Sepsis and septicemia, major killers that associate with sun deprivation. By Marc Sorenson, EdD

Sepsis facts:
Sepsis is an infection of tissues by bacteria, and septicemia is a form of sepsis that infects the blood. Septicemia is a severe and often deadly blood infection. Noxious bacteria attack tissue or blood, and when they die or when their cell walls rupture, they release poison (endotoxin). So, these dying organisms may do more harm than the bacterial attack itself. In addition, the disease accounts for 500,000 emergency-room hospital visits per year in the USA. And, it is followed by a typical stay of 6 to 9 days.[1] As a result, it is one of the worst medical conditions. And, it often results in multiple organ failure and death. There are about 750,000 cases per year, and about 3% of all hospital admissions result in a case of sepsis. Read more.
Sepsis and hospitals
Hospitals are hotbeds of antibiotic-resistant “superbugs” and other infectious agents. In cases of severe sepsis, antibiotics have not improved survival. In fact, antibiotics may produce molecules that exacerbate sepsis.[2] Therefore, the health system must urgently find and implement non-antibiotic solutions to this crisis.
Also, it should be remembered that sunlight is said to be the best disinfectant.[3] The annual cost of care for sepsis is about $17 billion. And, in the case of severe sepsis, antibiotics have not improved survival. In fact, it is especially relevant that antibiotics may produce molecules that exacerbate it.[4] Sepsis is one of the top-ten causes of death and the second leading cause of hospital-associated deaths. So only coronary intensive care units end up having more deaths. In North America, sepsis and its related disorders kill more hospitalized people than heart attacks, colon cancer, breast cancer or AIDS.
Dr. William B. Grant’s research with sepsis and septicemia.
Dr. William Grant hypothesized that vitamin D deficiency, due to inadequate sun exposure, is a risk factor. That is true for both sepsis and septicemia.[5] He points out that septicemia incidence is also highest in winter and lowest in the autumn. Another point is that rates are highest in the Northeast (low sunlight) and lowest in the Southwest (high sunlight).[6] Therefore, all of this leads to the idea that sun deficiency is a major cause this disorder.

Consequently, sun deficiency could play a strong causal role in the disease, since deficiency inhibits the production of cathelicidins. Cathelicidins are antimicrobial peptides which facilitate the destruction of pathogenic germs’ cell walls, leading to their death. In addition, these peptides also help inactivate the endotoxins released as a result of that destruction.[7], [8], [9]
Stay well and thereby avoid hospitals (and sepsis).
Finally, it would be best to avoid hospitals and their superbugs. The formula? Obtain some regular, non-screened, non-burning sunlight around noon when available. Happy sunning! And be sure to read my new book, Embrace the Sun.
[1] http://www.summitmedicalgroup.com/library/adult_care/ac-sepsis_dx/
[2] Mookherjee N, Rehaume LM, Hancock RE. Cathelicidins and functional analogues as antisepsis molecules. Expert Opinions on Therapeutic Targets 2007;11:993-1004
[3]http://sunlightinstitute.org/tag/sepsis/.
[4] Mookherjee N, Rehaume LM, Hancock RE. Cathelicidins and functional analogues as antisepsis molecules. Expert Opinions on Therapeutic Targets 2007;11:993-1004.
[5] Grant, WB. Solar ultraviolet-B irradiance and vitamin D reduce the risk of septicemia. Dermatoendocrinol 2009;1:37-42.
[6] Danai PA, Sinha S, Moss M, Haber MJ, Martin GS. Seasonal variation in the epidemiology of sepsis. Crit Care Med. 2007;35:410–15.
[7] Giacometti A, Cirioni O, Ghiselli R, Mocchegiani F, D’Amato G, Circo R, Orlando F, Skerlavaj B, Silvestri C, Saba V, Zanetti M, Scalise G. Cathelicidin peptide sheep myeloid antimicrobial peptide-29 prevents endotoxin-induced mortality in rat models of septic shock. Am J Respir Crit Care Med 2004;169:187-94.
[8] Giacometti A, Cirioni O, Ghiselli R, Bergnach C, Orlando F, D’Amato G, Mocchegiani F, Silvestri C, Del Prete MS, Skerlavaj B, Saba V, Zanetti M, Scalise G. The antimicrobial peptide BMAP-28 reduces lethality in mouse models of staphylococcal sepsis. Crit Care Med. 2004;32:2485–90.
[9] Cirioni O, Giacometti A, Ghiselli R, Bergnach C, Orlando F, Silvestri C, Mocchegiani F, Licci A, Skerlavaj B, Rocchi M, Saba V, Zanetti M, Scalise G. LL-37 protects rats against lethal sepsis caused by gram-negative bacteria. Antimicrob Agents Chemother. 2006;50:1672–9
Melanoma risk is prevented by sun exposure. Case closed! -By Marc Sorenson, EdD
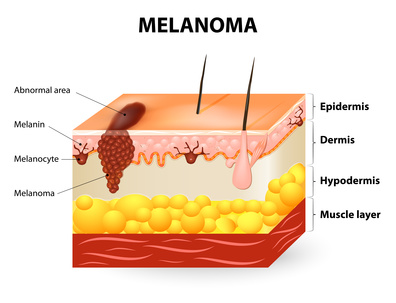
Melanoma risk between persons with high and low vitamin D levels
Melanoma risk is probably the most misunderstood topic in medicine. I recently wrote about the inverse association between vitamin D and melanoma. But I finally decided that my case had insufficient passion and surety. Consequently, I decided to write this addition and provide some new and restated information.
Melanoma risk is directly associated with low levels of vitamin D. That is the conclusion of recent study published in the European Journal of Cancer.[1] The investigators measured the blood vitamin D levels of 137 subjects who had been diagnosed with melanoma. They collected the blood samples at the time of diagnosis of the disease. Another group of 99 healthy subjects served as the control group. The investigators collected the samples of the control group between October and April. The scientists then compared the blood collections of the melanoma group with those of the control group. They then determined whether vitamin D levels had an association with melanoma risk.
The study produced convincing results regarding vitamin D and melanoma risk.
The results were as follows:
- The controls (no melanoma) had vitamin D levels 50% higher than the melanoma group (27.8 ng/ml vs. 18 ng/ml).
- 66.2% of the melanoma group had vitamin D “deficiency,” compared to only 15.2% of the health controls. The scientists defined vitamin D deficiency as being equal to or less than 20 ng/ml. So, the melanoma group had more than four-times the risk of deficiency.
- The scientists defined vitamin D “sufficiency” as being equal to or greater than 30 ng/ml. They found that only 7.4% of melanoma patients were sufficient, compared to 37.4% of healthy controls. Hence, the melanoma group had about one-fifth the likelihood of having sufficient D levels.
More scientific analysis on vitamin D measurements vs. melanoma risk
The scientists then adjusted the data for possible confounding factors such as age, sex and body mass. Then, they performed an analysis that showed the following:
- First of all, a significant inverse association was demonstrated with vitamin D sufficiency versus deficiency. Those who had sufficient levels had only 4% of the melanoma risk when compared to those who were deficient! Hence, this would indicate that those with the lowest vitamin D levels (after adjusting for confounding factors) had 25-times the melanoma risk!
- And, vitamin D insufficiency vs. deficiency was significantly inversely associated with melanoma. Those who were insufficient had a definite advantage over those who were deficient. They had only 13% of the melanoma risk.
Now, let’s get to the most important point about melanoma risk:
In addition, this research proves conclusively that sun deprivation is a major cause of melanoma. Therefore, vitamin D levels are surrogate measurements for sun exposure in nearly every case. And why do I say than this research conclusively proves that sun exposure reduces melanoma risk? Because about 90% of serum vitamin D is produced by sun exposure to the skin.[2] So, the aforementioned research is really research on sun exposure. It indicates that regular sun exposure leads to a profoundly higher vitamin D levels and therefore a profoundly reduced melanoma risk. So, let’s restate the facts about vitamin D, sunlight and melanoma.
- First of all, sunlight exposure to skin produces 90% of the vitamin D levels in the public.
- Secondly, the higher the vitamin D levels, the lower is the risk of melanoma.
- Therefore, high sun exposure reduces melanoma risk.
- Case closed!
Nevertheless, there is more corroborating evidence for the case.
In addition, here are a few more facts indicative of sun exposure’s protective effect against melanoma risk:
- Another supporting fact: 75% of melanomas occur on body areas that are seldom if never exposed to sunlight.[3]
- In addition, sun exposure decreased by 90% since 1935, while melanoma increased by 3,000%.[4]
- Also, in the past four decades, melanoma has increased 400% while sunscreen use also increased 400%.[5]
- Furthermore, sunburn is said to increase melanoma risk. And recent research shows that sunscreen use increases the risk of sunburn from 300-600%.[6]
Could sunlight reduce melanoma through photoproducts beyond vitamin D?
In conclusion: In my new book, Embrace the Sun (coauthored by Dr. William Grant), we note that sun exposure provides more than vitamin D. It also provides other photoproducts such as nitric oxide, serotonin, endorphin, and brain-derived neurotropic factor (BDNF). All of these photoproducts are vital to human health. Could these photoproducts have a positive and protective effect against melanoma risk beyond vitamin D? And, who is to say that the vitamin D produced by sunlight is not superior to that given in pill form?
Finally, this research gives us one more reason to embrace the sun safely without burning. And who would have thought that safe sunlight could be one of the best prophylactics against melanoma risk?
Happy sunning! Do not burn.
The book is available at Amazon: https://www.amazon.com/Embrace-Sun-Marc-B-Sorenson/dp/069207600X
[1] Cattaruzza MS, Pisani D, Fidanza L, Gandini S, Marmo G, Narcisi A, Bartolazzi A, Carlesimo M. 25-Hydroxyvitamin D serum levels and melanoma risk: a case-control study and evidence synthesis of clinical epidemiological studies. Eur J Cancer Prev. 2018 Feb 12. [Epub ahead of print]
[2] Reichrath J. The challenge resulting from positive and negative effects of sun: how much solar UV exposure is appropriate to balance between risks of vitamin D deficiency and skin cancer? Prog Biophys Mol Biol 2006;92(1):9-16
[3] Crombie IK. Distribution of malignant melanoma on the body surface.Br J Cancer. 1981 Jun;43(6):842-9.
[4] Melanoma International Foundation, 2007 Facts about melanoma. Sources: National Cancer Institute 2007 SEER Database, American Cancer Society’s 2007 Facts and Figures, The Skin Cancer Foundation, The American Academy of Dermatology.
[5] Joseph C DiNardo and Craig A Downs. Should We Use Products Containing Chemical UV Absorbing Sunscreen Actives on Children? Clin Dermatol Res J 2019, 4:1.
[6] Kasey L. Morris, PhD; Frank M. Perna, EdD, PhD. Decision Tree Model vs Traditional Measures to Identify Patterns of Sun-Protective Behaviors and Sun Sensitivity Associated With Sunburn. JAMA Dermatol. Published online June 27, 2018.
The great outdoors, sun exposure and health. By Marc Sorenson, EdD.
The great outdoors, because of the sun, is magnificent! The UVB rays have returned to the sunshine in Saint George, Utah, and I have taken full advantage of them, sunbathing daily at midday. But In addition, the great outdoors furnishes so many advantages beyond our life-giving sunlight. Or does it? First of all, sunlight directly effects human health through stimulating the skin to produce photoproducts. Hence, such life-saving products as vitamin D, serotonin, endorphin, nitric oxide, dopamine and brain-derived neurotropic factor (BDNF) are increased. Furthermore, none of the other attributes of the great outdoors, such as the greenery and animal life, would be possible without the sun.
Recent research on the great outdoors
A recent study analyzed most of the health research that has been done on the benefits of the great outdoors.[1] The title of the research was: The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. It was an analysis of 143 studies. The researchers showed impressive results from spending time in the great outdoors, especially the green great outdoors, known as greenspace.
Health expectations derived from enjoying the great outdoors:
- A reduction in diastolic blood pressure
- Decreased preterm birth risk
- A reduction in type two diabetes risk
- Decreased all-cause mortality
- A reduced risk of small size for gestational age
- Decreased risk of cardiovascular mortality
- An increased incidence of self-reported health
- Decreased incidence of stroke, hypertension, dyslipidaemia, asthma, and coronary heart disease
- Decreased risk of neurological and cancer-related outcomes and respiratory mortality
- Reduced negative emotions and fatigue
In addition, the authors noted that groups who exercised in the great outdoors had better health results. Indoor exercisers had results that were less than the outdoor exercisers. Thus, the great outdoors groups had significantly improved blood pressure, heart rate, fat percentage, BMI, cholesterol, depression and physical functioning.
While being in the great outdoors is exceptionally important to health, so is sunlight exposure. It is especially relevant that benefits enumerated for outdoor exposure are identical to those for regular, non-burning sun exposure. My new book, Embrace the Sun, delineates those healthful effects. It also cites research that indicates sun deprivation is as dangerous a cigarette smoking.[1]
Summary: Combine sun exposure with the great outdoors.
I opine that both safe sun exposure and exposure to the
great outdoors, are vital to health. So, it is best not to neglect either. Happy sunning!
[1] Lindqvist PG, Epstein E, Nielsen K, Landin-Olsson M, Ingvar C, Olsson H. Avoidance of sun exposure as a risk factor for major causes of death: a competing risk analysis of the Melanoma in Southern Sweden cohort. J Intern Med. 2016 Oct;280(4):375-87.
[1] Caoimhe Twohig-Bennett, Andy Jones. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environmental Research 166 (2018) 628–637.
[2] Lindqvist PG, Epstein E, Nielsen K, Landin-Olsson M, Ingvar C, Olsson H. Avoidance of sun exposure as a risk factor for major causes of death: a competing risk analysis of the Melanoma in Southern Sweden cohort. J Intern Med. 2016 Oct;280(4):375-87.
 Parkinson’s disease prevented by sunlight. By Marc Sorenson, EdD
Parkinson’s disease prevented by sunlight. By Marc Sorenson, EdD
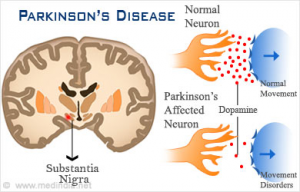 Parkinson’s disease is a common nerve disease, and it is caused by deterioration of brain cells that produce dopamine. It is characterized by tremors, muscle rigidity, shuffling gait, slow speech, and a mask-like facial expression. In addition, even simple movements may become difficult for the person suffering from the disease. And, the disease is a killer that takes the lives of 14,593 per year.[1] So how do we prevent it? In this blog, I will explain the disease, show what the research says about sunlight, and make recommendations for prevention.
Parkinson’s disease is a common nerve disease, and it is caused by deterioration of brain cells that produce dopamine. It is characterized by tremors, muscle rigidity, shuffling gait, slow speech, and a mask-like facial expression. In addition, even simple movements may become difficult for the person suffering from the disease. And, the disease is a killer that takes the lives of 14,593 per year.[1] So how do we prevent it? In this blog, I will explain the disease, show what the research says about sunlight, and make recommendations for prevention.
Research points out that Sun exposure is the key to prevention of Parkinson’s disease.
Several studies have shown that there is a close association between sunlight exposure, blood 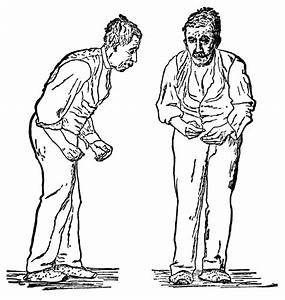 vitamin D levels and Parkinson’s. First of all, one paper showed that when vitamin D levels are low, there is a tripling of the risk.[2] Another study from China demonstrated that persons with highest levels of blood vitamin D had a 48% decrease in risk. And, that same research demonstrated that those receiving the greatest sun exposure had about a 47% decrease in risk.[3] So, based on those findings, one might think that vitamin D supplements could prevent the disease. Yet, that thought is erroneous. Sun exposure is the direct key for preventing this debilitating disease.
vitamin D levels and Parkinson’s. First of all, one paper showed that when vitamin D levels are low, there is a tripling of the risk.[2] Another study from China demonstrated that persons with highest levels of blood vitamin D had a 48% decrease in risk. And, that same research demonstrated that those receiving the greatest sun exposure had about a 47% decrease in risk.[3] So, based on those findings, one might think that vitamin D supplements could prevent the disease. Yet, that thought is erroneous. Sun exposure is the direct key for preventing this debilitating disease.
Vitamin D supplements do not stop Parkinson’s, so how can that be?
Recent research, a systematic review and meta-analysis, is most noteworthy. And it explains this interesting paradox.[4] It showed that sun exposure was significantly associated with a reduced risk of Parkinson’s. Especially relevant is the fact that those persons with plenty of sun exposure had only 1/50 the risk of Parkinson’s. That is an astounding figure! However, although vitamin D supplements were effective in raising vitamin D levels, they had no significant benefits for Parkinson’s disease.
Vitamin D and sun exposure are not the same.
While sun exposure and supplements both raise vitamin D levels, supplements are no help to Parkinson’s sufferers. Hence, we must look beyond vitamin D for an answer. Sun exposure leads to the production of vitamin D, but it also leads to the production of dopamine. Dopamine, as previously mentioned, is a vital chemical for the brain as regards Parkinson’s. Vitamin D is a marvelous, vital photoproduct and is due to sun exposure. It is vital for human health. However, it appears that vitamin D does nothing for Parkinson’s. Most of all, we must remember that sun exposure produces many essential photoproducts beyond vitamin D.
Vitamin D blood levels, in the case of Parkinson’s and some other diseases, are simply surrogate measurements of sun exposure. We simply cannot substitute a vitamin D pill for sun exposure and expect to reap all the benefits of sunlight. The “holistic” sun will never be supplanted by a capsule. The sun stimulates the production of vitamin D, dopamine, nitric oxide, serotonin, endorphins, brain-derived neurotropic factor (BDNF) and other photoproducts. And, all of these photoproducts play their roles in human health. For some diseases, vitamin D is vital for prevention. In others such as Parkinson’s, it is just along for the ride.
The takeaway regarding sun exposure and Parkinson’s.
To help prevent this disease, be sure to obtain plenty of non-burning sunlight. And In lieu of that, when there is no sunlight available, use a low-pressure sunbed (tanning bed) in a salon. Always remember not to burn. For more information, read my new book, Embrace the Sun, available at Amazon: https://www.amazon.com/Embrace-Sun-Marc-B-Sorenson/dp/069207600X 
Happy sunning!
[1] ttps://www.rightdiagnosis.com/p/parkinsons_disease/deaths.htm
[2] Knekt P, Kilkkinen A, Rissanen H, Marniemi J, Sääksjärvi K, Heliövaara M. Serum vitamin D and the risk of Parkinson disease. Arch Neurol. 2010 Jul;67(7):808-11.
[3] Wang J, Yang D, Yu Y, Shao G. Wang Q. Vitamin D and Sunlight Exposure in Newly-Diagnosed Parkinson’s Disease. Nutrients 2016;8:142.
[4] Zhou Z, Zhou R, Zhang Z, Li K. The Association between Vitamin D Status, Vitamin D Supplementation, Sunlight Exposure, and Parkinson’s disease: A Systematic Review and Meta-Analysis. Med Sci Monit. 2019 Jan 23;25:666-674.
 Sunlight improves public health. By Marc Sorenson, EdD.
Sunlight improves public health. By Marc Sorenson, EdD.
An excellent new paper by Dr. Hoel and Dr. de Gruijl is titled “Sun Exposure Public Health Directives.” It decries the vilification of sunlight and suggests people return to its healthful rays.[1] https://www.mdpi.com/1660-4601/15/12/2794/htm
So is dermatology awakening to the truth about sunlight?
And one of the authors, Dr. de Gruijl, works at a dermatology department in the Netherlands. He is also a photobiologist and melanoma skin cancer research specialist. It seems like the dermatology world is returning to common sense, since other dermatologists have lately suggested more sunlight exposure. And well they should suggest more sunlight! Sunlight can save millions of lives, yet much of the population is dying in the dark due to misinformation. Many dermatologists consider sunlight exposure to be a killer, and thus frighten their patients away from sun exposure. Why? Because they are fearful of skin damage from sunlight, something they need not fear if they advise their patients properly.
Sunlight and skin cancer: the truth
One of my pet peeves is the statement that “sunlight causes cancer.” First of all, there are about 18 major cancers that are reduced by sunlight. And in addition, there are also myriad non-cancer maladies that are reduced or eliminated by safe sun exposure. These disorders run the gamut from arthritis and heart disease to psoriasis, erectile dysfunction and osteoporosis.[2] Secondly, not even skin cancer is caused by sun exposure unless people burn themselves. Therefore, it is a lack of both caution and common sense that leads to skin damage. The authors state that the public has been taught that health benefits of sun exposure are limited to bone health. That is another egregious error (italics mine).
The aforementioned paper reads almost like a synopsis of Embrace the Sun, the book by Marc Sorenson and William Grant,
Here are the major points on sunlight that make the research in the paper so compelling:
- There is a public health message that “overexposure” to the sun causes skin cancer. Nevertheless, those who promote this message do not define overexposure. Therefore, due to the lack of a definition, the public is led to believe that sun exposure is an enemy. In addition, the public is not educated regarding the detriments of “sun avoidance,” or should we say “underexposure.” Due to this omission, the public is exposed to disability, destruction and death (italics mine).
Sunlight deprivation: the staggering cost to human health
Consequently, in Embrace the Sun, we calculated the number of deaths due to diseases associated with high sunlight exposure. And, we then calculated the number of deaths due to diseases associated with sunlight deprivation. As a result, we determined that approximately 1,684,677 yearly deaths are caused by diseases associated with sunlight deprivation. Also, there were about 5125 deaths from diseases associated with high sunlight exposure, producing a ratio of approximately 328.7:1. This is most noteworthy! 328 deaths were associated with diseases of sun deprivation for each death associated with diseases of sun exposure. So, what do you think?
So, is sunlight avoidance risk free?
- Furthermore, the paper states that people believe sun avoidance is risk free. That is a colossal error as previously stated,
- Another mistake is to believe vitamin D supplements are an adequate substitute for sunlight. That is simply not so. Sun exposure causes the production of serotonin, nitric oxide, endorphin, brain-derived neurotropic factor (BDNF), dopamine and urocanic acid. All of these substances are vital for human health and wellbeing.
- Another important point stated by the authors is as follows: “This public health message is potentially causing significant harm to public health and should be changed immediately.” And, based on the analysis from Embrace the Sun, mentioned above, that should be an easy conclusion.
Is there an inverse association between sunlight and melanoma?
- The authors also state that melanoma risk is reduced by non-burning sun exposure. And only severe sunburns increase risk. In addition, they mention that melanoma in the U.S. has steadily increased at an annual rate of 3–4%. There was 1 case per 100,000 in 1935, when accurate records were established. Yet, there were 25.8 cases per 100,000 in 2015. [That is about a 2,600% increase!]
Our analysis of melanoma in Embrace the Sun was almost identical. It showed a 3,000% increase in melanoma risk accompanied by a 90% decrease in sunlight exposure from 1935 to 2015. And, Sunscreen use also increased dramatically during that period, meaning that more sunscreen use is associated with greater melanoma risk.
And should we use sunscreens to reduce sunlight damage?
The answer to that question is “of course not.”
I was surprised that nothing was said about sunscreens, while I was considering the authors’ comment on severe sunburns, Why? Because recent research has shown that persons who use sunscreens have 4-6 times greater risk of sunburn.[3] In addition, the same research showed that the greatest protection against burning was to seek shade or cover up. Imagine that! Also, a recent meta-analysis showed that sunscreen use made absolutely no difference in the risk of skin cancer.[4].
- The authors also make it clear that the common assertion—that tanned skin affords insignificant protection against sunburn—is not correct.
- In conclusion, the commentary made this statement: “All persons in the world regardless of skin color or latitude of residence, other than those with extraordinary sensitivity to sunlight, should get enough sun exposure to maintain a serum 25(OH)D level well over 20 ng/mL (desirably at 30–60 ng/mL) while taking care to avoid sunburn.
I agree and would like to reiterate that vitamin D supplements are not an adequate substitute for sunlight. Consequently, these measurements should be used only among those who do not take supplements. That is, if we expect to really measure sunlight exposure.
Embrace the Sun is available here. 
Happy sunning!
[1] Hoel D, de Gruijl, F. Sun Exposure Public Health Directives. Int. J. Environ. Res. Public Health 2018;15:2794
[2] Sorenson, Marc, Grant, WB. Embrace the Sun. Sorenson, Publisher 2018. Available at Amazon.
[3] Kasey L. Morris, PhD; Frank M. Perna, EdD, PhD. Decision Tree Model vs Traditional Measures to Identify Patterns of Sun-Protective Behaviors and Sun Sensitivity Associated With Sunburn. JAMA Dermatol. Published online June 27, 2018.
[4] Elizabet saes da SILVA, Roberto TAVARES, Felipe da silva PAULITSCH, Linjie ZHANG. Eur J Dermatol 2018; 28(2): 186-201.
Obesity in children: Caused by pregnant mom’s sun deprivation? By Marc Sorenson, EdD. 
Obesity in children is linked closely to maternal vitamin D status in pregnancy.[1] And is anyone surprised about this? First of all, everyone should know that vitamin D deficiency is caused by inadequate sun exposure. So, if high vitamin D is associated with less weight, it is because of high sun exposure. That is of course, unless the research involves vitamin D supplementation. Because sunlight produces nitric oxide, endorphin, serotonin, dopamine and other chemicals, only research can determine if vitamin D is protective. Therefore, a supplementation study would be required.
What did the research show regarding obesity?
It seems like sun exposure, which produces all of the photoproducts, would always be the best way to prevent weight gain. Most noteworthy, however, is that we are discussing only the sun deprivation aspects of obesity. That is because being overweight is primarily due to 1. eating junk food and 2. not staying active. This blog, however, deals only with extra weight due to sun deprivation.
So what did this obesity study show? To perform the research, pregnant women were first of all measured for vitamin D levels before birth. In addition, their newborns were followed for 4-6 years and then compared for obesity levels. In conclusion, those whose mothers had the lowest vitamin D levels had children with the greatest obesity problems.
So, we still don’t know if vitamin D was the protective photoproduct against obesity in children. Because of that lack of surety, let’s visit some research on sunlight and obesity.
In addition to the aforementioned research, another scientific paper “sheds more light” on the subject of obesity.[2]
This research was conducted on mice with shaved backs, because the applied light needed to be unimpeded by hair. Also, a second part of the experiment was to put them on a high-fat diet. Finally, they were exposed to non-burning ultraviolet radiation (UVR) during a three-month period. (UVR is the same light they would receive from sunlight). The mice, because of the high-fat diet, would have been expected to gain weight rapidly. But with UVR, the weight gain was consequently (and impressively) reduced. As a result of the treatment the mice achieved 30-40% less weight gain. That is, compared to the expected weight gain.
Blue light for reduced obesity?
Furthermore, a study published in 2017 showed that the blue-light spectrum of sunlight can cause subcutaneous fat to decrease.[3] In other words, it can cause obesity to diminish, much as good nutrition would also cause it to decrease. Thus, the action of sunlight may help one to prevent obesity or even to create slimness. Consequently, blue light from the sun may be a preventer of obesity, and an adjunct to good nutrition and exercise.
Is obesity reduced by morning light?
So—here we have another benefit of sun exposure—morning sun specifically! A recent study from Northwestern Medicine demonstrates that timing and intensity of light correlate with body mass index (BMI).[4] So to understand the research we need to understand BMI. BMI is a numerical computation comparing height and weight. And it is a commonly used method to assess obesity or the lack thereof. So a high BMI usually means a person is obese or at least approaching obesity. Optimal BMI is 18-25. Below 18 is considered underweight, above 25 is overweight, 30 is obese and 40 and above is morbidly obese.
So does sun exposure influence BMI? Is obesity reduced?
This study showed, first of all, that exposure to bright morning light was directly related to BMI. After adjusting for confounders, it was determined that very early exposure to morning light correlated remarkably to lower BMI. Opposite to what one might expect, when light intensity was equal at different times of the day, results were identical. Consequently, those who received the earliest bright light had lower BMI. Furthermore, for each hour later in the day when light exposure occurred, BMI increased by 1.3 units. This fact is exceptionally important, since a person who has a BMI of 25 (upper ideal range) could approach 30 (obesity). And that would be due to the habit of later sun exposure (10:00 AM rather than 6:00 AM).
Does vitamin D supplementation help prevent obesity?
Another scientific paper “sheds more light” on the subject of obesity.[5] This research was conducted on mice with shaved backs that were placed on a high-fat diet and then exposed to non-burning ultraviolet radiation (UVR) during a three-month experiment. The mice, without the benefit of UVR, would have been expected to gain weight rapidly on that diet, but when they were exposed to UVR, the weight gain was impressively reduced. The UVR treatment achieved a 30-40% reduction in weight gain, compared to the expected weight gain with the high-fat diet.
Interestingly, when vitamin D supplementation was used, it did not help, and actually stopped the positive effects of UVR treatment.
In conclusion, the pandemic of obesity may be exacerbated by sun deprivation. And, it may be due to something other than low vitamin D. Expectant mothers and their children should always obtain plenty of non-burning sun exposure. So should most other members of the human race. Happy sunning! 
Also see: http://sunlightinstitute.org/sun-exposure-reduces-obesity-vitamin-d-not
Read My book, Embrace the Sun, available at
Time limit is exhausted. Please reload CAPTCHA.
[1] V. Daraki T. Roumeliotaki G. Chalkiadaki M. Katrinaki M. Karachaliou V. Leventakou M. Vafeiadi K. Sarri M. Vassilaki S. Papavasiliou M. Kogevinas L. Chatzi. Low maternal vitamin D status in pregnancy increases the risk of childhood obesity
[2] Geldenhuys S, Hart PH, Endersby R, Jacoby P, Feelisch M, Weller RB, Matthews V, Gorman S. Ultraviolet radiation suppresses obesity and symptoms of metabolic syndrome independently of vitamin D in mice fed a high-fat diet. Diabetes. 2014 Nov;63(11):3759-69
[3] Ondrusova K, Fatehi M, Barr A, Czarnecka Z, Long W, K Suzuki K, Campbell S, Philippaert K, Hubert M, Tredget E, Kwan P, Touret N, M Wabitsch M, Lee K, Peter E. Light P. Subcutaneous white adipocytes express a light sensitive signaling pathway mediated via a melanopsin/TRPC channel axis. Scientific Reports 2017 November 27;7:16332
[4] Reid KJ, Santostasi G, Baron KG, Wilson J, Kang J, Zee PC. Timing and intensity of light correlate with body weight in adults. PLoS One 2014;2;9(4)
[5] Geldenhuys S, Hart PH, Endersby R, Jacoby P, Feelisch M, Weller RB, Matthews V, Gorman S. Ultraviolet radiation suppresses obesity and symptoms of metabolic syndrome independently of vitamin D in mice fed a high-fat diet. Diabetes. 2014 Nov;63(11):3759-69
Vitamin D levels: sufficient for winter? By Marc Sorenson, EdD
 Vitamin D levels and sunshine are exceptionally important to human health, and therefore we should be aware of vitamin D science. The Vitamin D Society of Canada is always at the forefront of the research on vitamin D levels and sunlight. And, they deliver press releases to keep people from Canada (and the world) apprised of new and important findings. Hence, I would like to comment on the salient points of their latest release. As I do so, it is especially relevant to note that vitamin D levels are surrogate measures for sun exposure.
Vitamin D levels and sunshine are exceptionally important to human health, and therefore we should be aware of vitamin D science. The Vitamin D Society of Canada is always at the forefront of the research on vitamin D levels and sunlight. And, they deliver press releases to keep people from Canada (and the world) apprised of new and important findings. Hence, I would like to comment on the salient points of their latest release. As I do so, it is especially relevant to note that vitamin D levels are surrogate measures for sun exposure.
The relationship of vitamin D to sun exposure
Ninety percent of vitamin D levels in the blood is due to sun exposure.[1] The UVB portion of sunlight stimulates vitamin D production in skin. Therefore, a UVB light source, which produces vitamin D levels, is the best source in winter. Remember also that the press release information is true for the world, not just Canada.
Salient points about vitamin D levels and sunlight: breast cancer
- First of all, consider a breast-cancer study published in the scientific journal, Plos One.[2] It showed that women with the highest vitamin D levels had a reduced breast-cancer risk. Most noteworthy, women with levels > 60 ng/ml had 82% reduced risk, compared to those with levels < 20 ng/ml. Furthermore, there was a dose-response decrease. For each increase in vitamin D levels, there was a concomitant decrease is breast-cancer risk.
Vitamin D levels and Breast Cancer
- Since we mentioned that vitamin D is produced by sun exposure, we should mention an Iranian sunlight-breast cancer study. In Iran, among women who totally avoid sun exposure, there is a 10-fold increase breast cancer risk.[3] That is an especially relevant fact for women who believe they should avoid the sun! And remember, melanoma is also reduced in those who are regularly exposed to sunlight.[4]
Another Vitamin D levels- and sunlight-deficiency cancer
- It seems like if breast cancer is reduced by high vitamin D levels, the same relationship could exist for other cancers. Hence, the press release mentioned colorectal cancer as the second disease associated to low vitamin D levels or low sun exposure. And, it mentioned another important piece of research.[5] Participants with vitamin D levels below 12 ng/ml had a 31% higher risk of colorectal cancer. Those with levels above 30 ng/ml had a 27% reduced risk.
Other disorders associated with vitamin D levels
In addition, the press release mentions four other disorders where higher vitamin D levels reduce risk or improve the condition. The disorders: diabetes (81% reduced risk), multiple sclerosis (45% reduced risk), preterm birth (62% reduced risk) and poor cognitive function. As to cognitive function, those who spent the most time outdoors with the least sun protection, had better cognitive function.
Finally, this is an excellent press release regarding vitamin D levels and sunlight. I strongly suggest you read it. http://www.vitamindsociety.org/press_release.php?id=60 Also, see the previous blog regarding the vitamin D Society and vitamin D levels: http://sunlightinstitute.org/vitamin-d-canada-warning/
Vitamin D and sunlight are sine qua nons for health, and so are proper nutritional habits. Happy health! Be sure to read my book, Embrace the Sun, available at Amazon. 
[1] Reichrath J. The challenge resulting from positive and negative effects of sun: how much solar UV exposure is appropriate to balance between risks of vitamin D deficiency and skin cancer? Prog Biophys Mol Biol 2006;92(1):9-16
[2] McDonnell SL, Baggerly CA, French CB, Baggerly LL, Garland CF, Gorham ED, Hollis BW, Trump DL, Lappe JM. Breast cancer risk markedly lower with serum 25-hydroxyvitamin D concentrations ≥60 vs <20 ng/ml (150 vs 50 nmol/L): Pooled analysis of two randomized trials and a prospective cohort. PLoS One. 2018 Jun 15;13(6).
[3] Bidgoli SA, Azarshab H. Role of vitamin D deficiency and lack of sun exposure in the incidence of premenopausal breast cancer: a case control study in Sabzevar, Iran. Asian Pac J Cancer Prev. 2014;15(8):3391-6.
[4] Vågero D, Ringbäck G, Kiviranta H. Melanoma and other tumors of the skin among office, other indoor and outdoor workers in Sweden 1961–1979. Brit J Cancer 1986;53:507–12.
[5] McCullough ML, Zoltick ES, Weinstein SJ, Fedirko V, Wang M, et al. Circulating Vitamin D and Colorectal Cancer Risk: An International Pooling Project of 17 Cohorts. J Natl Cancer Inst. 2018 Jun 14.
An infant breakthrough! Our babies need sunlight! By Marc Sorenson, EdD
An infant may return to the sun due to exciting new research from Australia.[1] The researchers surmised that vitamin D deficiency might explain the high rates of infant allergic diseases. They specifically measured infant eczema. Eczema and other allergic diseases are common in areas of industrialization and high latitudes. Thus, eczema could indicate low vitamin D levels. The researchers made this statement: “Suboptimal vitamin D levels during critical periods of immune development have emerged as an explanation for higher rates of allergic diseases associated with industrialization and residing at higher latitudes.” That seems like wisdom, yet, as you’ll see, they turned out to be wrong.
The infant study: UV light or vitamin D?
So, the researchers set out to determine the effects of early-life vitamin D supplementation on infant allergy prevention. In addition to supplementation, they also outfitted some infants with a dosimeter to also measure UV exposure. This group was compared to a placebo group. In addition, each infant was assessed from birth until age six months. This was done because about 90% of vitamin D is produced by sun exposure to the skin. Vitamin D is an important photoproduct of sunlight. And I opine that sun exposure is of much greater importance. Why? Because sun exposure and its UV light lead to the production of many essential photoproducts beyond vitamin D. Also, a high vitamin D level may simply be a surrogate measurement for sun exposure in some cases. Consequently, other photoproducts such as nitric oxide, serotonin, endorphins, dopamine, BDNF and many others may be the health givers. (For a list of more photoproducts, see my last blog, called Holistic Sun). An infant may need all that the sun can provide, including vitamin D.
The results for infant eczema risk
The results were surprising to the researchers but not to me, based on the facts stated in the above paragraph. So, infant vitamin D levels were greater for the supplemented group than the placebo group.at three and six months, That seems like an expected outcome. Most noteworthy, however, was that there was no difference in eczema incidence between infant groups. And also especially relevant was the fact that those who showed the most UV (sun) exposure had the least risk. In addition, the children with eczema had only a bit over half the UV exposure. Vitamin D simply made no difference to eczema.
The researchers’ conclusion regarding infant eczema
Therefore, the researchers wrote the following: “This study is the first to demonstrate an association between greater direct UV light exposures in early infancy with lower incidence of eczema and pro inflammatory immune markers by 6 months of age. Our findings indicate that UV light exposure appears more beneficial than vitamin D supplementation as an allergy prevention strategy in early life.”
In conclusion, UV exposure from sunlight, tanning lamps or tanning beds is far more important that vitamin D per se. And sun exposure also produces vitamin D in the way God (or nature if you prefer), intended. Why should we accept one pill containing vitamin D, when we can obtain the entire package of photoproducts with UV-containing sunlight? For more information on sunlight, eczema and psoriasis, read my new book, Embrace the Sun, Available at Amazon. Also read my previous blog, Holistic Sun.
[1] Rueter K, Jones AP, Siafarikas A, Lim EM, Bear N, Noakes PS, Prescott SL, Palmer DJ. Direct infant UV light exposure is associated with eczema and immune development. J Allergy Clin Immunol. 2018 Oct 15. [Epub ahead of print]
 First of all, low-back pain is pandemic in much of the world. And, it is especially common in countries where most women wear clothing that prevents sun exposure to the skin.[1] One of the first studies to show an association between LBP and reduced sun exposure was done in England:[2] Northerners were 3-4 times as likely to suffer low-back pain as southerners. Of course, we know that there is less sunshine in the north.
First of all, low-back pain is pandemic in much of the world. And, it is especially common in countries where most women wear clothing that prevents sun exposure to the skin.[1] One of the first studies to show an association between LBP and reduced sun exposure was done in England:[2] Northerners were 3-4 times as likely to suffer low-back pain as southerners. Of course, we know that there is less sunshine in the north.
Other low-back pain research shows similar results based on latitudes.
Hence, it is no surprise that research done in Southeast Asian countries shows an equally impressive result for sun exposure. Low-back pain increases from southern to northern latitudes, starting at 5º North (Malaysia – 8.8% low-back pain rate), continuing to 23º N (10.2% low-back pain rate), then 32º N (13%), and finally to 40º N (Beijing — 15.8%).[3] Furthermore, another study by showed that vitamin D deficiency was common among those suffering from low-back pain. It was three-times more common than among those who did not suffer from low-back pain.[4] The researchers stated, “The major determinant of hypovitaminosis D in our patients is limited sun exposure.”
Low-back pain research from Saudi Arabia and Pakistan
In addition, similar findings have been reported in Saudi Arabia[5] and Pakistan.[6] Researchers did a study on undergraduates in those areas. They researchers wanted to assess the students awareness regarding vitamin D deficiency associated with lack of sun exposure. These students often suffered from fatigue and muscular pain. Researchers concluded that many of them were acquainted with vitamin D deficiency, and some used a supplement. However, the investigators seemed to feel that supplements were not sufficient. They believed that sun exposure was the best method to maximize vitamin D levels.
In conclusion, they stated that the role of the sun, and the proper time and duration of exposure, could not be ignored. That is, if the students were to help effect a healthy and active society. Furthermore, they also indicated that since these students would be medical care givers in the future, their habits should be similar to the habits they intended to recommend to their future patients.
My conclusion about sun exposure and low-back pain.
In conclusion, it appears that sunlight, whether or not accompanied by vitamin D production, is effective for relief. Try a few minutes of non-burning sun exposure daily to ease the low-back pain. Remember how vital regular, non-burning sun exposure is for human health. For more information, read my new book, Embrace the Sun, available at Amazon. https://www.amazon.com/Embrace-Sun-Marc-B-Sorenson/dp/069207600X/ref=sr_1_1?ie=UTF8&qid=1534654532&sr=8-1&keywords=embrace+the+sun+sorenson
[1] Lotfi A1, Abdel-Nasser AM, Hamdy A, Omran AA, El-Rehany MA. Hypovitaminosis D in female patients with chronic low back pain. Clin Rheumatol. 2007 Nov;26(11):1895-901
[2] Walsh K, Cruddas M, Coggon D. Low back pain in eight areas of Britain. J Epidemiol Community Health. 1992 Jun;46(3):227-30.
[3] Zeng QY, Chen R, Xiao ZY, Huang SB, Liu Y, Xu JC, Chen SL, Darmawan J, Couchman KG, Wigley RD, Muirden KD. Low prevalence of knee and back pain in southeast China; the Shantou COPCORD study. J Rheumatol. 2004 Dec;31(12):2439-43.
[4] Lotfi A, Abdel-Nasser AM, Hamdy A, Omran AA, El-Rehany MA. Hypovitaminosis D in female patients with chronic low back pain. Clin Rheumatol. 2007 Nov;26(11):1895-901
[5] Al Faraj S, Al Mutairi K. Vitamin D deficiency and chronic low back pain in Saudi Arabia. Spine (Phila Pa 1976). 2003 15;28(2):177-9.
[6] Qureshi AZ, Zia Z, Gitay MN, Khan MU, Khan MS. Attitude of future healthcare provider towards vitamin D significance in relation to sun exposure. Saudi Pharm J. 2015 Oct;23(5):523-527.