoma patients and have a deleterious effect on their risk and survival.
Comment: Low vitamin D levels are caused by sunlight deprivation; we are told to avoid the sun, but sun avoidance leads to vitamin D deficiency, which further leads to melanoma. If our population regularly enjoyed non-burning sun exposure, vitamin D levels would be much higher and the risk of melanoma much lower. This is corroborated by the fact that people who habitually work outdoors have a far lower risk of the disease. Dr. Cedric Garland and his colleagues showed that those who worked indoors had a 50% greater risk of than those who worked both indoors and outdoors.[3]
- An excess of naevi (moles), not sun exposure, is the strongest risk factor for melanoma, and when comparing the risk created by sunburns and fair skin to the risk created by an excess of moles, the moles create a 15-30 times higher risk.
Comment: Some very important research by Dr. Adele Green found that the strongest risk factor for both limb melanoma and trunk melanoma was the presence of more than 10 moles on the arm, which predicted a 42-times increased risk. [4] This means that public health campaigns should promote mole awareness! Unfortunately, they promote sun avoidance, which increases the risk of melanoma.
- Attempts to decrease melanoma incidence and mortality, by reducing sun exposure, has not been proven to work and may be harmful.
Comment: the statement is obviously true. In the U.S., Sun exposure has decreased by about 90% since 1935. During that same period, melanoma has increased by 3,000%.[5] Data from the Bureau of Labor statistics showed that indoor occupations such as “professional, managerial, clerical, sales, and service workers (except private household service workers) grew from one-quarter to three-quarters of total employment between 1910 and 2000.” The BLS also stated, during the same period, the outdoor occupation of farming declined by 96% from 33% to 1.2% of total employment. The data also show approximately 66% of the decline in the occupation of farmers and 50% of the decline in the occupation of farm laborers occurred after 1935.
Further information, this time from the Environmental Protection Agency (EPA) determined as of 1986, about 5 percent of adult men worked mostly outside, and about 10 percent worked outside part of the time. The proportion of women who worked outside was thought to be even lower.[6] These data demonstrate a dramatic shift from outdoor, sun-exposed activity to indoor, non-sun-exposed activity during the mid-to-late 20th Century. This change, nonetheless, has been accompanied by a 30-times increase in risk since 1935, the MIF-baseline year.
- Photoageing, which is skin ageing due to sunlight exposure, is not greater in melanoma patients than patients who do not have the disease. In fact, patients with the cancer exhibit less photoageing than those who do not have the disease.
Comment: This was a new research for me and it belied the idea that sun exposure caused melanoma. If sun exposure causes skin photoageing, and there is less photoageing on cancer sites, sun exposure cannot possibly be causing melanoma. Enough said.
We need our sunshine, and one of the reasons for that need is to prevent deadly cancers.
[1] Bataille V. Melanoma. Shall we move away from the sun and focus more on embryogenesis, body weight and longevity? Medical Hypotheses 81 (2013) 846–850.
[2] Argenziano G, Cerroni L, Zalaudek I, Staibano S, Hofmann-Wellenhof R, et al. Accuracy in melanoma detection: a 10-year multicenter survey.J Am Acad Dermatol. 2012 Jul;67(1):54-9.
[3] Garland FC, White MR, Garland CF, Shaw E, Gorham ED. Occupational sunlight exposure and melanoma in the U.S. Navy. Arch Environ Health. 1990 Sep-Oct;45(5):261-7.
[4] Green AC, Siskind V. Risk factors for limb melanomas compared with trunk melanomas in Queensland. Melanoma Res. 2012 Feb;22(1):86-91.
[5] Melanoma International Foundation, 2007 Facts about melanoma. Sources: National Cancer Institute 2007 SEER Database, American Cancer Society’s 2007 Facts and Figures, The Skin Cancer Foundation, The American Academy of Dermatology.
[6] US Congress, Office of Technology Assessment, Catching Our Breath: Next Steps for Reducing Urban Ozone, OTA-O-412 (Washington, DC: US Government Printing Office, July 1989).
 Ovarian cancer, like most cancers, is nothing to trifle with. There are 22,280 new cases of ovarian cancer and 14,240 deaths annually in the U.S.[1] Compare that death statistic to melanoma, which has a death rate of only 9,730.[2] (And I might mention that people who are regularly in the sun have a reduced risk of melanoma.) But are there any indications that ovarian cancer is reduced by sun exposure? Yes. The National Cancer Institute’s Cancer Mortality Map also shows that ovarian cancers are much less common in sunnier Southern and Southwestern States than in the North and Northeast,[3] indicating a protective effect of sun exposure.
Ovarian cancer, like most cancers, is nothing to trifle with. There are 22,280 new cases of ovarian cancer and 14,240 deaths annually in the U.S.[1] Compare that death statistic to melanoma, which has a death rate of only 9,730.[2] (And I might mention that people who are regularly in the sun have a reduced risk of melanoma.) But are there any indications that ovarian cancer is reduced by sun exposure? Yes. The National Cancer Institute’s Cancer Mortality Map also shows that ovarian cancers are much less common in sunnier Southern and Southwestern States than in the North and Northeast,[3] indicating a protective effect of sun exposure.
Research has also demonstrated a relationship between high sun exposure and low risk of ovarian cancer. For example, an Australian investigation showed that women in the highest third of sun exposure, over a lifetime, had a 30% reduced risk of all endothelial ovarian cancers, a 53% reduced risk of borderline tumors and 22% reduced risk of invasive tumors.[4] And, in one piece of research using the Nurses’ Health Study ll, sun exposure was associated with a 33% reduced risk of ovarian cancer.[5] Ovarian cancer mortality rates were also found to be strongly inversely correlated with solar UVB doses in an ecological study by Drs. William Grant and Cedrick Garland.[6]
Sun avoidance is one of the most deadly practices ever perpetrated on the public. Women, carefully embrace the sun and reduce your risk of this potentially deadly disease.
[1] Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016 Jan;66(1):7-30.
[2] American Cancer society statistics, 2017.
[3] Grant, W B. Information available at SUNARC.org, and at the National Cancer Institute’s Cancer Mortality Maps and Graphs.
[4] Tran B, Jordan SJ, Lucas R, Webb PM, Neale R; Australian Ovarian Cancer Study Group. Association between ambient ultraviolet radiation and risk of epithelial ovarian cancer. Cancer Prev Res (Phila). 2012 Nov;5(11):1330-6.
[5] Prescott J, Bertrand K, Poole E, Rosner B, Tworoger S. Surrogates of Long-Term Vitamin D Exposure and Ovarian Cancer Risk in Two Prospective Cohort Studies. Cancers 2013, 5, 1577-1600;
[6] Grant WB, Garland CF. The association of solar ultraviolet B (UVB) with reducing risk of cancer: multifactorial ecologic analysis of geographic variation in age-adjusted cancer mortality rates. Anticancer Res. 2006 Jul-Aug;26(4A):2687-99.
Hypertension, or chronic high blood pressure, is determined by the amount of blood the heart pumps and the amount of resistance to blood flow in the arteries. The more blood the heart pumps and the tighter the arteries, the higher the blood pressure.[1] The top number on a blood-pressure measurement, stated in millimeters of mercury (mm/Hg), is called systolic pressure, and the lower number is called diastolic pressure. Hypertension is defined as having a blood pressure > 140/90 mm/Hg.  Thirty-one percent of US adults are hypertensive.[2] Hypertension can damage arterial walls and can eventually lead to an increased risk of death from heart disease, heart failure, and other arterial diseases. It is also associated to a higher risk of kidney disease, irregular heart rhythms, osteoporosis, cognitive dysfunction, painful intercourse and stroke.[3] Conventional textbook theory holds that blood pressure is regulated by the brain, blood vessels, or kidney, but recent evidence suggests it could be regulated in the skin, and sun exposure plays a role in controlling hypertension.[4]
Thirty-one percent of US adults are hypertensive.[2] Hypertension can damage arterial walls and can eventually lead to an increased risk of death from heart disease, heart failure, and other arterial diseases. It is also associated to a higher risk of kidney disease, irregular heart rhythms, osteoporosis, cognitive dysfunction, painful intercourse and stroke.[3] Conventional textbook theory holds that blood pressure is regulated by the brain, blood vessels, or kidney, but recent evidence suggests it could be regulated in the skin, and sun exposure plays a role in controlling hypertension.[4]
One of the earlier studies of hypertension and sun showed hypertension increased linearly at increasing distances from the equator.[5] One study of hypertensive subjects shows that blood pressure levels average 165/90 in winter but 134/74 in the summer, and both stroke and heart attack rates double in the winter.[6] Even in children, blood pressure is higher in winter than summer.[7] This, of course, is indicative of a protective role of sun exposure on hypertension.
UVB light treatments with sun lamps have also been shown to substantially lower blood pressure in 24 hours, and over six weeks to raise serum 25(OH)D levels of vitamin D by 162%, while lowering both systolic and diastolic pressure by six points.[8]
However, it is important to again mention that there is another important player in the relationship between hypertension and sun. Ultraviolet A (UVA) light (part of sunlight) stimulation of the skin causes the release of nitric oxide (NO) from pre-formed stores of NO in the skin. NO is a potent vasodilator, and when released into the arteries by UVA stimulation, causes increased blood flow and lowered blood pressure.[9], [10]
Safe sun exposure, along with plenty of vegetable and fruit consumption, may enable you to say goodbye to blood-pressure problems.
[1] Mayo Clinic Diseases and Conditions: High blood pressure (hypertension). http://www.mayoclinic.org/diseases-conditions/high-blood-pressure/basics/definition/con-20019580 (accessed January 5, 2016).
[2] Fields LE, Burt VL, Cutler JA, Hughes J, RoccellaEJ, Sorlie P. The burden of adult hypertension in the United States 1999–2000: a rising tide. Hypertension. 2004;44:398–404.
[3] Ann Pietrangelo. Healthline 2014 http://www.healthline.com/health/high-blood-pressure-hypertension/effect-on-body (accessed January 4, 2016).
[4] Johnson RS, Titze J, Weller R. Cutaneous control of blood pressure. Curr Opin Nephrol Hypertens. 2016;Jan25(1):11-5.
[5] Rostand SG. Ultraviolet light may contribute to geographic and racial blood pressure differences. Hypertension. 1997 Aug;30(2 Pt 1):150-6.
[6] Charach G, Rabinovich PD, Weintraub M. Seasonal changes in blood pressure and frequency of related complications in elderly Israeli patients with essential hypertension. Gerontology. 2004 Sep-Oct;50(5):315-21
[7] Polat M, Akil I, Yuksel H, Coskun S, Yilmaz D, Erguder I, Onag A. The Effect of seasonal changes on blood pressure and urine specific gravity in children living in Mediterranean climate. Med Sci Monit2006;12:CR186-90.
[8] Krae R, Bühring M, Hopfenmüller W, Holick MF, Sharma AM. Ultraviolet B and blood pressure. Lancet 1998;352:709-10.
[9] Liu D, Fernandez BO, Hamilton A, Lang NN, Gallagher JM, Newby DE, Feelisch M, Weller RB. UVA irradiation of human skin vasodilates arterial vasculature and lowers blood pressure independently of nitric oxide synthase. J Invest Dermatol. 2014 Jul;134(7):1839-46.
[10] D Liu, BO Fernandez, NN Lang, JM Gallagher, DE Newby, M Feelisch and RB Weller. UVA lowers blood pressure and vasodilates the systemic arterial vasculature by mobilization of cutaneous nitric oxide stores. Photobiology Abstract # 1247 May 2013.
In an impressive mouse study,[1] it was shown that in animals that were exposed to high doses of radiation during a 35-week program, those that were fed a pre-radiation dose of tomato powder or tangerine powder had a higher level of the antioxidant lycopene than mice who were not fed the powders (control group). Lycopene is a potent antioxidant found in tomatoes, tangerines, watermelon and other fruits and vegetables.
Interestingly, the animals that consumed the tangerine powder had higher levels of lycopene than those consuming the tomato powder, but the results were not as impressive. The number of cancerous tumors that developed in the tomato-fed mice was about half the number that developed in the control group. Tomatoes obviously have anti-skin cancer attributes, but remember that lycopene may not be as effective as the whole tomato powder in reducing that disease. Whole foods are nearly always superior to the nutrients extracted from them, as all of the nutrients work in concert to help health whether for mice or men. There may be hundreds of nutrients besides lycopene in tomatoes, all having a positive effect in protecting against cancer. Why just take one nutrient from the tomato and put it in a pill? I’ll tell you why: It is a way to make money. In this case, the researchers discovered that important substances called glycoalkaloids were significantly higher in the skin after the ingestion of tomato powder, and seem to believe that these substances were responsible for the reduced risk of skin cancer.
It has actually been known for some time that some of the best skin protectants are tomatoes. One investigation showed that among individuals who consumed forty grams of tomato paste daily for ten weeks, sunburn-resistance time increased by 40%,[2] and other research demonstrated that eating different tomato-based products correlated to significantly reduced risk of sunburn after exposure to ultraviolet radiation from sunlamps.[3] It is also known that individuals with the lowest intake of alpha-carotene, beta-carotene, cryptoxanthin, lutein, and lycopene (all carotenoid antioxidants found in such vegetables such as carrots and tomato) had a 50% increased risk for melanoma.[4]
There are several other scientific investigations demonstrating that high fruit and vegetable consumption predict a lesser risk of skin cancer.[5],[6],[7], [8]
There are few foods that taste better than a ripe, field-grown tomato. Eat your fill and enjoy some regular, non-burning sun.
[1] Cooperstone JL, Tober KL, Riedl KM, Teegarden MD, Cichon MJ, Francis DM, Schwartz SJ, Oberyszyn TM. Tomatoes protect against development of UV-induced keratinocyte carcinoma via metabolomic alterations. Sci Rep. 2017 Jul 11;7(1):5106.
[2] Stahl W, Heinrich U, Wiseman S, Eichler O, Sies H, Tronnier H. Dietary Tomato Paste Protects against Ultraviolet Light–Induced Erythema in Humans. J Nutr 2001;131:1449-51.
[3] Aust O, Stahl W, Sies H, Tronnier H, Heinrich U. Supplementation with tomato-based products increases lycopene, phytofluene, and phytoene levels in human serum and protects against UV-light-induced erythema. Int J Vitam Nutr Res 2005;75:54-60.
[4] Millen AE, Tucker MA, Hartge P, Halpern A, Elder DE, Guerry D 4th, Holly EA, Sagebiel RW, Potischman N. Diet and melanoma in a case-control study. Cancer Epidemiol Biomarkers Prev 2004;13:1042-51
[5] Afaq F, Katiyar SK. Polyphenols: skin photoprotection and inhibition of photocarcinogenesis.Mini Rev Med Chem. 2011 Dec;11(14):1200-15.
[6] Afaq F, Katiyar SK. Skin photoprotection by natural polyphenols: Anti-inflammatory, anti-oxidant and DNA repair mechanisms. Arch Dermatol Res 2010;302:71.
[7] Stahl W, Heinrich U, Wiseman S, Eichler O, Sies H, Tronnier H. Dietary Tomato Paste Protects against Ultraviolet Light–Induced Erythema in Humans. J Nutr 2001;131:1449-51.
[8] Meyskens FL Jr, Farmer PJ, Anton-Culver H. Diet and melanoma in a case-control study. Cancer Epidemiol Biomarkers Prev 2004;13:1042-51.
 In research on rheumatoid arthritis, involving studies done on nurses, an interesting result emerged.[1] It was found that among nurses 30-55 years of age who were assessed in 1976, and followed until 2008, there was an inverse association between sun exposure and the risk of rheumatoid arthritis. Those who were exposed to the greatest sun exposure had a 21% reduced risk of the disease. However, among nurses 25-42 years of age who were assessed in 1989 and followed until 2008, rheumatoid arthritis was not associated with greater sun exposure.
In research on rheumatoid arthritis, involving studies done on nurses, an interesting result emerged.[1] It was found that among nurses 30-55 years of age who were assessed in 1976, and followed until 2008, there was an inverse association between sun exposure and the risk of rheumatoid arthritis. Those who were exposed to the greatest sun exposure had a 21% reduced risk of the disease. However, among nurses 25-42 years of age who were assessed in 1989 and followed until 2008, rheumatoid arthritis was not associated with greater sun exposure.
The authors of the researchers offered an explanation regarding the disparate results. They felt that the greater use of sunscreen among the younger subjects
may have made the difference.
I agree with that idea. Sunscreen would have decreased the availability of vitamin D production, which may have lead to the lack of a protective effect on rheumatoid arthritis among the younger nurses.
Rheumatoid arthritis is a disease which causes chronic inflammation of the joints, the tissue around the joints and even in certain organs in the body.[2] It is an autoimmune disease such as lupus, multiple sclerosis and seasonal vitamin D declines may trigger it.[3] Vitamin D is an anti-inflammatory hormone and declines in vitamin D levels, of course, are a result of decreasing sun exposure in colder seasons.
Arthritic joints carry another devastating side effect. Hip replacement surgery is often prescribed for arthritic conditions, and those people who go through total-hip-replacement procedures are 4.7 times as likely to have an ischemic stroke, and 4.4 times as likely to have a hemorrhagic stroke in the first two weeks post surgery.[4] Those stroke risks remain elevated for 6-12 weeks. The term “ischemic” means producing a local deficiency of blood supply by obstructing blood flow.
I would be remiss if I did not also mention the transcendent importance of anti-inflammatory nutrition program. Sunlight is important but what you eat is critical. I would suggest that you google “anti-inflammatory diet.” Learn which foods (primarily fruits and vegetables) will help to decrease or prevent the inflammation that leads to RA. In the meanwhile, enjoy some safe, non-burning sunbathing.
[1] Arkema EV, Hart JE, Bertrand KA, Laden F, Grodstein F, Rosner BA, Karlson EW, Costenbader KH. Exposure to ultraviolet-B and risk of developing rheumatoid arthritis among women in the Nurses’ Health Study. Ann Rheum Dis. 2013 Apr;72(4):506-11
[2] Medicinenet.com. Definition of rheumatoid arthritis. http://www.medterms.com/script/main/art.asp?articlekey=5354.
[3] Cutolo M, Paolino S, Sulli A, Smith V, Pizzorni C, Seriolo B. Vitamin D, steroid hormones, and autoimmunity. Ann N Y Acad Sci. 2014 May;1317:39-46.
[4] Lalmohamed A, Vestergaard P, Cooper C, de Boer A, Leufkens HG, van Staa TP, de Vries F. Hip replacement surgery and stroke. Stroke 2012;43(12):3225-9.
A recent sunshine article in the UK online newspaper, The Mail, led with the headline, “Sunshine breaks could mean better mental health.” It then went on to describe how many shift workers, as well as other residents of the UK, are deficient in vitamin D.[1] Quoting from research published in the Journal BMC Public Health,[2] the article stated that about 91% of residents are at least insufficient in vitamin D.
Vitamin D deficiency of that extent is a health crisis, of that there is no doubt. It is also a surety that the way to combat vitamin D deficiency is by taking “sunshine breaks.” However, it is misleading to assume it is vitamin D deficiency that is responsible for the entire problem with mental health and other diseases as they relate to sun exposure. Consider the fact that lack of sunshine deficiency also causes problems beyond vitamin D deficiency. For example, the natural 24-hour cycles, called circadian rhythms, are desynchronized by lack of sunshine in the morning. This causes us to feel out of synch and to be more susceptible to many diseases including cancer.
Remember that sun exposure also leads to the production of serotonin,[3] endorphin,[4] dopamine,[5] and BDNF,[6] all of which have a positive effect on mood and mental health.
Sunshine is vital to mental and physical health, and that health is not due to vitamin D alone. Take a holistic view of the importance of sunshine.
[1] http://www.nwemail.co.uk/news/Sunshine-breaks-could-mean-better-mental-health-88b00574-032c-4467-846c-1eff0514d4e8-ds
[2] Sowah D, Fan X, Dennett L, Hagtvedt R, Straube S. Vitamin D levels and deficiency with different occupations: a systematic review. BMC Public Health. 2017 Jun 22;17(1):519.
[3] Lambert GW, Reid C, Kaye DM, Jennings GL, Esler MD. Effect of sun and season on serotonin turnover in the brain. Lancet. 2002 Dec 7;360(9348):1840-2.
[4] Asta Juzeniene and Johan Moan. Beneficial effects of UV radiation other than via vitamin D production: Dermato-End Holick, M. The UV Advantage 2. Ibooks 2003, New York. Ocrinology 2012;4(2):109–117.
[5] Holick, M. The UV Advantage 2. Ibooks 2003, New York.
[6] Molendijk ML, Haffmans JP, Bus BA, Spinhoven P, Penninx BW, Prickaerts J, Oude Voshaar RC, Elzinga BM. Serum BDNF concentrations show strong seasonal variation and correlations with the amount of ambient sun. PLoS One. 2012;7(11):e48046.
 Sun exposure is crucial to preventing multiple sclerosis (MS), the terrible, debilitating autoimmune disease in which T-cells initiate an inflammatory response against myelin, the protective cover of nerves.[1],[2] This leaves the nerves bare and susceptible to “short circuiting,” a process known as demyelination. This attack prevents proper functioning within the brain and body, which leads to a variety of symptoms like vision changes, muscle spasms, and numbness. These symptoms profoundly decrease the ability to function and destroy the quality of life.
Sun exposure is crucial to preventing multiple sclerosis (MS), the terrible, debilitating autoimmune disease in which T-cells initiate an inflammatory response against myelin, the protective cover of nerves.[1],[2] This leaves the nerves bare and susceptible to “short circuiting,” a process known as demyelination. This attack prevents proper functioning within the brain and body, which leads to a variety of symptoms like vision changes, muscle spasms, and numbness. These symptoms profoundly decrease the ability to function and destroy the quality of life.
We have known for decades that people who live in areas of low sun exposure, such as far-northern or far southern countries, have a far greater risk of contracting MS than those who live in countries closer to the equator. In fact, there is more than 100 times the risk of MS in far northern as in equatorial areas, where sun is intense, and the rate of MS approaches zero.[3],[4],[5]
I ran across an interesting study demonstrating that the age at which the low sun exposure occurs is also a predictive factor in the risk of MS.[6] It showed that in Norway, the amount of sun exposure in the period of life between 16-18 years of age was critical in predicting the disease. Those youngsters who experienced the lowest sun exposure during those ages were 83% more likely to develop MS. The same research showed that in Italy the critical period was between birth and age 5 years, with those receiving the lowest sun exposure being 56% more likely to develop MS.
I spite of incontrovertible research that proves regular, non-burning sun exposure is critical for human health, the sunscare movement continues to promote the idea that we should avoid the sun. The blood is on their hands.
[1] Racke, M. Immunopathogenesis of multiple sclerosis. Ann Indian Acad Neurol. 2009 Oct–Dec; 12(4): 215–220.
[2] Markovic-Plese S, McFarland HF. Immunopathogenesis of the multiple sclerosis lesion. Curr Neurol Neurosci Rep 2001;1:257-62
[3] Alter M, Yamoor M, Harshe M. Multiple sclerosis and nutrition. Arch Neuroll974;31:267-72.
[4] Kurtkze, J. Geography in multiple sclerosis. J Neurol1977;215:1-26.
[5] Hayes CE, Cantorna MT, DeLuca HF. Vitamin D and multiple sclerosis. Proc Soc Exp Biol Med 1997;216:21-27
[6] Bjørnevik K, Riise T, Casetta I, Drulovic J, Granieri E. et al. Sun exposure and multiple sclerosis risk in Norway and Italy: The EnvIMS study. Mult Scler. 2014 Jul;20(8):1042-9.
Sun exposure reduces risk of heart disease. High cholesterol levels are associated with vascular diseases such as heart disease, ischemic stroke and intermittent claudication (an occlusion of the arteries of the legs that leads to pain and disability). The authors of a recent study compared the effects of vitamin D supplementation with sun exposure to determine which was more effective in reducing risk factors.[1] A group of individuals with insufficient serum vitamin D levels was divided into two groups with different experimental protocols: one was treated with sun exposure to the arms and face between 11 AM and 3 PM and the other was treated with 1,000 IU of vitamin D. A third group had “normal” vitamin D levels and served as a control (no treatment group). Total cholesterol levels and its components of cholesterol, HDL and LDL, were also measured to determine the positive (or negative) effects of the two treatment protocols.
The results were enlightening. Both experimental groups had significant increases in vitamin D. However, the results with cholesterol varied. A significant decrease in total cholesterol was noted in the sun exposure group, and HDL and LDL also decreased in the sun-exposure group. However, in the vitamin D-supplement group, a significant increase was noted in in total cholesterol. HDL also increased significantly, and LDL increased non-significantly.
In other words, vitamin D supplementation could actually lead to an increased risk of vascular diseases by raising total cholesterol, whereas sun exposure is protective against those diseases. So the takeaway is that there is no substitute for the sun when it comes to providing some protection against vascular diseases.
There are those people who worry that melanoma risk may be increased by regular sun exposure. However, we have mentioned many time in this blog that melanoma is much more common among those who work indoors than those who work outdoors. It should also be mentioned that vascular diseases kill far more people than skin cancer. Dr. Richard perhaps said it best:
“Sunlight may have beneficial cardiovascular effects, independently of Vitamin D production. Vitamin D could, in these circumstances, act as a marker for sunlight exposure and its postulated beneficial effects. These recent human data show the physiological relevance of photorelaxation. High blood pressure is the leading cause of disability-adjusted life years lost worldwide and as a risk factor underlies 18% of all deaths.” Weller further noted: “The action spectrum of nitrite release shows ultraviolet B is also involved in nitrite reduction to Nitric Oxide, and thus sunlight may be more effective than a pure UVA source.” He concluded: “the prevalence of cardiovascular and cerebrovascular deaths is around 100 times higher than those from skin cancer. Interventions leading to small changes in the incidence of cardiovascular disease are thus of greater benefit to the health of the public even than large changes in skin cancer incidence.”[2]
Safely embrace the sun and your heart, brain and blood vessels will love you for it!
[1] Patwardhan VG, Mughal ZM, Padidela R, Chiplonkar SA, Khadilkar VV, Khadilkar AV. Randomized Control Trial Assessing Impact of Increased Sunlight Exposure versus Vitamin D Supplementation on Lipid Profile in Indian Vitamin D Deficient Men. Indian J Endocrinol Metab. 2017 May-Jun;21(3):393-398.
[2] Weller R. The health benefits of UV radiation exposure through vitamin D production or non-vitamin D
Pathways. Blood pressure and cardiovascular disease. Photochem. Photobiol. Sci. 2016.